Cerebral autoregulation in infants during sevoflurane anesthesia for craniofacial surgery
Abstract
Background
Data on cerebral pressure-flow autoregulation in the youngest children are scarce. We studied the correlation between mean arterial pressure and cerebral tissue oxygen saturation (rSO2) by near-infrared spectroscopy (NIRS) in patients undergoing nose, lip, and palate surgery.
Aim
We tested the hypothesis that cerebral pressure-flow autoregulation is impaired in children less than 1 year undergoing surgery and general anesthesia with sevoflurane under controlled mechanical ventilation.
Method
After approval from the Ethical board, 15 children aged <1 year were included. Before anesthesia induction, a NIRS sensor (INVOSTM, Medtronic, Minneapolis, USA) was placed over the cerebral frontal lobe. Frontal rSO2, a surrogate for cerebral perfusion, mean arterial pressure, end-tidal CO2- and sevoflurane concentration, and arterial oxygen saturation were sampled every minute after the induction. A repeated measures correlation analysis was performed to study correlation between mean arterial pressure and cerebral rSO2, and the repeated measures correlation coefficient (rrm) was calculated.
Results
Fifteen patients, aged 7.7 ± 1.9 months, were studied. rSO2 showed a positive correlation with mean arterial pressure ([95% CI: 9.0-12.1], P < 0.001) with a moderate to large effect size (rrm = 0.462), indicating an impaired cerebral pressure-flow autoregulation. The slopes of the rSO2-mean arterial pressure correlations were steeper in patients who were hypotensive (mean arterial pressure <50 mm Hg) compared to patients having a mean arterial pressure ≥50 mm Hg, indicating that at lower mean arterial pressure, the cerebral pressure dependence of cerebral oxygenation is even more pronounced.
Conclusion
During sevoflurane anesthesia in the youngest pediatric patients, cerebral perfusion is pressure-dependent, suggesting that the efficiency of the cerebral blood flow autoregulation is limited.
What is already known
- Near-infrared spectroscopy (NIRS) is a well-established technology used to estimate cerebral oxygenation.
- The use of NIRS in the youngest pediatric patients is limited, and there is a lack of data on cerebral pressure-flow autoregulation in infants.
What this article adds
- During surgery and anesthesia in pediatric patients <1 year of age, cerebral perfusion is pressure-dependent, suggesting impaired cerebral blood flow autoregulation.
- At mean arterial pressures below 50 mm Hg, the relationship between cerebral oxygenation and blood pressure is more pronounced, indicating an increased risk of cerebral hypoxia.
1 INTRODUCTION
In adults, cerebral blood flow is maintained constant, during normocapnia, within a range of mean arterial pressure (MAP) of 60-160 mm Hg.1 Outside this range, cerebral blood flow will become pressure-dependent. In pediatric patients, there is an incomplete comprehension of cerebral pressure-flow autoregulation during anesthesia and surgery. A MAP below the lower limit of pressure-flow autoregulation results in a pressure-dependent flow with a risk of intraoperative cerebral ischemia. The lower limit of pressure-flow autoregulation is not well defined in pediatric patients, particularly not in patients <1 year of age.2
Data on cerebral blood flow autoregulation in pediatric patients during anesthesia and surgery are scarce and somewhat controversial. Vavilala et al studied patients with a mean age of 1.1 up to 13 years of age and found no age-related differences in the cerebral autoregulatory capacity.3 In children with traumatic brain injury, Freeman et al found that the incidence of impaired cerebral autoregulation was higher in the younger patients (<4 years of age) than older (≥4 years) children.4 Brady et al studied cerebral pressure-flow autoregulation in pediatric patients undergoing cardiac surgery with cardiopulmonary bypass by cerebral oximetry for assessment of regional cerebral oxygenation (rSO2) using near-infrared spectroscopy (NIRS) as a surrogate for cerebral blood flow.5 Hypotension was associated with lower rSO2, but there was no association between the lower limit of autoregulation and age.
There are few studies on cerebral pressure-flow autoregulation in our youngest pediatric patients (<1 year of age). In the present study, we therefore studied the correlation between MAP and cerebral regional tissue oxygen saturation (rSO2) during steady-state sevoflurane anesthesia in infants <1 year of age undergoing cleft lip and/or palate surgery. Near-infrared spectroscopy (NIRS) was used as a surrogate for regional cerebral perfusion (cerebral rSO2).6 Our hypothesis was that the cerebral pressure-flow autoregulation was impaired in this pediatric population.
