The effect of dexmedetomidine premedication on postoperative systemic inflammatory response in children undergoing hernia repair surgery: A randomized controlled trial
Trial registration: ChiCTR, ChiCTR1900026795. Registered October 22, 2019; http:// www.chictr.org.cn
Funding information
This study was funded by the Medical Scientific Research Fund of the Health Department of Hunan Province, China [grant number B2016042].
Abstract
Background
Surgery results in systemic inflammation, which can affect the central nervous system, leading to changes in mood, emotion, and behavior. Our previous study has shown that compared to midazolam, dexmedetomidine premedication effectively decreased children's postoperative anxiety.
Aim
To investigate whether dexmedetomidine infusion before hernia repair alleviates postoperative systemic inflammation in children and whether postoperative anxiety may be associated with postoperative inflammation.
Methods
This prospective double-blind randomized controlled trial was conducted in 120 children scheduled to undergo elective hernia repair. Before anesthesia induction, all children received an intravenous infusion consisted of dexmedetomidine (n = 40; 0.5 µg/g, group D), midazolam (n = 40; 0.08 mg/kg, group M), or normal saline (n = 40; group C). One-way ANOVA with least significant difference multiple comparison test was used for multigroup comparisons of postoperative plasma levels of inflammatory cytokines and m-YPAS scores. Spearman rank correlation tests were used for analyzing m-YPAS scores with postoperative plasma levels of inflammatory cytokines.
Results
Plasma levels of tumor necrosis factor-alpha (7.0 ± 1.6 vs. 8.1 ± 1.6, mean difference [95% CI]: 1.19 [0.26–2.11], p = .008) (pg/ml) and of interleukin-6 (1.8 ± 1.2 vs. 3.3 ± 1.6, mean difference [95% CI]: 1.49 [0.74–2.25], p < .001) (pg/ml) and neutrophils-to-lymphocyte ratio (1.0 ± 0.5 vs. 1.5 ± 0.7, mean difference [95% CI]: 0.48 [0.17–0.78], p < .001) were significantly lower in group D than in group C. Furthermore, compared to group M, group D showed significantly lower plasma tumor necrosis factor-alpha levels (7.0 ± 1.6 vs. 7.9 ± 1.9, mean difference [95% CI]: 0.96 [0.04–1.88], p = .04) (pg/ml) and interleukin-6 levels (1.8 ± 1.2 vs. 2.9 ± 1.5, mean difference [95% CI]: 1.06 [0.31–1.81], p = .004) (pg/ml), and neutrophil-to-lymphocyte ratio (1.0 ± 0.5 vs. 1.5 ± 0.6, mean difference [95% CI]: 0.42 [0.11–0.72], p = .004). Anxiety scores at postoperative 2 and 4 h in the three groups positively correlated with plasma levels of proinflammatory cytokines.
Conclusion
A single preoperative intravenous dexmedetomidine dose in children undergoing same-day surgery reduces postoperative systemic inflammation.
What is already known about the topic
- Dexmedetomidine premedication effectively decreases children's postoperative anxiety.
- Postoperative anxiety is positively related to preoperative anxiety and postoperative pain.
What new information this study adds
- Dexmedetomidine premedication can effectively decrease children's postoperative systemic inflammation.
- Postoperative anxiety may also be positively related to postoperative systemic inflammation.
1 INTRODUCTION
Increased levels of proinflammatory cytokines, including tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6), are early features of acute injury. Surgical procedures elicit a complex, systemic inflammatory response effectuated and modulated by cytokines.1 Systemic infection and inflammation trigger signals that influence the central nervous system (CNS), leading to changes in mood, emotion, and behavior.2 Some studies quantified the associations among psychological variables and inflammatory response components.3, 4 Increased circulating TNF-α concentrations have been found in patients with anxiety disorders.5 Higher levels of C-reactive protein (CRP) have been found among children with anxiety than among controls.6
Up to 50%–75% of children undergoing surgery experience considerable anguish and anxiety during the perioperative period.7, 8 Factors that may affect postoperative anxiety and negative experiences include the child's and parents’ preoperative anxiety, child's temperament, previous hospitalization for surgery, preoperative preparation and medications, kinds of anesthetics used, the presence of parents during the induction of anesthesia, the child's experience in the postanesthetic care unit (PACU), and postoperative pain.7-10 However, whether postoperative inflammation can affect postoperative anxiety has not yet been examined.
