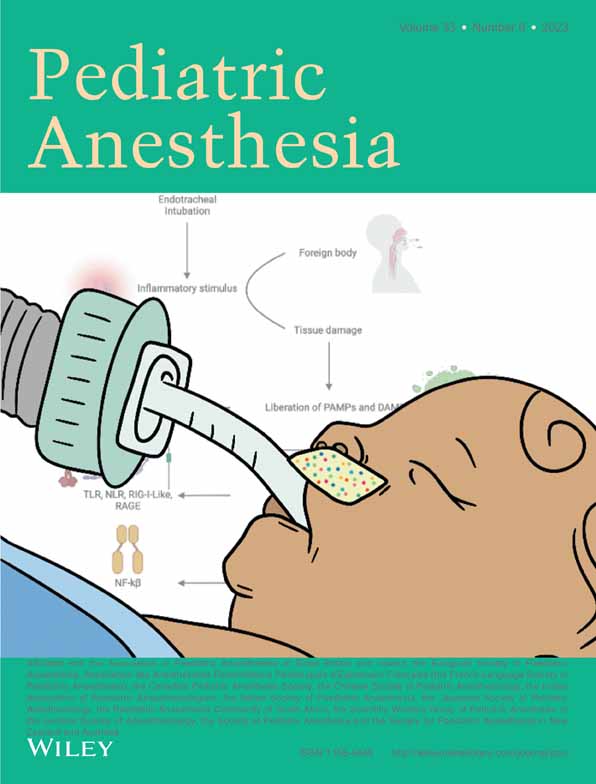
The role of local inflammation in complications associated with intubation in pediatric patients: A narrative review
Corresponding Author
Sebastian Amaya
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Department of Anesthesiology and Pain Medicine, Nationwide Children's Hospital, Columbus, Ohio, USA
Correspondence
Sebastian Amaya, Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia.
Email: [email protected]
Search for more papers by this authorMarcelino Murillo
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Department of Anesthesiology and Pain Medicine, Nationwide Children's Hospital, Columbus, Ohio, USA
Search for more papers by this authorMartha L. Gutiérrez Pérez
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Otorhinolaryngology Interest Group, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorHector S. Cervera
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorMaría J. Andrade
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorMaría A. Zuñiga
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorNatalia Barreto
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorMaría I. Daza
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorLuisa F. Carvajal
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorCatalina M. Alarcón
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorLaura Aponte
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorVanessa A. Olbrecht
Department of Anesthesiology and Pain Medicine, Nationwide Children's Hospital, Columbus, Ohio, USA
Search for more papers by this authorCorresponding Author
Sebastian Amaya
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Department of Anesthesiology and Pain Medicine, Nationwide Children's Hospital, Columbus, Ohio, USA
Correspondence
Sebastian Amaya, Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia.
Email: [email protected]
Search for more papers by this authorMarcelino Murillo
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Department of Anesthesiology and Pain Medicine, Nationwide Children's Hospital, Columbus, Ohio, USA
Search for more papers by this authorMartha L. Gutiérrez Pérez
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Otorhinolaryngology Interest Group, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorHector S. Cervera
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorMaría J. Andrade
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorMaría A. Zuñiga
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorNatalia Barreto
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorMaría I. Daza
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorLuisa F. Carvajal
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorCatalina M. Alarcón
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorLaura Aponte
Anesthesiology and Critical Care Interest Group, Universidad El Bosque, Bogotá, Colombia
Colombian School of Medicine, Universidad El Bosque, Bogotá, Colombia
Search for more papers by this authorVanessa A. Olbrecht
Department of Anesthesiology and Pain Medicine, Nationwide Children's Hospital, Columbus, Ohio, USA
Search for more papers by this authorSection Editor: Britta S von Ungern-Sternberg
Abstract
Although the most important primary local inflammatory response factor to intubation is not yet clear, it is known that it may be directly attributed to the presence of trauma during intubation or the response of oral bacterial flora present in the trachea. It is known that prolonged intubation is associated with worse outcomes, but other underlying systemic issues, such as sepsis and trauma, are also associated with this result. Likewise, patients who require advanced airway management and excessive manipulation are more likely to experience complications. There are various inflammatory mediators that are generated during orotracheal intubation, many of which can be considered targets for therapies to help reduce inflammation caused by intubation. However, there is little evidence on the management of the inflammatory response induced by orotracheal intubation in pediatric patients. Therefore, the aim of this narrative review is to highlight the intubation associated complications that can arise from poorly controlled inflammation in intubated pediatric patients, review the proposed pathophysiology behind this, and discuss the current treatments that exist. Finally, taking into account the discussion on pathophysiology, we describe the current therapies being developed and future directions that can be taken in order to create more treatment options within this patient population.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
REFERENCES
- 1Puyo CA, Dahms TE. Innate immunity mediating inflammation secondary to endotracheal intubation. Arch Otolaryngol - Head Neck Surg. 2012; 138(9): 854-858.