2 METHODS
This is prospective single-center, non-invasive, observational study. After ethics committee approval, written and informed consent was obtained from parents/guardians. Between June 2017 and April 2018, 20 children <1 year of age, ASA 1–2, scheduled for treatment with cleft lip and/or palate surgery under general anesthesia, were eligible. Exclusion criteria included children with (i) a history of an abnormal airway, (ii) a reactive airway disease, (iii) an upper respiratory tract infection in the preceding 3 weeks, (iv) an abnormal cognitive development, (v) a developmental delay, and (vi) a known history of allergic reactions to the drugs in our protocol. The study was performed at the Sahlgrenska University Hospital, Gothenburg in accordance with applicable laws and regulations, good clinical practice and the Declaration of Helsinki. The study was registered in the ClinicalTrial.gov, PRS, D.nr 106-17. NCT03136952.
All patients were premedicated fifteen minutes before entering the operating room with midazolam (0.3 mg/kg) and atropine (0.15 mg) rectally. In the operating room, the patients were induced with 3-8% sevoflurane (n = 15) in oxygen via face mask or with intravenous propofol (3-6 mg/kg, n = 1). After loss of consciousness, all children received a bolus dose of fentanyl, 2 μg/kg. Sixty seconds after administering the fentanyl, rocuronium 0.4/mg/kg was given, and 60 seconds thereafter, the patients were orally intubated. After intubation, betamethasone (200 ug/kg) was administered intravenously to prevent postoperative nausea. The target end-tidal level of sevoflurane for maintenance of anesthesia was 2.8%-3.6%. Tidal volume was adjusted to receive and end-tidal (ET) carbon dioxide (ETCO2) level between 5.0 and 5.4 kPa with a PEEP of 2-5 H2O cm H2O. A balanced crystalloid solution was administered at a rate of 10 ml/kg during the first hour followed by maintenance infusion rate of 2-4 ml/kg per hour to achieve and maintain hemodynamic stability. The target mean arterial pressure was >40 mm Hg or >75% of the pre-induction value. Opioid administration and titration were initiated before extubation depending on respiratory rate and ETCO2.
All patients were monitored with near-infrared spectroscopy (NIRS, Medtronic INVOS™) with sensors placed on the frontal head, to measure regional tissue oxygenation (rSO2). Baseline values (rSO2, HR, oxygen saturation) were recorded 4-5 minutes before induction of anesthesia. Values of rSO2 oxygen saturation, HR, ETCO2, rectal temperature, and ET sevoflurane were recorded every minute. Noninvasive blood pressure was obtained every 5 minutes. Data were recorded until the completion of surgery and the discontinuation of sevoflurane administration.
2.1 Statistical analysis
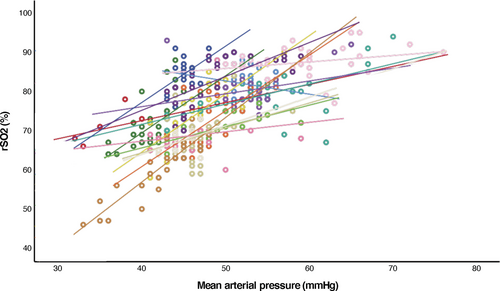
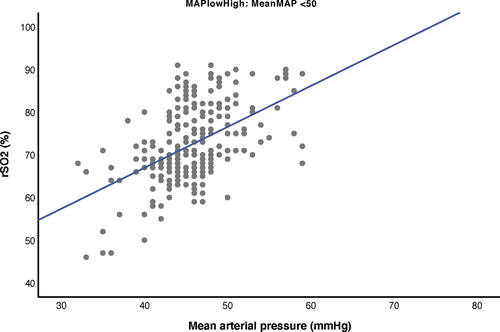
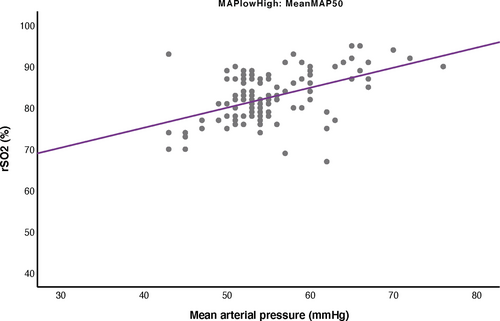
Statistical analyzes were performed using SPSS version 24.0 software (IBM, Chicago, IL). Descriptive statistics are presented in number, (%), median, and mean ± SD. A repeated measures correlation plot was constructed for each patient. A repeated measures (rm) correlation analysis7 was performed to correlate paired data of MAP and rSO2. To assess the strength of the linear relationship between MAP and rSO2, the repeated measures correlation coefficient (rrm) was calculated.7 Individual plots of rSO2 and MAP were made, and the slope of the regression lines was calculated. Furthermore, the patients were divided into two groups, based on a mean MAP <50 mm Hg (low group) or MAP ≥50 mm Hg (high group), respectively, during the surgical procedure. For these two groups, rrm and the mean slope of the regression line were calculated and a statistical difference between the two groups was tested with a Mann-Whitney U test. A P < 0.05 was considered statistically significant.