The effects of dexmedetomidine on inflammation have been demonstrated in some clinical settings and studies. Medium and high concentrations of dexmedetomidine inhibited the expression and release of inflammatory factors in mice.11 Adult patients receiving a 1.0 μg/kg loading dose of dexmedetomidine followed by infusion at 0.5 μg/kg/h for laparoscopic cholecystectomy showed a decreased inflammatory response.12 Our previous study showed that dexmedetomidine, compared with midazolam, as premedication, lowered postoperative anxiety in children undergoing same-day surgery.13 Hence, in this study, we test our hypotheses that dexmedetomidine premedication can relieve postoperative systemic inflammation in children and postoperative systemic inflammation may be one of the related factors affecting postoperative anxiety.
2 MATERIALS AND METHODS
2.1 Patient selection
This was a randomized, double-blind, controlled trial. The study was performed in Hunan Children's Hospital, approved by the Ethics Committee of Hunan Children's Hospital (HCHLL-2016–002, Chairperson: Prof Si-Jun Zhao), and registered in the Chinese Clinical Trial Registry (ChiCTR-IPR-1900026795). Written informed consent was obtained from parents, and verbal consent was obtained from each child.
Potential participants were screened at the preoperative visit. Children aged 6 to 11 years with American Society of Anesthesiologists physical status of I and II and scheduled for elective hernia repair under general anesthesia were considered eligible for inclusion. The exclusion criteria were as follows: complicated hernia, a known allergy or hypersensitive reaction to dexmedetomidine or midazolam, long-term use of sedative or analgesic drugs, long-term use of steroids or anti-inflammatory drugs, a history of surgery or anesthesia, current upper respiratory infections, asthma, developmental delay, psychological diagnosis requiring active treatment, or congenital or neurological diseases.
2.2 Study design
Random numbers were generated by a statistician by using computer software. Children were randomly allocated into three groups in a 1:1:1 ratio. According to the random numbers, an anesthesia nurse not involved in the experiment prepared 20 ml of normal saline containing dexmedetomidine (0.5 μg/kg) or midazolam (0.08 mg/kg) or without dexmedetomidine/ midazolam. The dexmedetomidine and midazolam doses were selected based on our previous study showing they were equivalent in reducing separation anxiety and cause no cardiovascular instability.13 The randomization numbers were then sealed in envelopes. The anesthetists, surgeons, children, and parents were blind to group allocation. All anesthesia procedures were performed by the same two attending anesthesiologists. Operations were performed by a surgical team that included three pediatric surgeons.
2.3 Anesthesia procedure and perioperative care
Anesthesia procedure and perioperative care were as described previously.13 In a pre-anesthesia holding room, children in groups D, M, and C received an IV infusion of dexmedetomidine (0.5 μg/kg), midazolam (0.08 mg/kg), and normal saline, respectively, for 10 min. All the children were transported to the operating room with their parents 10 min later.
IV sufentanyl 0.2 μg/kg and inhalation of sevoflurane (4%–6%) in oxygen at 6 L/min were used for induction. A laryngeal mask airway was inserted, and the child was kept in spontaneous ventilation. Anesthesia was maintained by inhalation of sevoflurane in oxygen at 2 L/min, which was regulated to maintain the Narcotrend index between 40 and 60 during the surgery.
At the end of the surgery, 2 ml of 0.2% ropivacaine was used for wound infiltration. Then, the anesthetics were stopped and the laryngeal mask was removed. Children were transferred to the PACU and discharged from the hospital within 24 h.
If the child's postoperative pain score was equal to or greater than 4, it was recorded and the child was administered intravenous sufentanyl 0.05 μg/kg for rescue. The children were not allowed to use steroids or other drugs with an anti-inflammatory effect during the perioperative period.
