Modular Femoral Stem for Hartofilakidis Type C Hip Dysplasia: Is It Necessary for 1-mm Increment of Distal Stem Diameter?
Funding: This work was supported by Beijing Natural Science Foundation, L234011; National Natural Science Foundation of China, U22A20355.
Jiafeng Yi and Hongbin Xie contributed equally to this manuscript.
ABSTRACT
Background
S-ROM prosthesis, one well-used femoral prosthesis in the patients with developmental dysplasia of the hip (DDH), has a skipping size of the distal stem diameter. The purpose of this study was to investigate whether its 2-mm incremental diameter could meet clinical needs for high-riding DDH patients.
Methods
Between July 2018 and December 2022, the Hartofilakidis type C DDH patients with S-ROM stem (9 or 11 mm) were retrospectively enrolled according to the inclusion criteria and exclusion criteria in our institute. The intraoperative femur fractures, the diameter of the femoral medullary cavity, the canal filling ratio of the S-ROM stem, the closure conditions of the stem slot, and the healing rate of subtrochanteric osteotomy were analyzed to evaluate the effect of stem design on clinical outcomes. Statistical analyses were conducted using independent samples t-tests, chi-square test, and logistic regression analysis with a significance threshold of p < 0.05.
Results
A total of 95 patients (109 hips) were included in this study, including 60 hips with 9 mm S-ROM and 49 hips with 11 mm S-ROM. Compared with the 9 mm S-ROM group, the 11 mm S-ROM group presented nearly 5 times the intraoperative fracture rate (16.3%, 3.3%, p < 0.05). The mean diameter of the femoral medullary cavity in the 9 mm S-ROM group was 0.84 ± 0.20 mm and in the 11 mm S-ROM group was 1.03 ± 0.18 mm. The canal filling ratio in the 9 mm S-ROM group is significantly lower than that of the 11 mm S-ROM group. In the 11 mm S-ROM group, the filling ratio of the femoral medullary cavity of fracture hips was significantly higher than that in non-fracture hips.
Conclusion
The S-ROM design with a distal stem diameter increment of every 2 mm would increase the risk of intraoperative periprosthetic femoral fractures in high-riding DDH patients. It is necessary for a 1-mm increment of distal stem diameter in such patients.
Level of Evidence
Level III, retrospective comparative study.
1 Introduction
Hartofilakidis type C developmental dysplasia of the hip (DDH), characterized by high dislocation of the proximal femur and narrow femoral canal, posed great challenges upon total hip arthroplasty (THA) [1]. Modular S-ROM prostheses have been widely used in THA for high-riding DDH because of their anatomical adaptability to adjust the femoral canal morphology and anteversion angle [2]. They have shown excellent survivorship in long-term follow-up [3, 4]. However, intraoperative periprosthetic femoral fractures were still a prominent problem in DDH patients [5, 6].
Due to the larger skeletal size of European and American DDH patients, the 2 mm incremental design of the S-ROM prosthesis poses minimal challenges for them. However, smaller skeletal frames, anatomical variations of the femoral canal, and poorer bone quality in some Asian DDH patients make it difficult to select compatible prostheses. Japanese researchers developed the S-ROM-A prosthesis, with a femoral stem diameter in every 1-mm increment, to better accommodate Asian DDH patients. However, according to our survey, this type of prosthesis is rarely available in other regions with a high incidence of DDH, such as China and Turkey.
To date, there have been no related studies on the impact of this design on surgery. Therefore, we carried out this study to explore the following two points: (i) whether the 2-mm incremental diameter of traditional S-ROM could meet clinical needs; (ii) propose some suggestions for prosthesis improvement to fit high-riding DDH patients.
