Child deaths with persistent neglected experiences from medico-legal documents in Japan
Abstract
Background
Few studies have examined the actual conditions of fatal neglect in Japan. The aims of this study were to investigate persistent neglect among child fatalities using medico-legal documents, and to describe the characteristics of the socio-familial background and biological data.
Methods
The current study analyzed the documents of all postmortem external examinations and autopsies in children <2 years old carried out in one prefecture in Japan from 2006 to 2011. After examining 59 autopsy cases using modified the Maltreatment Classification System, we identified six children who experienced persistent neglect as study samples.
Results
Three children were found in unsanitary rooms and one was left alone inside a car. In two cases, age of mother at delivery was <21 years old. Three victims had 1 year older sibling. With regard to history of use of health services, three mothers missed some prenatal care visits, and two refused to receive neonatal home visits. With regard to biological data the average weight Z score of six children was −2.22 after being adjusted to average weight for age (in months) and sex. Three children had acute or chronic undernutrition. Three victims had thymic involution considered as being due to chronic child maltreatment.
Conclusions
The present collaboration between public health and legal medicine has enabled investigation of the background and biological impact of experiences of persistent neglect. A multidisciplinary system of evaluating child death is needed to identify preventable factors in order to intervene in the case of neglected children in a timely manner.
The number of child maltreatment reports to the Child Guidance Center has drastically increased every year in Japan. Reported cases increased by more than fivefold in 2012 from 1999, prior to the Child Abuse Prevention Act being enforced in 2000.1, 2 The proportion of neglect among reported child maltreatment was 28.9%, which was much less than that reported in the USA (78.3%).2, 3 The proportion of fatalities due to neglect had the same tendency: 27% in Japan and 69.9% in the USA among total deaths due to child maltreatment.3, 4
The reason for this discrepancy may be because it is not possible to assess fatal child maltreatment sufficiently, especially neglect cases in Japan. The national annual report on fatal child maltreatment selected subjects from death cases reported in newspapers, or cases that municipal authorities could recognize as death due to child maltreatment. Therefore, it is possible that some subjects were missed due to being unidentified as child maltreatment, not reported, and not examined adequately.
In addition to the insufficient reporting system, the number of studies on fatal child neglect is also limited in Japan. Although neglect is difficult to define and measure,5 to our knowledge only seven articles were available from PubMed (by searching with “child neglect” and “autopsy” and “Japan”);6-12 and three articles from Igaku Chuou Zasshi, the Japanese database for medical articles (by searching with “child neglect” and “autopsy” and “death” in Japanese6, 13 and by hand-searching14). The majority were case reports, and there was neither systematic evaluation nor classification of child fatal neglect so far.
A previous study conducted by Welch and Bonner found that children <2 years old, the youngest children in the family, and male infants had a higher risk of fatal child neglect.15 Use of a holistic view of child neglect and intervention at an early stage may be necessary to reduce the risk factors of neglect and to prevent the worst outcome (death).
An innovative approach to accessing children's death reports could help to identify preventive factors. Every unexpected death notified to police is criminally investigated, and this includes postmortem external examination of corpses and autopsy. Medico-legal documents are a potential source of details of child maltreatment that have not appeared in the previous national reports. The aims of this study were to investigate persistent neglect among child fatalities using medico-legal documents, and to describe characteristics of the socio-familial background and biological data.
Methods
Defining persistent child neglect
There are several classifications of types of child maltreatment, such as the Child Protection Services (CPS) classification, National Incidence Study (NIS) maltreatment coding system, and Modified Maltreatment Classification System (MMCS).16 CPS reports are likely to describe only a primary or single issue, but MMCS assesses multiple subtype co-occurrence. Although NIS is used to examine incidence of child maltreatment nationwide including both CPS records and non-CPS records, the coding system of MMCS provides a severity weight of caregiver behavior.17 Therefore, we chose MMCS operationally to define neglect experiences of children and to describe inadequate care before their deaths in the current study. MMCS includes two major types of neglect: “failure to provide” and “lack of supervision”.5 There are five subtypes of failure to provide and three subtypes of lack of supervision. The details of the MMCS coding mechanisms are available from the website.18 According to MMCS, all documents on children <2 years old were examined to determine whether any subtypes of neglect existed. A child who had at least one subtype was defined as having an experience of neglect in the present study.