- 2Puyo CA, Earhart A, Staten N, et al. Endotracheal intubation results in acute tracheal damage induced by mtDNA/TLR9/NF-κB activity. J Leukoc Biol. 2019; 105(3): 577-587.
- 3Holzki J, Laschat M, Puder C. Iatrogenic damage to the pediatric airway mechanisms and scar development. Pediatr Anesth. 2009; 19: 131-146.
- 4Vasileiou PVS, Chalkias A, Brozou V, et al. Interleukin-6 as a marker of inflammation secondary to endotracheal intubation in pediatric patients. Inflammation. 2013; 36(6): 1533-1538.
- 5Gourlay T, Samartzis I, Stefanou D, Taylor K. Inflammatory response of rat and human neutrophils exposed to Di-(2-ethyl-hexyl)-phthalate-plasticized polyvinyl chloride. Artif Organs. 2003; 27(3): 256-260.
- 6Puyo CA, Tricomi SM, Dahms TE. Early biochemical markers of inflammation in a swine model of endotracheal intubation. Anesthesiology. 2008; 109(1): 88-94.
- 7Naunheim MR, Zhou AS, Puka E, et al. Laryngeal complications of COVID-19. Laryngoscope Invest Otolaryngol. 2020; 5(6): 1117-1124.
- 8Hollander DD, Muckart DJ. Post-extubation stridor in children: a case report and review of the literature. South Afr J Crit Care. 2009; 25: 20-26.
- 9Sue RD, Susanto I. Long-term complications of artificial airways. Clin Chest Med. 2003; 24(3): 457-471.
- 10Shahzad T, Radajewski S, Chao C-M, Bellusci S, Ehrhardt H. Pathogenesis of bronchopulmonary dysplasia: when inflammation meets organ development. Mol Cell Pediatr. 2016; 3(1): 23.
- 11Hussain WA, Marks JD. Approaches to noninvasive respiratory support in preterm infants: from CPAP to NAVA. Neoreviews. 2019; 20(4): e213-e221.
- 12Touman AA, Stratakos GK. Long-term complications of tracheal intubation. In: Tracheal Intubation. InTech; 2018.
- 13Gaynor EB, Greenberg SB. Untoward sequelae or prolonged intubation. Laryngoscope. 1985; 95(12): 1461-1467.
- 14Rivera R, Tibballs J. Complications of endotracheal intubation and mechanical ventilation in infants and children. Crit Care Med. 1992; 20(2): 193-199.
- 15Kato A, Schleimer RP. Beyond inflammation: airway epithelial cells are at the interface of innate and adaptive immunity. Curr Opin Immunol. 2007; 19(6): 711-720.
- 16Pouwels SD, Heijink IH, ten Hacken NH, et al. DAMPs activating innate and adaptive immune responses in COPD. Mucosal Immunol. 2014; 7(2): 215-226.
- 17Roh JS, Sohn DH. Damage-associated molecular patterns in inflammatory diseases. Immune Netw. 2018; 18(4): e27.
- 18Pouwels SD, Zijlstra GJ, van der Toorn M, et al. Cigarette smoke-induced necroptosis and DAMP release trigger neutrophilic airway inflammation in mice. Am J Physiol Cell Mol Physiol. 2016; 310(4): L377-L386.
- 19Simopoulos AP. Omega-3 fatty acids in inflammation and autoimmune diseases. J Am Coll Nutr. 2002; 21(6): 495-505.
- 20Cannizzaro V, Hantos Z, Sly PD, Zosky GR. Linking lung function and inflammatory responses in ventilator-induced lung injury. Am J Physiol Cell Mol Physiol. 2011; 300(1): L112-L120.