2 Materials and Methods
2.1 Patients
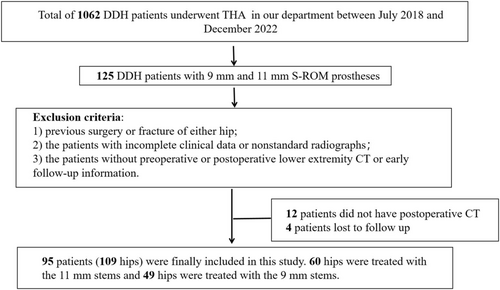
In this study, we retrospectively analyzed 1062 DDH patients who underwent primary THA with S-ROM prostheses in our department between July 2018 and December 2022. For the purpose of this study, we included 125 Hartofilakidis type C DDH patients with 9 mm or11 mm S-ROM prostheses. Of those, 16 patients (12.8%) were lost prior to the minimum study follow-up of half a year or had incomplete datasets. The inclusion criteria were as follows: (1) all surgeries were performed through the posterolateral approach, and (2) all surgeries were performed by the same surgeon with extensive experience (an average annual volume of 500 joint replacements for 10 years). The exclusion criteria were as follows: (1) previous surgery, infection, or trauma of either hip, (2) incomplete clinical data or nonstandard radiographs, and (3) without preoperative or postoperative lower extremity CT. The detailed process is shown in Figure 1. Our study was approved by the Ethics Review Meeting of our department. The study results are reported in line with the STROCSS criteria [7].
2.2 Surgery
All patients included in this study underwent detailed preoperative planning to select appropriate prostheses, utilizing both 2D planning software (Orthoview, version 3.0, Materialize NV, Belgium) and/or 3D planning software (AIHIP, Changmugu, China). Femoral stems with diameters of 9 or 11 mm were selected based on the femoral medullary canal diameter. When the planned prosthesis was a 10 mm femoral stem, we generally adopted the “rather larger than smaller” principle, prioritizing the 11 mm femoral stem to ensure prosthesis stability (particularly in osteotomy cases, where distal reaming and pre-binding with cerclage wires were performed to accommodate larger stems).
Trident acetabular prostheses (Stryker, USA) or Pinnacle acetabular prostheses (Johnson & Johnson, USA) were used in the acetabular side, and S-ROM modular prostheses (Johnson & Johnson, USA) were used in the femoral side.
The acetabular cup was placed at the anatomic position. We reamed the acetabulum to at least 44 mm to simultaneously accommodate the interface of ceramic on ceramic. In the femoral side, a sleeve or cone was chosen depending on the shape of the proximal femur. The trial component was subsequently inserted, and reduction was attempted. If unsuccessful, the distance between the center of the acetabular cup and the femoral head during trial reduction was recorded, followed by subtrochanteric transverse osteotomy, whose length was equal to the previously determined length minus 1.5 cm.
Regular antibiotic and antithrombotic prophylaxis were administered postoperatively. Patients were placed in the genuflex hip flexion dorsal position to reduce femoral nerve and sciatic nerve tension. Patients who did not undergo osteotomy were allowed partial weight-bearing 1 day after surgery, whereas a 3-week delay was required for patients who underwent subtrochanteric osteotomy.
2.3 Clinical and Radiographic Evaluation
The main purpose of this study was to evaluate the surgical and short-term adverse effects of the limited size of the distal stem, and the main evaluation indicators were available for a relatively short period postoperatively. Patient demographic data, including age, sex, height, weight, body mass index (BMI) and primary disease information, were collected from medical records.
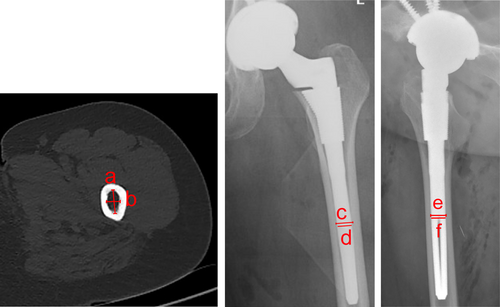
Standard anteroposterior and lateral radiographs of the bilateral hips and lower limb CT were taken for each patient preoperatively and postoperatively. The anterior–posterior and internal-external diameters of the medullary cavity corresponding to the bifurcation of the coronal slot were measured separately on the preoperative CT, that is, the coronal and sagittal medullary lengths at the mid-isthmus level of the femur (Figure 2). Information on intraoperative fracture at the distal end of the prosthesis was collected from the surgical records and postoperative radiological data. The canal filling ratio was defined as the width of the prosthesis divided by the width of the medullary cavity as measured at the bifurcation of the coronal slot on postoperative X-ray (Figure 2) [8]. We also used these views to observe whether the distal coronal slot was closed. The osteotomy healing rate was measured 6 months postoperatively via X-ray; nonunion of the osteotomy was manifested by discontinuous cortical callus at the osteotomy site on the anteroposterior and lateral radiographs of the bilateral hips. To ensure measurement accuracy and reduce measurement error, two nonparticipating orthopedic surgeons with rich measurement experience obtained the measurements, and the final result was taken as the mean of the two similar measurements.