2.4 Data collection
The primary outcomes were postoperative plasma levels of inflammatory factors. Venous blood samples (2.0 ml each) were drawn after surgery and before the cessation of sevoflurane inhalation. Plasma samples were immediately separated by centrifugation at 3000 rpm for 10 min at 4°C, divided into aliquots, and stored at −80°C for subsequent assays using highly sensitive enzyme-linked immunosorbent assay kits to detect the proinflammatory TNF-α and IL-6. The neutrophil-to-lymphocyte ratio (NLR) was obtained from the absolute neutrophil count and the absolute lymphocyte counts.
The secondary outcomes included children's perioperative anxiety scores, postoperative pain, and the correlation between postoperative inflammation and postoperative anxiety. Children's preoperative and postoperative anxiety levels were measured using the modified Yale Preoperative Anxiety Scale (m-YPAS) at the preoperative interview, and postoperative 2 and 4 h in the ward.14 Pain was measured 2 h and 4 h postoperatively using the visual analogue scale (VAS), which had been explained to the children and their parents during a preoperative visit. Its values range from 0 (no discomfort and no pain) to 10 (high discomfort and maximum pain). Data were collected by an anesthesiologist who was blind to group assignment. She was trained in data collection and scoring the tools to ensure inter-rater reliability.
2.5 Statistical analyses
Sample size was estimated according to the plasma level of TNF-α, a major proinflammatory cytokine. A pilot study in 10 children with no premedication, 10 children who received midazolam premedication, and 10 children who received dexmedetomidine at Hunan Children's Hospital found that the TNF-α levels (mean ±standard deviation [SD]) in the three groups were 8.2 ± 1.7, 7.8 ± 1.8, and 6.8 ± 1.5 (pg/ml) respectively. Thus, a sample size of 37 per group was necessary to achieve a power of 90% and a type I error of 5%. To compensate for the possibility of dropout, 120 children, with 40 children per group, were recruited.
The data are expressed as the mean ± SD, median, interquartile range (IQR), or numbers. Multigroup comparisons in age, weight, surgery duration, TNF-α and IL-6 levels, NLR, and m-YPAS and VAS scores were analyzed via one-way ANOVA with least significant difference (LSD) multiple comparison tests. Sex was analyzed using the χ2 test. Spearman rank correlation analyses were performed for m-YPAS scores at 2 h and 4 h postoperatively with postoperative TNF-α and IL-6 levels and NLR. Statistical analyses were performed using SPSS 19.0 (SPSS). p-values <.05 were considered statistically significant.
3 RESULTS
3.1 Children's characteristics
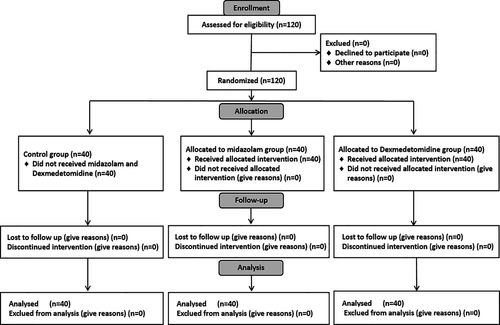
Between October 2019 and January 2020, a total of 120 patients were enrolled, and all 120 patients completed the study (Figure 1). The three groups showed no significant differences in the demographics and the duration of the operations between the three groups (Table 1). All of the children were discharged as scheduled without any complications.
| Variables |
Group C (n = 40) |
Group M (n = 40) |
Group D (n = 40) |
p |
|---|---|---|---|---|
| Age (year) | 7.6 ± 1.2 | 7.8 ± 1.6 | 7.6 ± 1.5 | .983 |
| Males/females | 23/17 | 22/18 | 25/15 | .822 |
| Body weight (kg) | 24.5 ± 4.5 | 25.4 ± 5.3 | 24.7 ± 6.3 | .672 |
| Duration of surgery (min) | 26.9 ± 6.1 | 25.0 ± 5.1 | 25.9 ± 6.3 | .354 |
- Data are shown as the number or mean ± standard deviation values.