- 21Pneumatikos IA, Dragoumanis CK, Bouros DE, Warner DS, Warner MA. Ventilator-associated pneumonia or endotracheal tube-associated pneumonia? Anesthesiology. 2009; 110(3): 673-680.
- 22Puyo CA, Peruzzi D, Earhart A, et al. Endotracheal tube-induced sore throat pain and inflammation is coupled to the release of mitochondrial DNA. Mol Pain. 2017; 12(13): 174480691773169.
- 23Joshi VV. Acute lesions induced by endotracheal intubation. Am J Dis Child. 1972; 124(5): 646.
- 24Jang M, Basa K, Levi J. Risk factors for laryngeal trauma and granuloma formation in pediatric intubations. Int J Pediatr Otorhinolaryngol. 2018; 107: 45-52.
- 25Sathyamoorthy M, Lerman J, Asariparampil R, Penman AD, Lakshminrusimha S. Stridor in neonates after using the microcuff® and uncuffed tracheal tubes. Anesth Analg. 2015; 121(5): 1321-1324.
- 26Chen L, Zhang J, Pan G, Li X, Shi T, He W. Cuffed versus uncuffed endotracheal tubes in pediatrics: a meta-analysis. Open Med. 2018; 13(1): 366-373.
10.1515/med-2018-0055 Google Scholar
- 27Fine GF, Borland LM. The future of the cuffed endotracheal tube. Pediatr Anesth. 2004; 14(1): 38-42.
- 28Liew FY. Toll-like receptor 2 signalling and inflammation. Ann Rheum Dis. 2005; 64(Suppl 4): iv104-iv105.
- 29Chen G, Shaw MH, Kim Y-G, Nuñez G. NOD-like receptors: role in innate immunity and inflammatory disease. Annu Rev Pathol Mech Dis. 2009; 4(1): 365-398.
- 30Bermejo-Jambrina M, Eder J, Helgers LC, et al. C-type lectin receptors in antiviral immunity and viral escape. Front Immunol. 2018; 9: 590.
- 31Mosquera J. Role of the receptor for advanced glycation end products (RAGE) in inflammation. Invest Clin. 2010; 51: 257-268.
- 32Dinarello CA. Interleukin-1β. Crit Care Med. 2005; 33(Suppl): S460-S462.
- 33Zelová H, Hošek J. TNF-α signalling and inflammation: interactions between old acquaintances. Inflamm Res. 2013; 62(7): 641-651.
- 34Kimura S, Ahn JB, Takahashi M, Kwon S, Papatheodorou S. Effectiveness of corticosteroids for post-extubation stridor and extubation failure in pediatric patients: a systematic review and meta-analysis. Ann Intensive Care. 2020; 10(1): 155.
- 35Veldhoen ES, Smulders CA, Kappen TH, et al. Post-extubation stridor in respiratory syncytial virus bronchiolitis: is there a role for prophylactic dexamethasone? PLoS One. 2017; 12(2):e0172096.
- 36Cheng K-C, Hou C-C, Huang H-C, Lin S-C, Zhang H. Intravenous injection of methylprednisolone reduces the incidence of postextubation stridor in intensive care unit patients*. Crit Care Med. 2006; 34(5): 1345-1350.
- 37Lee C-H, Peng M-J, Wu C-L. Dexamethasone to prevent postextubation airway obstruction in adults: a prospective, randomized, double-blind, placebo-controlled study. Crit Care. 2007; 11(4): R72.
- 38Derendorf H, Nave R, Drollmann A, Cerasoli F, Wurst W. Relevance of pharmacokinetics and pharmacodynamics of inhaled corticosteroids to asthma. Eur Respir J. 2006; 28(5): 1042-1050.
- 39Barnes PJ, Adcock IM. How do corticosteroids work in asthma? Ann Intern Med. 2003; 139(5_Part_1): 359.
- 40Ericson-Neilsen W, Kaye AD. Steroids: pharmacology, complications, and practice delivery issues. Ochsner J. 2014; 14(2): 203-207.
- 41Williams DM. Clinical pharmacology of corticosteroids. Respir Care. 2018; 63(6): 655-670.