2.4 Statistical Analysis
SPSS version 26 (IBM, Armonk, NY, USA) was used for data analysis. The inter-observer reliability was used to analyze the reliability of the measured data. Continuous data are presented as the means and standard deviations. Independent samples t-tests were used to compare the diameters of the medullary cavity and the canal filling rates of the prostheses between the different groups. The chi-square test was used for the comparison of intraoperative fracture rate and osteotomy rate between different groups. Logistic regression analysis was employed to identify the independent risk factors for intraoperative periprosthetic femoral fracture. A p value < 0.05 was considered to indicate statistical significance.
3 Results
The ICC analysis demonstrated that the inter-observer reliability value was 0.877 [0.823, 0.915], indicating excellent agreement. A total of 95 patients (109 hips), consisting of 12 men (14 hips) and 83 women (95 hips), were included in our study. There was no difference in demographic information between the two groups. The patients' detailed demographics are shown in Table 1.
| Variable | 9 mm | 11 mm | Statistic value | p |
|---|---|---|---|---|
| Gender | X2 = 0.165 | p = 0.684 | ||
| Female | 53 (48.6%) | 42 (38.6%) | ||
| Male | 7 (6.4%) | 7 (6.4%) | ||
| Age (years) | 38.63 ± 11.55 | 43.51 ± 11.88 | t = −1.657 | p = 0.101 |
| Height (m) | 1.56 ± 0.06 | 1.59 ± 0.07 | t = −1.559 | p = 0.123 |
| Weight (kg) | 56.64 ± 8.7 | 60.63 ± 11.63 | t = −1.935 | p = 0.056 |
| BMI (kg/m2) | 23.03 ± 3.06 | 23.98 ± 3.62 | t = −1.453 | p = 0.150 |
- Abbreviations: BMI, body mass index; SD, standard deviation.
3.1 Clinical and Radiographic Outcomes
A total of 60 hips were treated with S-ROM femoral prostheses with a distal diameter of 9 mm, and the remaining 49 hips were treated with 11 mm.
Ten hips were found to have intraoperative periprosthetic femoral fractures of the distal femoral stem; the fracture rate in the group of 11 mm (8 of 49, 16.3%) was 4.94 times that in the group of 9 mm (2 of 60, 3.3%) (p = 0.045). Fractures around the distal end of the femoral prosthesis occurred at the time of femoral prosthesis implantation and were predominantly manifested as longitudinal fractures.
Preoperative CT measurements revealed that the mean mediolateral diameters of the medullary cavity in the group of 9 mm and the group of 11 mm were 0.84 cm and 1.03 cm, respectively, and the mean anterior–posterior diameters were 1.40 cm and 1.49 cm, respectively. The cortical index at the medullary isthmus was 52% and 54% in the group of 9 and 11 mm.
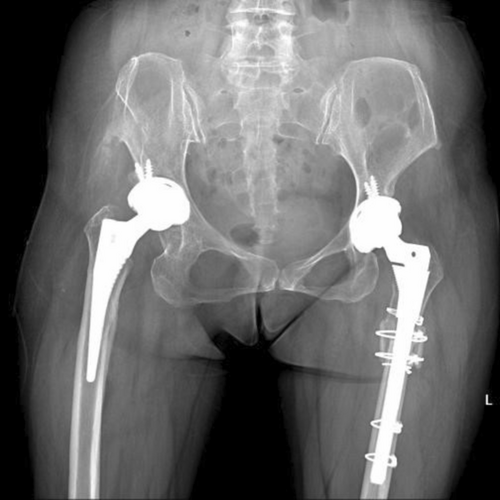
The canal filling ratio of the femoral prosthesis in the anterior–posterior direction was significantly lower than that in the medial-lateral direction in both groups. The canal filling ratio in the group of 9 mm is significantly lower than that of the 11 mm group, which might explain the reason for nonunion in the patients who had subtrochanteric osteotomy and 9 mm S-ROM (Figure 3). The bilateral leg length discrepancy in this patient is within 1 cm. On the left side, the degree of femoral head dislocation was lower compared to the right side, and the development of the acetabulum and proximal femur was superior on the left. Consequently, no osteotomy was performed during the left THA. In contrast, the right hip exhibited a higher degree of dislocation and a lower center of rotation, necessitating osteotomy to adjust the overall limb length.