3 RESULTS
A total of 20 children were initially enrolled but three patients were excluded due to organizational reasons and two patients declined to participate. The age, weight, physical status, and other demographic data are presented in Table 1. The mean age was 7.7 ± 1.9 months, and mean body weight was 8.3 ± 0.9 kilogram. The patients underwent nose/lip surgery (n = 5) palate surgery (n = 5) and combined procedures (n = 5).
| Gender, M/F | 10/5 |
| Nose/Lip surgery | 5 |
| Palate surgery | 5 |
| Combination surgery | 5 |
| Age (mo)a | 7.7 ± 1.9 (5-11) |
| Weight (kg)a | 8.3 ± 0.9 (6.8-10) |
| Recorded time (min)b | 153 (86-217) |
- Abbreviations: M/F: Male/Female; Combination surgery: Combination of Nose/Lip and Palate surgery (n).
- a Mean ±SD (Min-Max).
- b Median (Min-Max).
Data on SpO2, ET-CO2, ET sevoflurane, heart rate, arterial blood pressure, body temperature hemoglobin, bleeding, and fluid administration are shown in Table 2. Intraoperative bleeding was less than 2% of estimated blood volume (n = 15). However, one child had a bleeding of approximately 7% of the estimated blood volume (Table 2). None of the patients were treated with a vasopressor during the surgical procedure. ET sevoflurane was 2.95 ± 0.50, and ET-CO2 was 5.0%-5.5% during the surgical procedure.
| Monitoring | Mean | SD± |
|---|---|---|
| SpO₂ (%) | 99 | ±1 |
| Fraction inspired O₂ (%) | 39 | ±14 |
| End-tidal O₂ (%) | 33 | ±11 |
| End-tidal CO₂ (kPa) | 5.1 | ±0.4 |
| Heart rate (beats/min)) | 132 | ±13 |
| Systolic blood pressure (mm Hg) | 76 | ±10 |
| Diastolic blood pressure (mm Hg) | 39 | ±6 |
| Mean arterial pressure (mm Hg) | 49 | ±7 |
| Rectal temperature (C°) | 36.9 | ±0.6 |
| Hemoglobin (g/L) | 105 | ±3 |
| Accumulated Bleeding (ml) | 12 | ±14 |
| Accumulated Fluid (ml) | 149 | ±37 |
| End-tidal Sevoflurane (%) | 3.0 | ±0.5 |
| Sevoflurane MAC | 1.1 | ±0.5 |
- Abbreviations: SpO₂: peripheral capillary oxygen saturation; O₂: oxygen; CO₂: Carbon dioxide.