- 42Lnu R, Jhamb U. Dexamethasone in prevention of Postextubation stridor in ventilated children: a randomized, double-blinded, placebo-controlled trial. Indian J Crit Care Med. 2020; 24(12): 1230-1235.
- 43Lukkassen I, Hassing MBF, Markhorst D. Dexamethasone reduces reintubation rate due to postextubation stridor in a high-risk paediatric population. Acta Paediatr. 2006; 95(1): 74-76.
- 44Baranwal AK, Meena JP, Singhi SC, Muralidharan J. Dexamethasone pretreatment for 24 h versus 6 h for prevention of postextubation airway obstruction in children: a randomized double-blind trial. Intensive Care Med. 2014; 40(9): 1285-1294.
- 45Lu J, Tian W, Cui L, et al. Lidocaine-eluting endotracheal tube effectively attenuates intubation related airway response. Ann Transl Med. 2021; 9(10): 871.
- 46Thapa P, Shrestha RR, Shrestha S, Bajracharya GR. Betamethasone gel compared with lidocaine jelly to reduce tracheal tube related postoperative airway symptoms: a randomized controlled trial. BMC Res Notes. 2017; 10(1): 361.
- 47Abu Ammar A, Gruber M, Martin P, et al. Local delivery of mometasone furoate from an eluting endotracheal tube. J Control Release. 2018; 272: 54-61.
- 48Wang G, Qi Y, Wu L, Jiang G. Comparative efficacy of 6 topical pharmacological agents for preventive interventions of postoperative sore throat after tracheal intubation: a systematic review and network meta-analysis. Anesth Analg. 2021; 133(1): 58-67.
- 49Mekhemar NA, El-agwany AS, Radi WK, El-Hady SM. Estudo comparativo entre cloridrato de benzidamina em gel, lidocaína a 5% em gel e lidocaína a 10% em spray no balonete do tubo endotraqueal em relação à dor de garganta pós-operatória. Braz J Anesthesiol. 2016; 66(3): 242-248.
- 50Yhim H-B, Yoon S-H, Jang Y-E, et al. Effects of benzydamine hydrochloride on postoperative sore throat after extubation in children: a randomized controlled trial. BMC Anesthesiol. 2020; 20(1): 77.
- 51Bai M, Zhao B, Liu Z, et al. Mucosa-like conformal hydrogel coating for aqueous lubrication. Adv Mater. 2022; 8: 2108848.
- 52Hashemi MM, Rovig J, Bateman J, et al. Preclinical testing of a broad-spectrum antimicrobial endotracheal tube coated with an innate immune synthetic mimic. J Antimicrob Chemother. 2018; 73(1): 143-150.
- 53Zhao B, Li Y-P, Wang Q, et al. Ultra-slippery, nonirritating, and anti-inflammatory hyaluronic acid-based coating to mitigate intubation injury. Chem Eng J. 2022; 427:130911.
- 54Jung H, Lee JS, Lee JJ, Park HS. Anti-inflammatory and anti-bacterial effects of allicin-coated tracheal tube on trachea mucosa. In Vivo. 2022; 36(3): 1195-1202.
- 55Aronson MR, Ali Akbari Ghavimi S, Gehret PM, Jacobs IN, Gottardi R. Drug-eluting endotracheal tubes for preventing bacterial inflammation in subglottic stenosis. Laryngoscope. 2022; 132(7): 1356-1363.
- 56Piscianz E, Tesser A, Rimondi E, Melloni E, Celeghini C, Marcuzzi A. MitoQ is able to modulate apoptosis and inflammation. Int J Mol Sci. 2021; 22(9): 4753.
- 57Sallam MY, El-Gowilly SM, Abdel-Galil A-GA, El-Mas MM. Cyclosporine counteracts endotoxemia-evoked reductions in blood pressure and cardiac autonomic dysfunction via central sGC/MAPKs signaling in rats. Eur J Pharmacol. 2017; 797: 143-152.
- 58Wang K, Wu M, Xu J, et al. Effects of dexmedetomidine on perioperative stress, inflammation, and immune function: systematic review and meta-analysis. Br J Anaesth. 2019; 123(6): 777-794.
- 59Rudra A, Ray S, Chatterjee S, Ahmed A, Ghosh S. Gargling with ketamine attenuates the postoperative sore throat. Indian J Anaesth. 2009; 53(1): 40-43.