In addition, the present study focused on “persistent” neglect experiences. According to guidelines for the safeguarding of children in the UK “Working together to safeguard children”, neglect is defined as “persistent failure” to meet a child's basic physical and/or psychological needs.19 A major obstacle to the establishment of a general definition of child neglect is the problem of threshold, which is establishing what may be considered a minimally adequate level of care.20 It is very difficult to pinpoint when exactly the inadequacy of care becomes problematic.21 Therefore, the current study selected children who were clearly recorded as having experienced recurrent incidents of any subtypes of neglect over a certain time until just before death. There were some cases that had only one episode in the medico-legal documents. The current study did not include such gray-zone cases. Persistency means daily occurrence such as dirtiness of home environment or not having a bath for several days, or incidences of more than one episode such as not receiving any kind of public health service or canceling medical appointments. Persistency of any subtype of neglect was based on information taken from the medico-legal documents; two coauthors made the judgment of persistence and categorization of MMCS subtype.
Selection subjects
As Figure 1 shows, there were 13 050 postmortem external examinations for all age groups in one prefecture from 2006 to 2011. Of those, in 65 cases the age was identified as <2 years. One forensic pathologist carried out the autopsy in 59 cases (90.8%). The present study precisely examined the documents of 59 autopsies, and evaluated whether each victim had experienced any subtype of neglect in MMCS. After identifying 13 children who experienced neglect at least one time, persistency was confirmed in six cases, and these then became the study cases.
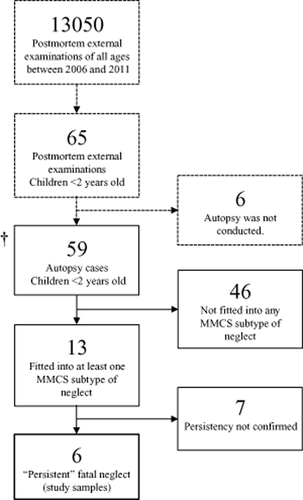
Flow chart of study samples. †Survey started at this point. MMCS, Modified Maltreatment Classification System.
Investigation of medico-legal documents
The documents were retained in the Department of Legal Medicine in Japan. Examiners in the current study extracted biological data, situation of death, family environment, and the use of maternal and child health services. They also noted body length, bodyweight, organ weight, conditions at death such as home environment, age of family members, family composition, the use of medical, and public health services from pregnancy until child rearing, and so on.
Assessment of weight loss and nutritional status
The Waterlow system that assesses the degree of malnutrition was used to evaluate nutritional status according to the weight and length data obtained.22 Decreased ratio of weight for length (W/L), represents wasting due to acute malnutrition, and decrease of length for age (L/A) represents stunting due to chronic malnutrition or nutritional growth failure. We used World Health Organization (WHO) Anthro version 3.2.223 to calculate W/L, L/A, and severity of undernutrition. According to the WHO Anthro manual, body height of children <24 months is described as length in the present study, instead of height, which is used for children aged ≥24 months.23
Ethics
The present study was approved by the official ethics review board of University of Tsukuba (document no. 807, Sep/13/2013).
Results
Persistent neglect
Table 1 lists the details of persistent neglect experienced, with MMCS subtype. Utilizing medico-legal documents, we investigated socio-familial and medical information (Table 2). In the six identified cases of persistent neglect, the home environment was described as unsanitary and unorganized in three cases. One child was found in the car. Time until detection varied from 1 h to 6.5 h. In the other two cases, the time of the last meal was longer than 12 h, which was not adequate at 2 months of age. In case 6 the child had been admitted to hospital with a 1 month history of pneumonia.