3.2 Postoperative systemic inflammation
The three groups showed significant differences in the postoperative plasma levels of TNF –α (p = .006) and IL-6 (p < .001) and the NLR (p < .001). The plasma levels of TNF-α (7.0 ± 1.6 vs. 8.1 ± 1.6, mean difference [95% CI]: 1.19 [0.26–2.11], p = .008) (pg/ml) and IL-6 (1.8 ± 1.2 vs. 3.3 ± 1.6, mean difference [95% CI]: 1.49 [0.74–2.25], p < .001) (pg/ml) and the NLR (1.1 0 ± 0.5 vs. 1.5 ± 0.7 mean difference [95% CI]: 0.48 [0.17–0.78], p < .001) were lower in group D than in group C. In comparison with group M, group D also showed significantly lower levels of TNF-α (7.0 ± 1.6 vs. 7.9 ± 1.9, mean difference [95% CI]: 0.96 [0.04–1.88], p = .04) (pg/ml) and IL-6 (1.8 ± 1.2 vs. 2.9 ± 1.5, mean difference [95% CI]: 1.06 [0.31–1.81], p = .004) (pg/ml) as well as a lower NLR (1.1 0 ± 0.5 vs. 1.5 ± 0.56, mean difference [95% CI]: 0.42 [0.11–0.72], p = .004) after surgery. The values for these three inflammatory factors were similar in groups M and C (Table 2).
| Variables |
Group C (n = 40) |
Group M (n = 40) |
Group D (n = 40) |
Mean difference (95% CI) | p |
|---|---|---|---|---|---|
| TNF-α (pg/ml) | 8.1 ± 1.6 | 7.9 ± 1.9 | 7.0 ± 1.6a,b |
1.19 (0.26–2.11), a = 0.008 0.96 (0.04–1.88), b = 0.04 |
.006 |
| IL−6 (pg/ml) | 3.3 ± 1.6 | 2.9 ± 1.5 | 1.8 ± 1.2 a,b |
1.49 (0.74–2.25), a < 0.001 1.06 (0.31–1.81), b = 0.004 |
<.001 |
| NLR | 1.5 ± 0.7 | 1.5 ± 0.6 | 1.1 ± 0.5 a,b |
0.48 (0.17–0.78), a = 0.001 0.42 (0.11–0.72), b = 0.004 |
<.001 |
- Data are shown as the mean ± standard deviation values. a: compared to Group C; b: compared to Group M.
3.3 Postoperative anxiety
The three groups had comparable anxiety scores preoperatively. However, the anxiety scores in the three groups were different at 2 h (p < .001) and 4 h (p < .001) postoperatively. In comparison with group C, anxiety in group D was significantly lower at 2 h (25.6 ± 2.6 vs. 30.1 ± 4.3, mean difference [95% CI]: 4.94 [2.99–6.88], p < .001) and 4 h (25.0 ± 2.4 vs. 28.0 ± 3.1, mean difference [95% CI]: 2.98 [1.21–4.74], p < .001) postoperatively. Anxiety scores were also much lower in group D than in group M at 2 h (25.6 ± 2.6 vs. 28.0 ± 3.9, mean difference [95% CI]: 2.88 [0.94–4.83], p = .002) and 4 h (25.0 ± 2.4 vs. 28.0 ± 3.1, mean difference [95% CI]: 3.27 [1.51–5.04], p < .001) postoperatively. There was no difference in postoperative anxiety scores between groups M and C (Table 3).
|
Group C (n = 40) |
Group M (n = 40) |
Group D (n = 40) |
Mean difference (95% CI) | p | |
|---|---|---|---|---|---|
| Preoperative interview | 27.1 ± 5.7 | 27.9 ± 3.2 | 28.0 ± 6.6 | .699 | |
| 2 h postoperative | 30.1 ± 4.3 | 28.0 ± 3.9 | 25.6 ± 2.6 a,b |
4.94 (2.99–6.88), a < 0.001 2.88 (0.94–4.83), b = 0.002 |
<.001 |
| 4 h postoperative | 28.0 ± 3.1 | 28.3 ± 4.2 | 25.0 ± 2.4 a,b |
2.98 (1.21–4.74), a < 0.001 3.27 (1.51–5.04), b < 0.001 |
<.001 |
- Data are shown as mean ± standard deviation values. a: compared to Group C, b: compared to Group M.
