An approach to define newborns´ sniffing position using an angle based on reproducible facial landmarks
Funding information
BH was supported by an intramural AKF- grant (Angewandte Klinische Forschung; number E0327039) from the Faculty of Medicine, University of Tübingen.
Abstract
Background
The neutral or sniffing position is advised for mask ventilation in neonates to avoid airway obstruction. As definitions are manifold and often unspecific, we wanted to investigate the reliability and reproducibility of angle measurements based on facial landmarks that may be used in future clinical trials to determine a hypothetical head position with minimal airway obstruction during mask ventilation.
Methods
In a prospective single-center observational study, 2D sagittal photographs of 24 near-term and term infants were taken, with five raters marking facial landmarks to assess interobserver agreement of those landmarks and angle δ, defined as the angle between the line parallel to the lying surface and the line crossing Subnasale (Sn) and Porion’ (P’). Angle δ was assessed in sniffing (δsniff) and physiologic (δphys) head position, the former based on a published, yet poorly defined head position where the tip of the nose aligns to the ceiling with the head in a supine, relaxed mid-position.
Results
Infants had a mean (SD) gestational age of 37.3 (2.3) weeks. Angle δ could be determined in all 48 images taken in either the sniffing or the physiological head position. Interobserver correlation coefficient was 98.6 for all measurements independent of head position. Angle δsniff was 90.5° (5.7) in the sniffing position.
Conclusions
This study provides a new measuring technique using an angle that is reproducible and reliable and may be used in future studies to correlate head position with airway obstruction.
What is already known about the topic
- Sniffing position is performed for years and differs widely within clinicians.
- Relationship between head position and airway obstruction remains unclear.
What new information this study adds
- A standardized angle defining infant's head position.
- This study provides a new measuring technique to examine the variation among clinicians and further correlate head position with airway obstruction.
1 BACKGROUND
About 10% of neonates require positive pressure ventilation (PPV) in the delivery room.1 Lung aeration is the critical first step to allow transition from fetal to postnatal circulation.2 If an infant is apneic, gasping, or breathing insufficiently, neonatal resuscitation guidelines recommend drying the newborn and to provide PPV in case of persistent apnea or bradycardia by using a facemask.3 A correct head position as recommended in resuscitation guidelines is important to avoid airway obstruction (AO) when using such masks, otherwise leading to inefficient ventilation and lung aeration.4 AO is common during the first two minutes of PPV; brief obstructions occurred in 25% of late preterm infants during PPV in the delivery room, which correlated with a higher rate of intubation.5, 6 Besides other reasons for ineffective ventilation such as mask leak,7, 8 AO can be caused by incorrect head position during mask ventilation,9 increased downward pressure on the facemask,10 a predominantly closed larynx immediately after birth during persistent apnea,11 laryngospasm,12 congenital abnormalities like retrognathia,13 or simply AO due to meconium stained fluid.14
An incorrect head position during mask ventilation9 might also contribute to airway obstruction.
The sniffing or neutral position, advised by European Resuscitation Guidelines as being the best position during neonatal mask ventilation,15 was first described in 189516 as a neck flexion with upper cervical extension,17, 18 but without any further detail on exactly what to achieve. Variations of the sniffing position have been used by clinicians for years and are mainly based on expert opinion19; yet a detailed definition of the angle used to unify its application is missing and may be a first step in addressing this omission.20
Up to now, there is only one study in spontaneously breathing yet sedated neonates receiving magnetic resonance imaging (MRI) that showed that the sniffing position was best to open up the airway, defined by an angle at the back of the head based on landmarks, in particular the head tilt angle, which is the angle between the occipito-ophisthion line and the ophisthion-C7-spine process line only visible on sagittal MR scans21 (Figure 1). MRI, however, is time-consuming and expensive; thus, a simple, easily obtainable and reproducible angle is needed.
The aim of this trial was to objectively define infants head positioning using facial landmarks, since positioning of the head is the most important measure to enable ventilation of the lungs.