| Case | Age (month) | Sex | Food† | Clothing | Shelter‡ | Medical | Hygiene | Supervision§ | Environment | Substitute care |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 7 | M | Mother had not given milk because the child had vomited. Older sibling had taken over the milk usually. | Wearing clothes | Room was very dirty and cluttered with food waste, used diapers, clothes, and bottle of formula. | Child had never received infant regular check-ups and vaccinations. | Child was not given a bath, and diapers were not changed, resulting in diaper rash. | NA | NA | NA |
| 2 | 18 | F | Parents did not cook meals, left food bought outside, and sometimes passed expiry date. | Child was not wearing any clothes, only a diaper. | Room was very dirty with food waste, feces, dishes tobacco, and used diapers. The toilet did not flush. | Child had received infant regular check-up only once, and no vaccinations. Parents refused neonatal home visits. Parents did not visit hospital even though child had fever, cough and vomiting. | Child was not given a bath, and diapers were not changed for 1 week, resulting in diaper rash. | Caregiver repeatedly left child alone at home at night. | NA | NA |
| 3 | 2 | M | (13 h interval from last meal on day of death because mother was drunk.) | Wearing clothes | No problem | No problem | No problem | The caregiver left the victim and a sibling at home for several hours repeatedly. | NA | NA |
| 4 | 2 | M | (12 h interval from last meal on the day of death because mother felt annoyed at having to care.) | Wearing clothes | Room was littered and piled with many clothes, plastic bags, and cans of formula. | Mother canceled perinatal visit and refused neonatal home visiting. | No problem | NA | NA | NA |
| 5 | 6 | M | No problem | Wearing clothes | (No information on home environment. The child was left inside a cluttered car with blankets, no child seat.) | Mother canceled medical appointments and refused admission. | No problem | NA | NA | (An acquaintance was taking care of him, and left him alone inside a car.) |
| 6 | 16 | F | Child was placed in infant home at 4 months old due to failure to thrive after admission to hospital. | Wearing clothes | No problem | No problem | No problem | (Child became asphyxiated during milk feeding without supervision, in infant home at 5 months old.) | NA | NA |
- Bold, repeated experiences of child neglect. (xxx), one-off occurrence and not confirmed as persistent. NA, not available (unobtainable information). “No problem” means that the child did not fit into subtype of neglect in MMCS. MMCS coding is available from http://www.unc.edu/depts/sph/longscan/. Supplemental explanations were added operationally in this study for implementing the coding system precisely and adjusting Japanese situations. †Also includes providing inadequate food (e.g. beyond expiration date). ‡Dirtiness was defined as >30% of the area of the floor covered or cluttered with objects including unsanitary waste or harmful things (e.g. used diapers, or tobacco). §Repeatedly leaving a child alone at home for >3 h, or repeatedly leaving a child alone inside a car. MMCS, Modified Maltreatment Classification System.
| Case 1 (7 months, M) | Case 2 (18 months, F) | Case 3 (2 months, M) | Case 4 (2 months, M) | Case 5 (6 months, M) | Case 6 (16 months, F) | |
|---|---|---|---|---|---|---|
| Situation of death | ||||||
| Cause of death | Unclear | Pneumonia | Unclear | Unclear | Unclear | Pneumonia, multiple organ failure |
| Home environment | Dirty | Dirty | Clean | Disorganized | Found in car | Admitted to hospital |
| Time until detection | 1.5 h | 6.2 h | 4.5 h | 6.5 h | 1 h | – |
| Time from last meal | 4 h | 6.2 h | 13 h | 12 h | 3 h | – |
| Last meal before death | Almost no milk (milk given was taken by a sibling) | 3 pieces of sushi (expiration the day before) | Milk 110 mL | Milk 20–30 mL | Milk 300 mL | – |
| Family information | ||||||
| Age of father (years) | 21 | 20 | 35 | 38 | 53 | 36 |
| Age of mother (years) | 18 | 22 | 30 | 32 | 31 | 34 |
| Age of mother at delivery (years) | 17 | 20 | 29 | 31 | 31 | 33 |
| No. siblings | 1 | 0 | 1 | 1 | 3 | 2 (twin) |
| Age of sibling(s) (years) | 1 | – | 1 | 1 | 9, 8, and 3 | Both of them died at 1.3 and 2.3 years old |
| Age-difference between siblings | 13 months | – | More than 10 months | 17 months | More than 2.5 years | 6.5 years |
| Use of maternal and child health services | ||||||
| Weight at birth (g) | 2486 | 2998 | 2214 | 2412 | 2400 (approx.) | 2466 |
| No. prenatal care visits | 2 | 12 | 13 | 2 | NA | NA |
| First prenatal care visit (gestational week) | 28 | 9 | 8 | 19 | NA | Around 7 months |
| No. infant regular health check-ups | None | Once (at only 1 month age) | Once (at 1 month age.) | Once (at 1 month age.) | NA | 1, 3 months |
| Neonatal home visit | NA | Refused | NA | Refused | NA | NA |
| Vaccination | None | None | (None)a | (None)a | NA | NA |
- a Vaccination starts around 2 months old in Japan. NA, not available.
From family information, both parents were biological parents in six cases. Two out of the six mothers delivered the victims at <21 years old. All victims were the youngest child or only child. In three cases, there were siblings who were 1 year older than victims. In case 6, there were twin siblings, and both of them had died before the victim was born.