3.4 Postoperative pain
The three groups showed comparable postoperative pain scores at 2 h and 4 h postoperatively (Table 4). In group C, 2 children had pain scores of 5 points, and 1 child had a pain score of 4 points; in group M, 1 child each had pain scores of 5 and 4 points 2 h postoperatively. These patients were all given intravenous sufentanyl 0.05 μg/kg for pain relief. None of the children in three groups required rescue pain medication 4 h postoperatively.
|
Group C (n = 40) |
Group M (n = 40) |
Group D (n = 40) |
p | |
|---|---|---|---|---|
| 2 h postoperative | 1 (2) | 1 (1.75) | 1 (1) | .11 |
| 4 h postoperative | 1 (0) | 1 (2) | 1 (1) | .07 |
- Data are shown as the median (interquartile range) values.
3.5 Correlation between postoperative anxiety and postoperative inflammation
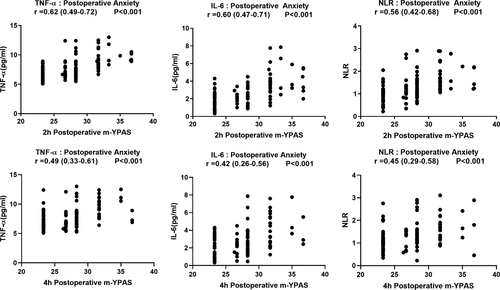
The anxiety scores of the three groups at 2 h postoperatively showed significant positive correlations with the plasma levels of TNF-α (r [95% CI]: 0.62 [0.49–0.72], p < .001) and IL-6 (r [95% CI]: 0.60 [0.47–0.71], p < .001) and the NLR (r [95% CI]: 0.56 [0.42–0.68], p < .001). The anxiety scores of the three groups at 4 h postoperatively also showed positive correlations with the plasma levels of TNF-α (r [95% CI]: 0.49 [0.33–0.61], p < .001) and IL-6 (r [95% CI]: 0.42 [0.26–0.56], p < .001) and the NLR (r [95% CI]: 0.45 [0.29–0.58], p < .001) (Figure 2).
4 DISCUSSION
Our study demonstrates that dexmedetomidine premedication results in lower postoperative plasma levels of TNF-α and IL-6 and NLR after same-day surgery in children, in comparison with regimens using midazolam or no premedication. The positive correlations between postoperative m-YPAS scores and TNF-α, IL-6 and NLR suggest that postoperative anxiety may be positively related to postoperative systemic inflammation.
Surgical procedures such as hernia repair elicit a systemic inflammatory response, which is characterized by increase in C-reactive protein, leukocytes, neutrophils, interleukin-1 (IL-1), IL-6, fibrinogen, and α1-antitrypsin, and decreases in lymphocytes and albumin.15 The current study shows that, in comparison with the other two groups, dexmedetomidine premedication significantly reduced postoperative TNF-α and IL-6 levels in children undergoing elective hernia repair surgery. This result is consistent with the findings of another study, in which dexmedetomidine was more effective than midazolam in reducing IL-6 and TNF-α levels 2 h and 4 h after drug administration in patients undergoing dental implant surgery.16 The mechanisms responsible for these actions may include dexmedetomidine suppressing the Toll-like receptor 4 (TLR4) / nuclear factor kappa-B (NF-κB) pathway and inhibiting nucleotide-binding oligomerization receptor domain–containing protein 3 (NLRP3) inflammasome and microglial cell activities in the hippocampus.17, 18 However, the effect of dexmedetomidine on neutrophils and lymphocytes remains controversial. One study found that dexmedetomidine suppressed the phagocytic activity of human neutrophils, which was associated with a respiratory burst coupled with NO production.19 However, no influence of dexmedetomidine on human neutrophil or lymphocyte functions during short-term incubation was found in vitro studies.20, 21 We did not observe an effect of dexmedetomidine on neutrophils or lymphocytes in this study, but we found that IV administration of 0.5 μg/kg dexmedetomidine could significantly reduce the ratios.