The mean number of MAP/NIRS recordings was 25 ± 9 (mean±SD) (range 6-39). At baseline, rSO2 was 70 ± 5 (63-82) and MAP was 49 ± 7 (32-76) mm Hg. Eleven patients had mean MAP <50 mm Hg during surgery (mean 46 ± 5) and were included in the low MAP group, and 4 patients had a mean MAP of >50 mm Hg during surgery (mean 55 ± 6) and were included in the high MAP group. The mean ET sevoflurane concentration was 3.0 ± 0.04 and 2.9 ± 0.02 in the high and the low MAP group, respectively ([95% CI: 0.05-0.19], P < 0.001). Cerebral rSO2 showed a significant positive correlation with MAP ([95% CI: 9.0-12.1], P < 0.001) with a moderate to large effect size (rrm = 0.462, Figure 1), suggesting a pressure-dependent cerebral perfusion, indicative of an impaired cerebral pressure-flow autoregulation (Figure 1). The mean regression slope of the correlation lines was 0.77 ± 0.59%/mm Hg (range −0.34 to 1.65). The individual repeated measures correlation plots from patients in the low or high MAP groups are shown in Figures 2 and 3, respectively. The rrm was 0.608 for the low MAP group (P < 0.001, n = 11) and 0.368 (P < 0.001, n = 4) for the high MAP group, that is, there was a stronger linear correlation between rSO2 and MAP in the hypotensive group. The mean regression slopes of the low and the high MAP groups were 0.995 ± 0.50%/mm Hg (range: 0.24-1.65) and 0.167 ± 0.37%/mm Hg (range: −0.34 to 0.52), respectively (P = 0.010).
4 DISCUSSION
4.1 Key findings
The main findings of the present study on infants undergoing cleft lip and/or palate surgery were that cerebral rSO2 correlated positively with MAP, suggesting a pressure-dependent cerebral perfusion indicative of an impaired cerebral pressure-flow autoregulation in pediatric patients younger than 1 year of age. The slopes of the repeated measures correlation plots, correlating MAP to rSO2, were more pronounced (=steeper) in patients who were hypotensive (mean MAP <50 mm Hg) compared to patients having a mean MAP >50 mm Hg, during the surgical procedure, indicating that at lower MAP, the cerebral pressure-flow autoregulation may be particularly impaired.
To our knowledge, this is the first study evaluating the cerebral pressure-flow autoregulation in the youngest pediatric patients during surgery and general anesthesia. The study highlights the importance of maintaining MAP intraoperatively at a level above 50 mm Hg not to jeopardize cerebral perfusion, as the cerebral pressure-flow autoregulation may be severely affected at MAP´s below 50 mm Hg, or rather, that it is below the autoregulatory range. When MAP is maintained at a level <50 mm Hg, a certain fall in MAP causes a 34% decrease in rSO2, while a similar decrease in MAP will only decrease rSO2 by 6% when MAP is maintained at a level >50 mm Hg. Thus, at a certain decrease in MAP, the relative fall in rSO2 is almost 4 times greater when MAP is maintained at hypotensive levels.
Data on cerebral blood flow autoregulation in pediatric patients undergoing anesthesia and surgery are scarce and somewhat controversial. Vavilala et al compared the dynamic autoregulatory response between conscious healthy adolescents (12-17 years) and adults (25-45 years) and found that the dynamic autoregulatory response to sudden short-lasting blood pressure drops was impaired in adolescents. Using a steady-state method of cerebral autoregulation, the same group studied patients with a mean age of 1.1 up to 13 years of age during low-dose sevoflurane anesthesia.3 The authors found no age-related differences in the cerebral autoregulatory capacity, not even when comparing children and adults. However, in that study, the effectiveness of cerebral autoregulation was tested only at MAP:s above baseline, awake MAP, by infusion of a vasopressor. Furthermore, the number of included patients less than 1 year was limited. In children with traumatic brain injury, cerebral autoregulation between young (<4 years of age) and older (≥4 years) children was compared.4 The incidence of impaired autoregulation was higher in the younger group with worse outcome than the older group. Brady et al studied cerebral pressure-flow autoregulation in pediatric patients with a mean age of 4.5 years undergoing cardiac surgery with cardiopulmonary bypass by cerebral oximetry for assessment of regional cerebral oxygenation (rSO2) using near-infrared spectroscopy (NIRS) as a surrogate for cerebral blood flow.5 Hypotension was associated with lower rSO2. They found that the lower limit of autoregulation was 42 ± 7 mm Hg but there was no association between the lower limit of autoregulation and age.