For this purpose, we determined facial landmarks and created a simple angle measurement using 2D images that are easily reproducible by different observers in different head positions.22
This angle can be used in future studies to examine the variation among clinicians in trying to achieve an optimal head position and define the latter while avoiding airway obstruction during mask ventilation.20
2 MATERIAL AND METHODS
2.1 Study design and consent
This single-center, prospective observational study took place at Tuebingen University Children's Hospital, Germany. The institutional Ethics Committee approved the study, and written informed parental consent was obtained (approval number: 704/2017BO1).
2.1.1 Patients, equipment, and outcome
Infants born between 34 and 41 weeks gestation were eligible within 48 to 72 hours of birth. Exclusion criteria were dysmorphic features or the need for respiratory support. Demographic details including gender, gestational age (GA), head circumference, mode of delivery, and birth weight were obtained from the hospital notes.
Two lateral 2D images were taken using a Nikon D7100 camera (Nikon, Chiyoda, Tokio, Japan). A plastic scale (sliding millimeter caliper, Maped®, Cedex, France) was placed on the side of the infant's head as a measurement reference. ImageJ software (National Institute of Health; USA), a public domain, java-based image processing tool developed at the National Institutes of Health, was used for analysis.23
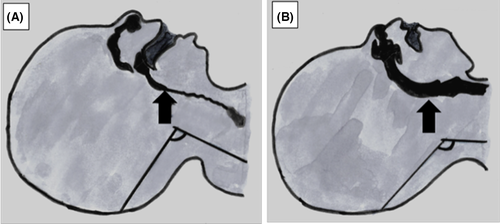
We focused on the following two landmarks based on AM Schwarz's concept of facial profiles (Figure 2)22: Subnasale (Sn) and Porion’ (P’) (defined as the midpoint of the upper contour of the external auditory canal on the soft tissue). The angle we focused on is called δ and is defined as the angle the line parallel to the lying surface and the line crossing the landmark Sn and P’ (Figure 2A,B).

To ensure that the new landmarks and angle were reliable and reproducible, five different observers individually and independently marked the two different anatomical landmarks Sn and P’ (Figure 2) on each of the 48 2D images using ImageJ software.23, 24
The five observers (physicians) had no experience in using ImageJ software or similar software or regarding special anthropology; they only received a short introduction to the software.
Each infant was photographed in two head positions: the “physiologic” and the “sniffing” position and the angle δphys, respectively, δsniff were calculated using the above-mentioned landmarks. Sniffing position was defined as the head position where the tip of the nose aligned to the ceiling 25 and physiologic position as the head positioned attained in a supine, relaxed mid-position. The underlying surface was standardized in each infant (Babytherm 8010, Draegerwerk®, Luebeck, Germany).
Both head positions were performed by a single physician. We used the same lens in all photographs. The distance between camera and patient varied between captures. We placed a plastic lineal on the infants’ side of the head to ensure measurements on the 2D images remained accurate.
Figure 2A shows an infant´s head in the supine, relaxed (physiologic) mid-position, while Figure 2B shows the same infant with its head in supine, sniffing mid-position.
To evaluate whether GA influences angle δ, patients were divided into near-term (34 to 37 weeks’ gestation) and term infants (≥ 37 weeks’ gestation).
2.2 Statistical analysis
A convenience sample of 24 infants was chosen for this pilot study. An intraclass correlation coefficient with a one-way model was used to calculate intra-rater and inter-rater reliability, respectively.
A P-value (two-sided) of <.05 was considered to represent statistical significance.
Continuous data are shown as mean ±SD if normally distributed or median (IQR) if skewed. Mean differences are shown with 95% confidence intervals. Categorical data are summarized as counts and percentages. As data were normally distributed, Pearson's correlation coefficient was used. Normally distributed variables were analyzed using t test, otherwise the Mann-Whitney U test was used. For paired samples, the paired t test or Wilcoxon signed-rank test was used.
All statistical analyses were performed using SPSS (version 25, SPSS Inc, Chicago, Ill).