In terms of service use, mothers in cases 1, 4, and 6 had fewer perinatal care visits, and also the timing of the first visit was close or passed the possible limit of abortion. After discharge, mothers in cases 2 and 4 refused the neonatal home visit that the municipal government conducts for every infant <1 month old. Children in cases 1 and 2 did not receive any vaccines despite being older enough to receive routine vaccinations (from 2 months of age in Japan). In case 5, we could not obtain details on health service use from pregnancy until infancy.
Biological data
Table 3 lists body length, bodyweight and organ weight. References for body length and weight were taken from assessment of physical growth in Japanese children.24 Reference data for organ weight were drawn from “reports on medico-legal data from massive investigation performed by the Medico-Legal Society of Japan”.25 In six cases, all children had lower weight for age and sex-adjusted average. The average Z score for bodyweight in six cases was −2.22 (i.e. 2.22 SD below the mean). In particular, in case 4 the bodyweight Z score of the victim was −4.0, and most organs had decreased weight, except for the adrenal glands. In cases 1 and 2 the thymus had become remarkably involuted compared to other cases. In case 6, body length, weight, and brain and thymus weight were extremely low because the child had become ventilator dependent at around 1 year after hypoxic–ischemic encephalopathy due to asphyxia at 5 months old.
| Case | 1 | Mean | SD | z score | 2† | Mean | SD | z score | 3 | Mean | SD | z score | 4 | Mean | SD | z score | 5 | Mean | SD | z score | 6† | Mean | SD | z score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Body length (cm) | 61 | 69.2 | 2.4 | −3.4 | 80 | 79.4 | 2.7 | 0.2 | 55 | 57.9 | 2.2 | −1.3 | 57 | 57.9 | 2.2 | −0.4 | 67 | 67.8 | 2.4 | −0.3 | 61 | 77.5 | 2.6 | −6.3 |
| Bodyweight (kg) | 4.6 | 8.2 | 0.92 | −4.0 | 9 | 9.9 | 1.0 | −0.9 | 3.7 | 5.5 | 0.67 | −2.7 | 4.8 | 5.5 | 0.67 | −1.0 | 7.5 | 8.0 | 0.9 | −0.6 | 6.1 | 10.1 | 0.97 | −4.1 |
| Organ weight (g) | ||||||||||||||||||||||||
| Brain | 830 | 934 | 57 | −1.8 | 930 | 1022 | 103 | −0.9 | 640 | 616 | 59 | 0.4 | 510 | 616 | 59 | −1.8 | 800 | 842 | 80 | −0.5 | 490 | 1022 | 103 | −5.2 |
| Heart | 26 | 42 | 5.7 | −2.8 | 45 | 49 | 8.3 | −0.5 | 30 | 31 | 5.2 | −0.2 | 35 | 31 | 5.2 | 0.8 | 45 | 36 | 2.2 | 4.1 | 40 | 49 | 8.3 | −1.1 |
| Lung (left) | 45 | 67 | 12.8 | −1.7 | 75 | 78 | 22.4 | −0.1 | 45 | 51 | 7.3 | −0.8 | 55 | 51 | 7.3 | 0.5 | 65 | 59 | 10 | 0.6 | 35 | 78 | 22.4 | −1.9 |
| Lung (right) | 60 | 82 | 17.2 | −1.3 | 85 | 92 | 27.5 | −0.3 | 50 | 61 | 11.4 | −1.0 | 50 | 61 | 11.4 | −1.0 | 80 | 72 | 12 | 0.7 | 65 | 92 | 27.5 | −1.0 |
| Liver | 260 | 327 | 30.0 | −2.2 | 420 | 392 | 62.0 | 0.5 | 160 | 210 | 35.0 | −1.4 | 170 | 210 | 35 | −1.1 | 290 | 269 | 31 | 0.7 | 180 | 392 | 62.0 | −3.4 |
| Spleen | 15 | 34 | 13.7 | −1.4 | 45 | 37 | 13.1 | 0.6 | 15 | 41 | 11.2 | −2.3 | 15 | 41 | 11.2 | −2.3 | 40 | 15 | 29 | 0.9 | 25 | 37 | 13.1 | −0.9 |
| Pancreas | 10 | 14 | 3.7 | −1.1 | 11 | 21 | 9.3 | −1.1 | 4 | 6 | 1.9 | −1.1 | 6 | 6 | 1.9 | 0.0 | 10 | 14 | 12 | −0.3 | 5 | 21 | 9.3 | −1.7 |
| Kidney (left) | 20 | 27 | 4.0 | −1.8 | 27 | 32 | 7.1 | −0.7 | 20 | 22 | 4.0 | −0.5 | 20 | 22 | 4 | −0.5 | 40 | 26 | 5.3 | 2.6 | 25 | 32 | 7.1 | −1.0 |
| Kidney (right) | 20 | 30 | 5.1 | −2.0 | 28 | 32 | 6.5 | −0.6 | 15 | 21 | 4.3 | −1.4 | 20 | 21 | 4.3 | −0.2 | 40 | 25 | 4.9 | 3.1 | 25 | 32 | 6.5 | −1.1 |
| Adrenal gland (left) | 2 | 1.9 | 0.92 | 0.1 | 2 | 1.9 | 0.53 | 0.2 | 1 | 2.4 | 0.68 | −2.1 | 2 | 2.4 | 0.68 | −0.6 | 1 | 1.8 | 0.6 | −1.3 | 2 | 1.9 | 0.53 | 0.2 |
| Adrenal gland (right) | 2 | 2.1 | 0.95 | −0.1 | 1.5 | 1.6 | 0.58 | −0.2 | 1 | 2.1 | 0.63 | −1.7 | 2 | 2.1 | 0.63 | −0.2 | 1 | 1.7 | 0.56 | −1.3 | 2 | 1.6 | 0.58 | 0.7 |