Delayed union or nonunion usually leads to a poor prognosis [9]. The osteotomy rate was 80% with the 9 mm stem and 59% with the 11 mm stem, and in these patients with a 9 mm stem, five of the osteotomies did not heal; two of the patients with 11 mm stems did not heal. For these patients, we typically recommend bed rest and weight-bearing restrictions. If nonunion persists 1 year postoperatively, revision of the femoral component or allograft bone plate augmentation should be performed. The detailed radiographic outcomes of the patients in the 9 group and 11 mm group were shown in Table 2. Logistic regression analysis revealed that prosthesis diameter enlargement was not an independent risk factor for intraoperative periprosthetic femoral fractures (Table 3).
| Variable | 9 mm | 11 mm | Statistic value | p | ||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Range | Median | Mean ± SD | Range | Median | |||
| Intraoperative fracture rate (%) | 3.3 (2 of 60) | 16.3 (8 of 49) | X2 = 4.017 | p = 0.045 | ||||
| Cortical index (%) | 53.95 ± 4.57 | 41.99–63.02 | 54.31 | 52.67 ± 4.70 | 40.38–60.85 | 53.36 | t = 1.393 | p = 0.167 |
|
Medullary cavity diameter (cm) |
||||||||
| Anterior–posterior direction | 1.4 ± 0.28 | 0.85–2.01 | 1.39 | 1.49 ± 0.25 | 0.93–2.11 | 1.51 | t = −1.608 | p = 0.111 |
| Medial-lateral direction | 0.84 ± 0.2 | 0.57–1.35 | 0.84 | 1.03 ± 0.18 | 0.58–1.42 | 1.03 | t = −4.693 | p < 0.05 |
|
Canal filling ratio (%) |
||||||||
| Anterior–posterior direction | 71.24 ± 10.23 | 47.24–94.12 | 73.2 | 78.54 ± 7.28 | 63.43–91.06 | 78.2 | t = −4.068 | p < 0.05 |
| Medial-lateral direction | 82.71 ± 7.24 | 61.88–95.19 | 84.91 | 86.74 ± 6.09 | 69.81–95.24 | 86.85 | t = −2.986 | p < 0.05 |
| Osteotomy rate (%) | 71.7 (43 of 60) | 67.3 (33 of 49) | X2 = 0.238 | p = 0.625 | ||||
| Number of osteotomy nonunion | 5 | 2 | X2 = 0.692 | p = 0.405 | ||||
| Variable | β | p | OR (95% CI) |
|---|---|---|---|
| Age | −0.005 | 0.886 | 0.995 (0.935, 1.060) |
| BMI | −0.065 | 0.595 | 0.937 (0.737, 1.192) |
| Prosthesis diameter | 0.872 | 0.052 | 2.392 (0.993, 5.767) |
In the group of 11 mm, the mediolateral canal filling ratio of the fractured hips was significantly larger than that of the unfractured hips, which might explain the higher fracture rate of 11 mm S-ROM (Table 4). Typical X-rays of intraoperative fractures were shown in Figure 4.
| Variable | Fractured hip | Non fractured hip | Statistic value | p | ||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Range | Median | Mean ± SD | Range | Median | |||
| Medullary cavity diameter (cm) | ||||||||
| Anterior–posterior direction | 1.59 ± 0.21 | 1.14–1.81 | 1.66 | 1.48 ± 0.26 | 0.93–2.11 | 1.51 | t = −0.083 | p = 0.934 |
| Medial-lateral direction | 1.14 ± 0.18 | 0.97–1.49 | 1.16 | 1.03 ± 0.19 | 0.76–1.42 | 1.03 | t = −0.985 | p = 0.329 |
| Canal filling ratio (%) | ||||||||
| Anterior–posterior direction | 79.54 ± 7.61 | 70.66 ~ 86.76 | 81.12 | 78.46 ± 7.15 | 63.43 ~ 91.06 | 78.20 | t = 0.338 | p = 0.737 |
| Medial-lateral direction | 91.59 ± 3.51 | 84.33 ~ 93.91 | 90.96 | 86.23 ± 6.1 | 69.81 ~ 95.24 | 86.85 | t = 2.064 | p = 0.044 |
In the group of 9 mm, there was no significant difference in the medullary cavity diameter or canal filling ratio between the fracture and nonfracture groups (Table 5).