3 RESULTS
One single physician adjusted the sniffing and physiological positions to generate a total of 48 images of 24 near-term (n = 13) and term (n = 11) infants with a mean (SD) gestational age of 37.3 (2.3) weeks, which were recruited between April and November 2018. Infants´ demographics are shown in Table 1. All 2D images were performed between 48 and 72 hours after birth, and no infant had visible head shape deformities.
| Characteristics | All (n = 24) | Near-term (n = 13) | Term (n = 11) |
|---|---|---|---|
| Birth weight (g) | 2883.8 (720.9) | 2366.1 (383.6) | 3495.5 (508.7) |
| Gestational age (weeks) | 37.3 (2.3) | 35.5 (0.7) | 39.5 (1.2) |
| Head circumference (cm) | 33.6 (2.3) | 32.4 (1.8) | 35 (1.9) |
| Male (%) | 12 (50%) | 6 (46%) | 6 (54%) |
| Twins (%) | 6 (25%) | 6 (46%) | 0 |
| Cesarean section (%) | 13 (54%) | 7 (54%) | 6 (54%) |
| Caucasian (%) | 22 (92%) | 11 (92%) | 11 (100%) |
Note
- Data of 24 infants are shown as mean (SD) or counts (percentages).
Two landmarks were placed in every image; altogether, 2 variables in 48 images were evaluated per observer (Figure 2). The interclass correlation coefficient of average measures was 99.8 with no statistically significant differences between measurements (p > 0.05). There was a homogenous distribution of the results for all raters indicating that these were placed almost identically by all five observers. No observer experienced any difficulties in placing the landmarks. When evaluating the accuracy and repeatability of the different landmarks, both had the same strength.
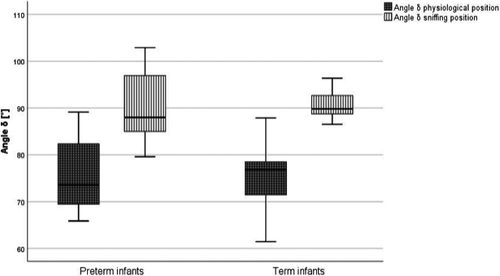
Mean δphys was 75.7° (8.0) and mean δsniff 90.5° (5.7), yielding a mean difference of 14.8° (95% CI; −17.6–−11.9), (p < 0.001).
There were no significant differences between near-term and term infants in measured angle δphys [76.1°(7.9) vs 75.3°(8.3);(p = 0.8)] or δsniff [90.5° (7.4) vs 90.6° (2.9); (p = 0.8)] (Figure 3).
4 DISCUSSION
The correct head positioning might be one of the simplest ways to reduce or even avoid airway obstruction.
Until now, however, different variations of the sniffing position are performed by clinicians 20 because a reliable and reproducible description of the sniffing position is missing. This study may be a first step addressing this omission.
There are several recommendations on how to achieve the sniffing position, for example, by placing a roll under the infant's neck26 or shoulder27 to compensate for its large occiput. Illustrations and descriptions of the sniffing position in the literature differ widely.28 This is the first study using visible facial angle measurements of facial landmarks to describe and define an infant's head position using sagittal photographs. Easy and reliable outer landmarks, such as Subnasale and Porion’, were used to calculate angle δ, which accurately describes an infant's head position and helps to perform further investigations about the relationship of head position and airway obstruction. The landmarks used in the study are well-defined,22 and there was a high intra- and inter-rater reliability in placing them, indicating that they are simple, reproducible, and precise. Using the ear and in this case Porion’ as landmarks might be debatable as this may have high interindividual variability. Data, however, refute this assumption, showing that all infants have a similar bitragial-subnasal axis if they do not suffer from a syndromic disorder of facial dysmorphia29 and it is also used for other well-established lines, for example, the Frankfort horizontal (FH).
The FH is well-defined as the line passing through the infraorbital point (the low point on the lower margin of the orbit on a human skull or head) and porion30 and is considered a reliable basis for clinical cephalometric analysis.31
It has been used to describe sniffing position in spontaneously breathing adults and is angled at 70–80° to the horizontal plane of the underlying surface.32
The infraorbital point for generating the FH would be covered by the rim of a facemask, while the porion as an anatomical landmark is constantly visible through a transparent facemask during mask ventilation.