| Thymus | 10 | 37 | 12.3 | −2.2 | 9 | 25.3 | 9.4 | −1.3 | 25 | 30.7 | 10.7 | −0.5 | 30 | 30.7 | 10.7 | −0.1 | 40 | 37 | 10.6 | 0.3 | 5 | 25.3 | 9.4 | −2.2 |
- Reference data matched for age and sex. †Reference was 12-month-old girl, because the reference data was shown in monthly figure during 0–11 month age and yearly after 1 year old.
Nutrition status
Scores for W/L L/A are listed in Table 4, with three grades of severity of undernutrition.26-28 Using the WHO classification to evaluate nutritious status, z score of W/L and L/A in case 1 were less than −3.0, which represents severe wasting and severe stunting. Likewise, the child in case 3 had moderate wasting and severe stunting, and the child in case 6 had severe stunting.
| Severity of undernutrition | ||||||
|---|---|---|---|---|---|---|
| Case | 1 | 2 | 3 | 4 | 5 | 6 |
| Weight for length (Z score) | −3.34 | −1.31 | −2.49 | −0.78 | −0.04 | −0.05 |
| Length for age (Z score) | −3.98 | −0.35 | −3.09 | −1.85 | −0.71 | −6.33 |
| Wasting (acute) | Severe | Mild | Moderate | Normal | Normal | Normal |
| Stunting (chronic) | Severe | Normal | Severe | Mild | Normal | Severe |
| WHO classification of child undernutrition | ||||||
|---|---|---|---|---|---|---|
| Severe | Moderate | Mild | ||||
| Z score < −3 | −3 ≤ Z score < −2 | −2 ≤ Z score < −1 | ||||
Discussion
Utilizing medico-legal documents, we investigated fatal cases of persistent neglect from the two aspects of legal medicine and public health, and described the detailed process and the effects of fatal neglect on children.
Socio-family background and history of service use
Multiple births are noted as one of the risk factors for child maltreatment,29, 30 and having several siblings in the family is another risk factor.31, 32 Although sibling age difference has not been reported as a risk factor, a 1 year difference between siblings was noted in three cases in the present study. One sibling (case 1; 1 year old) had never received vaccinations and health check-ups, and the other sibling (case 3; 1 year old) had been left at home with the victim for several hours. Further research is needed to determine the age and number of siblings most likely to be seen as a burden to parents when raising them together.
Moreover, neglect is associated with poverty. Children of low socioeconomic status were found to be sevenfold more likely to be neglected in the US Fourth National Incidence Study.33 In case 1, even after the parents realized that their child had delayed development, they stated that they had never visited a physician due to financial reasons. Other parents (case 2) stopped utilizing a daycare center 2 months prior to the death because they could not afford the fee and both parents went out to work while the child was left at home alone. We could not, however, evaluate the actual financial conditions and parenting attitudes in more detail. Collection of information from multi-disciplinary organizations is therefore needed in order to evaluate why and how neglect was occurring.
With regard to health service use, three mothers had fewer prenatal care visits and later first visits to obstetrics. In Japan, 86.9% of mothers visited the municipal office and received the Mother and Child Health (MCH) handbook by 11 weeks of gestation, after confirmation of the pregnancy at obstetrics.34 The Japanese Government recommends 14 prenatal visits at clinics or hospitals. Therefore, later first visit and fewer prenatal care visits may reflect unexpected pregnancy or failure to abort. Problems in the prenatal period would be carried over to the child rearing period. Knowing the timing of the first visit and the number of prenatal care visits is very important for assessing the mothers' willingness and conflicts with regard to child rearing. Support for mothers starting in pregnancy may help prevent fatal child neglect.