| Variable | Fractured hip | Non fractured hip | Statistic value | p | ||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Range | Median | Mean ± SD | Range | Median | |||
| Medullary cavity diameter (cm) | ||||||||
| Anterior–posterior direction | 1.42 ± 0.23 | 1.19–1.65 | 1.42 | 1.4 ± 0.28 | 0.85–2.01 | 1.39 | t = −0.342 | p = 0.734 |
| Medial-lateral direction | 0.80 ± 0.20 | 0.6–0.99 | 0.80 | 0.85 ± 0.20 | 0.57–1.35 | 0.84 | t = −0.088 | P = 0.93 |
| Canal filling ratio (%) | ||||||||
| Anterior–posterior direction | 69.59 ± 9.22 | 60.34–78.81 | 69.59 | 71.31 ± 10.26 | 47.34–94.12 | 73.20 | t = −0.228 | p = 0.821 |
| Medial-lateral direction | 76.52 ± 1.33 | 75.18–77.85 | 76.52 | 82.96 ± 7.27 | 61.88–95.20 | 84.91 | t = −1.229 | p = 0.225 |
4 Discussion
In this study, the 11 mm group showed a significantly higher canal filling ratio in both anterior–posterior and medial-lateral directions compared to the 9 mm group, and the rate of intraoperative periprosthetic femoral fractures of the 11 mm S-ROM was nearly 5 times higher than that of the 9 mm S-ROM. Subgroup analysis indicated that within the 11 mm group, the fracture subgroup had a significantly higher canal filling ratio in the medial-lateral direction than the non-fracture subgroup. The absence of the 10 mm stem of S-ROM resulted in the mismatch between the prosthesis and the medullary cavity, which could explain the above clinical problems. Thus, the well-used S-ROM design with skipping size of the distal stem diameter could increase the risk of intraoperative periprosthetic femoral fractures in high-riding DDH patients. It is necessary for a 1-mm increment of distal stem diameter in such patients.
4.1 Limitations of Current Asian-Specific Designs
Currently, the main prostheses used for high-riding DDH are the S-ROM prosthesis and the Wagnar cone femoral stem. However, the Wagnar cone femoral stem, owing to its thin distal end, tends to be unstable after subtrochanteric osteotomy. Therefore, the S-ROM stem is the most widely used prosthesis in our department for high-riding DDH patients. Several existing studies have also demonstrated the superior long-term survival and few complications associated with S-ROM prostheses in THA for DDH [4, 10, 11].
However, intraoperative periprosthetic femoral fractures of S-ROM are still a serious problem in the Chinese population. Cao et al. performed THA on 58 (71 hips) patients with Hartofilakidis Type C DDH, and a total of 20 hips were found to be intraoperatively fractured [12]. Zhou et al. reported a higher intraoperative fracture rate of 6.8% (7 of 103) in THA in Chinese DDH patients [13]. Furthermore, the high osteotomy rate observed in high-riding Chinese DDH patients significantly increases fracture risk at the osteotomy site [14, 15]. In contrast, the incidence of intraoperative fractures is much lower in western patients. Cameron et al. reported 10 intraoperative fractures in 517 patients with S-ROM prostheses, with an incidence of 1.9% [16]. To put it simply, the reason is that the relatively weak bone quality and narrow femoral cavity of the Asian population have insufficient tolerance to the traditional S-ROM design. Particularly, the S-ROM's slot opens in the coronal position, which is not compatible with the long anterior–posterior and short medial–lateral diameters of the femoral medullary cavity in DDH patients, easily leading to femoral fracture during THA.