We therefore aimed for a clearly visible anatomical landmark, while using the newly defined angle δsniff in sniffing position by creating an orthogonale that is easy to estimate.
Our observational study may offer a method to unify the definition of the sniffing position and replacing nonmeasurable terms like “complete atlanto-occipital extension”33 or “placing the infants with his/her eyes looking directly at the ceiling” or “with the nose pointed upward and forward”25 by providing a detailed and reliable angle to describe and evaluate an infant's head position. Our new and clearly defined angle δ may be used to validate the “sniffing position” as being the best position during mask ventilation in newborns. Obtaining the optimal head position for avoiding airway obstruction is fundamental for ventilation of the lungs.
One of the strengths of this study is that all raters had no previous experience in setting landmarks, indicating that the chosen landmarks are reproducible, and the calculated angle δ can be measured with high precision.
Since the aim of this study was only to determine landmarks that can be used to reliably define infants’ head position, our study population should represent a rather healthy and normal population. We therefore did not include any patients with head shape anomalies or extreme premature infants. Moreover, there was no difference in angle measurements between near-term and term infants, which confirms once again the quality of the anatomical landmarks to determine angle δsniff.
A limitation of our study is that there may be difficulties in seeing the anatomical landmark subnasale if a facemask covers the infant´s mouth and nose. Fisher & Paykel (F&P Healthcare, Schorndorf, Germany), for example, offers transparent facemasks, and the landmark Sn is sufficiently visible. Using anatomical or round facemasks with cushion rim or masks of the VBM brand (VBM, Medizinprodukte, Sulz, Germany), for example, it might be challenging to see the landmark due to the lack of translucency.
Limitations of our study include that the sniffing position was always performed by the same investigator, which might have contributed to the small standard deviation.
Nevertheless, we did not yet investigate different clinicians’ performance in assuming a so-called “sniffing position,” although it unquestionably varies greatly between clinicians. With the current evidence, it remains unclear which angle δsniff will be the best to avoid airway obstruction during mask ventilation. We are therefore planning a clinical study to determine the correlation between angle δsniff and the degree of airway obstruction during mask ventilation. At present, we can just speculate that both, head elevation and head extension, can decrease upper airway collapsibility during mask ventilation. Airway obstruction is common during ventilation in the delivery room during neonatal resuscitation.6 Adverse events like airway obstruction can be identified by a calorimetric CO2 detector6 or a respiratory function monitor (RFM), which displays a characteristic AO-associated flow pattern9 and might provide a guidance for finding the optimal angle δsniff. A zero inspiratory or expiratory flow,34 respectively, a zero/very small tidal volume (Vt) on the RFM during inflation, should be considered either as being due to an external (facemask pressure) or internal (head position) airway obstruction.9 Measuring angle δsniff is intended to describe an external airway obstruction but will remain a research tool providing valuable information about the optimal head position, which might lead to recommendations that are easy to perform during neonatal resuscitation.
5 CONCLUSION
A standardized angle defining an infant's head position can be used in future studies to examine the variation among clinicians in trying to achieve the optimal head position associated with minimal airway obstructions.
6 ETHICS APPROVAL
The research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. The institutional Ethics Committee of the University of Tuebingen approved the study (approval number: 704/2017BO1). All parents have given their written informed consent. Parental consent for publication of the photographs has been provided.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
AUTHOR CONTRIBUTIONS
BH was involved in study design, patient recruitment, data collection and analysis and has written the manuscript. AMB was involved in study design, patient recruitment, data collection and analysis and has also reviewed and contributed to each draft of the manuscript. LS was involved in study design and has reviewed and contributed to each draft of the manuscript. CFP was involved in study design and contributed to each draft of the manuscript. BK did the project supervision and has seen and contributed to each draft of the manuscript. All authors participated in critical revision of the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects to the work.
Open Research
DATA AVAILABILITY STATEMENT
In accordance with the “DFG Guidelines on the Handling of Research Data,” we will make all data available upon request. The data set will be archived for at least 10 years after publication.