Humoral signals, particularly cytokines circulating in the blood (eg, TNF-α and IL-6), communicate with the CNS via circumventricular organs.22 Previous studies have demonstrated that a rapid increase in TNF-α and IL-6 levels is associated with a change in mood and behavior, which is strongly correlated with enhanced evoked responses to emotional facial expressions within the subgenual anterior cingulate cortex (sACC).23 The sACC is involved in mood changes, and it shows enhanced activity during depression.24 It also contains vagal fibers that secrete acetylcholine, which acts on alpha-7 nicotinic receptors on macrophages to induce downregulation of the secretion of inflammatory cytokines.25 NLR is considered one of the most sensitive markers to classify patients in terms of acute inflammation.26 A high NLR may also reflect an altered inflammatory balance within the CNS.27 Although lymphocyte and neutrophil counts after psychological interventions for anxiety and depression have been linked to patient behaviors, the underlying mechanisms are unclear.28 Collectively, these findings suggest that proinflammatory cytokines are likely to facilitate the development and maintenance of postoperative anxiety and negative behavior manifestations. This study shows that the postoperative anxiolytic effects of dexmedetomidine are positively associated with greater reductions in postoperative TNF-α and IL-6 levels and NLR values. The significant positive correlations of postoperative anxiety with TNF-α and IL-6 levels and the NLR provide evidence that reducing inflammatory cytokine release could play an important role in dexmedetomidine-mediated reduction of postoperative anxiety in children undergoing hernia repair. The immunosuppressive effect of dexmedetomidine premedication reduces the initial peak of inflammatory cytokines and protects the host from the systemic consequences of the primary injury, which may be one of the main reasons for the anxiolytic effects of dexmedetomidine at 2 h and 4 h postoperatively in children.
On the basis of these results, we conclude that postoperative anxiety and systemic inflammation are positively related. Further research is needed to determine whether there is a new potentially psychological or behavioral variable associated with postoperative systemic inflammation, which may be more complex since it will involve analyses of the multiple collinearities among psychological variables, inflammatory response, and other factors like pain behavior.
5 STUDY LIMITATIONS
This study had several limitations. First, the plasma concentrations of inflammatory factors were measured only at the end of the operation under anesthesia, and data for the preoperative baseline concentrations as well as the concentrations at 2 and 4 hours or later after surgery were not assessed. The lack of preoperative group differences in inflammatory factors was the basis for evaluating these results. The course of plasma levels over several hours/days after surgery might improve our understanding of the correlation between postoperative inflammation and postoperative anxiety. Second, the residual effects of dexmedetomidine on postoperative inflammation and anxiety may cause a bias, since the duration of surgery and follow-up was short. Third, we used the m-YPAS, which is not validated for postoperative anxiety in children, as no such validated scale is available. Fourth, we did not record the perioperative vital signs of children, nor did we record the concentration of sevoflurane used during the operation in this study. The possible influence of lower sevoflurane concentrations on the reduction in postoperative systemic inflammation cannot be completely ruled out and needs to be studied further. Finally, it is not known whether reduced anxiety attenuated the postoperative systemic inflammatory response in our study, or the decreased systemic inflammatory response reduced postoperative anxiety. Since correlation does not imply causation, the findings of this study only provide clues for future investigations.
6 CONCLUSIONS
Our study demonstrates that dexmedetomidine reduces the postoperative inflammatory cytokines in children undergoing same-day surgery; the positive correlations between postoperative anxiety and inflammation suggest that postoperative anxiety may be positively associated with postoperative systemic inflammation.
7 ETHICS APPROVAL
The study protocol was approved by the Research and Ethics Committee of Hunan Children's Hospital on September 25, 2016. The approval code number was HCHLL-2016–002.
CONFLICT OF INTEREST
The authors report no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data cannot be shared at this time as the data also form part of an ongoing study.