The S-ROM-A was designed for the Asian population, which is characterized by a smaller stature, less bone stock, and a narrow canal. Several studies have reported that treatment with S-ROM-A leads to a better implant survival rate in Asian DDH patients, especially patients with difficult anatomy [17-19]. It has a femoral stem with a distal diameter of 10 mm, which partially solves the problem of skipping size. However, S-ROM-A prosthesis systems are not currently available in China, and they are plagued with several problems. Many studies also reported excellent long-term prosthetic survival with the S-ROM-A, but its thin trunnion increased the risk of trunnionosis [20-22]. The incidence of osteolysis was slightly greater in the S-ROM-A than in the S-ROM [23]. Kobayashi et al. reported a higher rate of aseptic loosening due to a lower canal filling ratio (16 of 104 hips, 15.4%) [24]. Compared with the traditional S-ROM, the S-ROM-A prosthesis has a shorter stem, a smaller diameter stem neck, and a bullet-shaped stem end [17]. Although shorter stems better fit the smaller femoral structure of Asian patients, this increases the risk of prosthetic instability in the site of subtrochanteric shortening osteotomy, which can lead to serious complications [25]. Moreover, the distal opening of the stem remains in the coronal position and does not match the morphology of the medullary cavity in Hartofilakidis C DDH patients.
4.2 Design Optimization Recommendations
We have made suggestions for prosthesis optimization based on our department's clinical practice. Firstly, it is necessary for a 1-mm increment of distal stem diameter in Chinese DDH patients. Secondly, the distal slot of the modular prosthesis should be set in the sagittal position so that there is sufficient cushion space in the mediolateral direction, where the diameter of the femoral medullary cavity is relatively small, potentially reducing the incidence of intraoperative femoral fracture.
4.3 Strengths and Limitations
This study provided evidence-based support for the 1-mm incremental design of domestic prosthetic systems. Furthermore, it proposes a novel domestically developed prosthetic system design tailored to the anatomical characteristics of these patients. Meanwhile, this study has several limitations. Firstly, the sample size of our study was relatively small (109 Hartofilakidis C dysplasia hips), although sample sizes of more than 100 are rare for such complex cases. Important differences in survival rates may exist for a larger number of patients, however. Secondly, this was a retrospective study, and despite our careful follow-up, problems such as missed visits or case selection bias are inevitable. Thirdly, this study focused solely on intraoperative periprosthetic femoral fractures and post-osteotomy healing outcomes, and did not address other complications such as periprosthetic infection, nerve injury, or aseptic loosening. Fourthly, the inclusion of only 9 and 11 mm S-ROM for comparison may not be representative of all patients, but this typical comparison is very telling.
5 Conclusion
In conclusion, the existing S-ROM prosthesis cannot perfectly meet the needs of Chinese high-riding DDH patients. It is necessary for a 1-mm increment of distal stem diameter in such patients.
Author Contributions
Jiafeng Yi: methodology, validation, software, writing – original draft, conceptualization, data curation, visualization, investigation. Hongbin Xie: methodology, investigation, software, data curation, formal analysis, writing – original draft. Yubo Liu: methodology, visualization, project administration, formal analysis. Yijian Huang: conceptualization, methodology, visualization. Wei Chai: project administration, resources, writing – review and editing, funding acquisition, supervision, data curation. Xiangpeng Kong: funding acquisition, writing – review and editing, project administration, resources, supervision, data curation, validation.
Acknowledgments
We thank all authors who contributed to this work. All authors have made substantial contributions to (1) the study conception and design (2) drafting and revising critically for important intellectual content, and (3) final approval of the submitted version. Xiangpeng Kong and Wei Chai was primarily responsible for the supervision of the research, including research protocol designing, data acquisition, and manuscript preparation. Jiafeng Yi and Hongbin Xie were mainly responsible for research design, data extraction, statistical analysis, article analysis, and manuscript drafting. Jiafeng Yi and Hongbin Xie contributed to this work equally and both of them were co-first authors. Yubo Liu, Yijian Huang participated in this study design, manuscript drafting, data analysis, and constructive discussions.
Ethics Statement
Ethical approval for this study was obtained from our institutional ethical committee (S2018-014-01). This study have been performed in accordance with the ethical standards in the 1964 Declaration of Helsinki. All details that might disclose the identity of the subjects under study had been omitted.
Conflicts of Interest
The authors declare no conflicts of interest.