Loss of bodyweight and undernutrition
The extent of weight loss in actual fatal neglect has not been sufficiently recognized in Japan, even though failure to thrive, or FTT is a known indicator of neglect.35 As noted, this study confirmed the extent of lower bodyweight. In cases 1 and 3 the children fitted the definition of FTT given that the Z score of weight for age was less than −2, and their weight loss Z score was −4.0 and −2.7, respectively. Although the child in case 6 had been diagnosed with FTT on a Z score of −3.7 at 4 months old, it was difficult to evaluate bodyweight at death with regard to nutritional status because of the long period of ventilation dependence.
Utilizing the Waterlow system and the WHO classification to evaluate nutritious status, the children in cases 1 and 3 had acute and chronic undernutrition. According to previous studies, children with weight for height below −3 SD based on the WHO standards have more than a ninefold higher risk of death compared to children with weight for height above −1 SD.36
It is important for medical professionals who may see neglected children to pay much closer attention to the extent of decrease of bodyweight and nutrition status.
Thymus involution due to long-term child neglect
Autopsy identified thymic involution in cases 1, 2 and 6. The children in cases 1 and 2 had more overlapping subtypes of neglect compared with the other four children. Thymus involution has been correlated with degree and duration of physical abuse and neglect,37 and immunodeficiency secondary to thymus involution can occur due to long-term child abuse.8, 38 The child in case 6 might have been affected by both chronic maltreatment and the stress of long-term ventilation. But, as seen in case 2, delay in visiting the physician is considered as medical neglect given that the parents failed to take the child to the clinic or hospital even after she had had fever, cough, vomiting and fatigue for 1 week. The victim received no vaccination, no regular health check-ups after 1 month old, and repeated exacerbation of atopic dermatitis and one occurrence of subcutaneous abscess. Combination of basic poor skin hygiene, immunosuppression due to thymus involution caused by persistent neglect, and delay of medical care could have led to the child's death, with exacerbation of pneumonia at the end. To prevent successive deaths from neglect, involution of the thymus should be noted as an important factor in the assessment of the probability of child maltreatment.
Collaboration of public health and legal medicine for prevention of child neglect
Collaboration between public health and legal medicine enabled collection of detailed background information and data on the biological effects of neglect on children in this study. In previous national reports of fatal child maltreatment, results of reviews were classed together as all types of fatal maltreatment. Therefore, we focused on only neglect cases, using the MMCS subtypes “failure to provide” and “lack of supervision”, and the dimension of “persistency”. The present findings, which have not been described in national reports, related to death situation parameters, including time until detection and time from last meal, age differences between siblings, and biological autopsy data.
Among six victims, previous involvement with Child Guidance Center was found in only case 6 at the time of FTT diagnosis. There was only one child those caregivers were prosecuted and reported in the newspapers, according to the medico-legal documents. Therefore, medico-legal documents have the potential to review child deaths that have not been reviewed in the existing national child fatal maltreatment reports.
Limitations and future directions
There were several limitations in the present study. Although collected information was multidirectional and meaningful to review, autopsy might not identify every cause of death. Second, if physicians failed to report the case as unnatural death, or failed to understand the importance of postmortem external examination and autopsy for determining the cause of death, the case would never have been recorded and examined by forensic physicians. Third, the number of subjects was extremely small in the present study. To set up preventive strategies, further research is needed to evaluate situations in which child neglect occurred in both an acute manner and for a persistent period. Last, parental responsibility differs on a cultural basis. It is recommended to examine what kinds of failure to provide and lack of supervision are suitable in Japanese society for identifying neglect cases in a timely manner before the neglect becomes fatal. Furthermore, failure to provide existed in most of the present cases, but identification of lack of supervision was limited. Raising awareness that lack of supervision is also a key part of neglect is necessary in order to identify the actual situation of neglect in Japan.
Conclusion
By integrating biological data and information on socio-familial background obtained from medico-legal documents, we were able to collect details on different subtypes of child neglect. A multidisciplinary system of integrating detailed information and evaluating death cases is needed to identify preventable factors in fatal child maltreatment.
Acknowledgment
This research was supported by JSPS KAKENHI #24249031 (Grant-in-Aid for Scientific Research A).