Our data are in line with the results from the study by Hayashida et al.8 They studied 65 children aged between 5 months and 17 years undergoing corrective cardiac surgery using cardiopulmonary bypass (CPB). Sixteen patients were aged <1 year. They determined the slopes of the regression lines correlating rSO2 to MAP both before and during CPB. They found that rSO2 was correlated to MAP in the younger child both before and during CPB, while in the older children, there was no correlation between MAP and rSO2 either during CPB or during the prebypass period, suggesting that younger patients (<4 years of age) have a poor cerebral pressure-flow autoregulation. They also demonstrated that children less than 4 years of age were more prone to develop cerebral ischemia during hypotension.
The notion that cerebral pressure-flow autoregulation is impaired in younger pediatric patients is supported by studies in normoterm and preterm infants. Lou et al measured the cerebral blood flow with the 133xenon clearance technique early after birth in distressed infants.9 They found a strong linear correlation between mean arterial pressure and cerebral blood flow, suggesting that autoregulatory capacity was lacking. Jorch and Jorch studied the relationship between MAP and the blood flow velocity in the internal carotid artery in neonates and found a loss of autoregulation in 16 of 23 patients at a gestational age of 31 weeks.10 Tsuji et al11 monitored fronto-parietal NIRS and arterial blood pressure in critically ill preterm infants, at a gestational age of 23-31 weeks and found that cerebral autoregulation was impaired in 53% of the patients.
In all patients, in the present study, anesthesia was maintained with sevoflurane, which has intrinsic vasodilatory properties and could therefore potentially have affected the cerebral pressure-flow autoregulation in the present study. However, previous studies in adult patients have shown that the static cerebral pressure-flow autoregulation is intact during sevoflurane anesthesia, suggesting that the intrinsic cerebral vasodilatory effect of sevoflurane does not seem to be profound.12-14 Only at high doses of sevoflurane, inducing electroencephalographic burst-suppression, cerebral vasodilation is induced, which impairs cerebral pressure-flow autoregulation.15 One could argue that the more pronounced positive linear correlation between MAP and rSO2 in the hypotensive group could be explained by a deeper anesthesia level in this group. However, there was no difference in ET sevoflurane concentration when comparing the high and low MAP groups.
One major limitation is the relatively small sample size. Furthermore, we did not measure arterial blood pressure and NIRS while awake, before induction of anesthesia, as we did not want to stress the child before the induction of anesthesia. In addition, the pressure-flow autoregulation should optimally have been studied under a constant arterial pCO2 and at a constant inhaled concentration of sevoflurane, as these variables may both affect the cerebral autoregulatory response.
5 CONCLUSIONS
In the present study on pediatric patients less than 1 year undergoing cleft lip and/or palate surgery, we studied the relationship between mean arterial pressure (MAP) and the fronto-parietal NIRS signal (cerebral rSO2) during the surgical procedure. There was a positive linear correlation between MAP and rSO2 indicating impaired cerebral pressure-flow autoregulation. Mean arterial pressures below 50 mm Hg may be below the autoregulatory range, making the pressure dependence of cerebral oxygen delivery more pronounced.
ACKNOWLEDGEMENT
The authors express their gratitude to Till Rudolph MD, for his help to anesthetize some of the studied children at Department of Anesthesiology and Surgery and Intensive Care Medicine, University Hospital Sahlgrenska in Gothenburg, Sweden.
CONFLICT OF INTEREST
None.
AUTHOR CONTRIBUTIONS
Pether Jildenstål, Sven-Erik Ricksten, and Lukas Lannemyr involved in study concept and design. Pether Jildenstål, Daniel Widarsson Norbeck, Sven-Erik Ricksten and Lukas Lannemyr involved in analysis and interpretation of data. Pether Jildenstål, Sven-Erik Ricksten, Johan Snygg, and Lukas Lannemyr drafted the manuscript. Pether Jildenstål, Sven-Erik Ricksten, Daniel Widarsson Norbeck, Johan Snygg, and Lukas Lannemyr. Zahler critically revised the manuscript for important intellectual content. NA obtained funding. Pether Jildenstål, Sven-Erik Ricksten, and Lukas Lannemyr supervised the study.
ETHICAL APPROVAL
No. 106-17, March 9 2017, ClinicalTrial.gov, PRS, D.nr 106-17. NCT03136952.
Open Research
DATA AVAILABILITY STATEMENT
Author elects to share data. Research data are available at reasonable request.