Kirschner Wire Internal Fixation of the Medial Tibiotalar Joint for Indirect Repair of Deltoid Ligament Injury: A Retrospective Comparative Study
Abstract
Objective
Ankle joint fractures are often accompanied by medial deltoid ligament rupture. There is controversy over whether or how to treat deltoid ligament rupture. This study was aimed to explore the feasibility of repairing the medial deltoid ligament using Kirschner wire internal fixation of the medial tibiotalar joint combined with external fixation.
Methods
Forty-six patients with ankle fractures involving deltoid ligament rupture, treated between October 2012 and February 2021, were retrospectively evaluated. Twenty-five patients were treated with a Kirschner wire to fix the tibiotalar joint and indirectly repair the deltoid ligament as the repaired group. Twenty-one patients underwent reduction and fixation of internal and external malleolus fractures, and the deltoid ligament was not repaired in the unrepaired group. The American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score, visual analog scale (VAS), Medical Outcomes Short Form 36-item questionnaire score (SF-36), and Medial clear space perpendicular (preoperative, postoperative, final follow-up) were used for functional evaluations and reduction assessments. Mann–Whitney test were used to compare the differences between the groups.
Results
The follow-up time was 13–112 months with a mean of 59.32 months for the repaired group and 11–94 months with a mean of 53.43 months for the unrepaired group. There was no significant difference in the operative time or intraoperative blood loss between the two groups (p > 0.05). At the last follow-up, the AOFAS ankle-hindfoot and SF-36 scores of the repaired group were significantly higher than those of the non-repaired group (p < 0.05). Moreover, the VAS pain score was significantly lower and the Medial clear space perpendicular was significantly narrower in the repaired group than that in the unrepaired group.
Conclusion
Tibiotalar joint fixation using Kirschner wires is a simple and effective technique that can indirectly reduce and repair the deltoid ligament and stabilize the ankle.
Introduction
Ankle joint fracture refers to a partial or total fracture of the medial, lateral, and posterior malleoli, which is itself a form of intraarticular fracture. The deltoid ligament, which is the primary stabilizer of the medial side of the ankle joint, consists of superficial and deep fibers.1, 2 The deep layer of the deltoid ligament includes the deep anterior and posterior tibiotalar ligaments, which prevent external rotation of the talus.3, 4 In pronation ankle injuries, including pronation abduction and pronation external rotation, the medial malleolar or triangular ligament is the first structure damaged. In degree IV supination injuries, the structure damaged is the medial malleolar or triangular ligament. Therefore, ankle fractures are often associated with deltoid ligament injuries.5 In a prior study, Hintermann et al. evaluated 288 patients with acute ankle fractures using ankle arthroscopy and found that 40% had deltoid ligament injuries.6 The injured deltoid ligament might result in an unstable ankle joint, lead to peak loading of the cartilage at certain spots and finally lead to early osteoarthritis.5, 7, 8
Currently, whether deltoid ligament injuries require surgical repair of ankle fractures remains controversial.9 Scholars who support non-repair of the deltoid ligament believe that most deltoid ligament injuries can heal with only conservative treatment.10 They believed that the deep anatomical position of the deltoid ligament was too deep to be exposed during surgery.2 As such, it is necessary to expose the deltoid ligament only when intraarticular entrapment prevents talar reduction.11, 12 In a retrospective analysis, Maynou et al. found no significant difference in ankle function between nonsurgical and surgical groups.13 They believed that the deltoid ligament did not require repair if the ankle point could be reduced anatomically after fibular fixation. Scholars who support the repair of the deltoid ligament have noted that if this repair is not considered when treating ankle fractures, some patients are prone to poor reduction and ligament relaxation, resulting in chronic ankle instability, which is also an important cause of chronic ankle pain.8, 14-17 Tornetta et al. further found that 26% of patients with medial malleolus avulsion fractures had deep deltoid ligament injury,18 and showed that deltoid ligament dysfunction would occur if only the fracture fragment was reduced and fixed without repair of the deltoid ligament. Repair methods for deltoid ligament rupture mainly include direct silk suture, anchor suture for reconstruction, anchor suture for the medial malleolus transosseous tunnel, and tendon reconstruction. However, few studies have compared the effects of the indirect repair of medial malleolar deltoid ligament injuries of the ankle joints.
In the present study, we retrospectively analyzed the data of 46 patients with ankle complete fractures of the deltoid ligament treated between October 2012 and February 2021. All patients underwent stress tests following fixation of the medial and lateral malleolar fractures, which indicated medial instability.19 Thus, this study has three objectives: (i) to determine whether it is necessary to repair the medial malleolus deltoid ligament when patients with joint instability suggested by stress test and deep rupture of triangular ligament by MRI, (ii) to evaluate the feasibility of repairing the medial deltoid ligament using Kirschner wire internal fixation of the medial tibiotalar joint combined with external fixation; and (iii) to compare the difference between indirect repair by fixing with Kirschner wire internal fixation and uprepair of medial ankle triangular ligaments in ankle fracture patients with triangular ligaments ruptured. We anticipated our study could provide evidence for future practice.
Methods
Patient Eligibility
We retrospectively analyzed patients with ankle fractures and complete rupture of the deltoid ligament treated at our hospital between October 2012 and February 2021. The inclusion criteria were as follows1: adult patients aged 22–65 years2; simple ankle fracture3; MRI showing deltoid ligament deep rupture4; all patients underwent reduction and fixation of ankle fractures with or without K-wire internal fixation5; ankle joint matching is normal without external force after intraoperative reduction and fixation of ankle fractures (medial clear space ≤4 mm or astragalus lateral inclination <6°)6; external rotation stress test or Cotton test revealed that the medial ankle joint was unstable (medial clear space ≥5mm or astragalus lateral inclination ≥6°) after intraoperative reduction and fixation of ankle fractures. The exclusion criteria were1: deltoid ligament injury combined with vascular and nerve injury, or several combined injuries of head, chest, and abdomen, or fractures of other parts of the lower limbs2; history of diabetes or a prior history of lower limb vascular disease before admission. This study was approved by the ethics committee of Affiliated Hospital of Jining Medical University (IRB No. 2022C229) and all patients provided signed informed consent.
Surgical Procedures
All patients were administered spinal anesthesia and underwent anatomical reduction and fixation of the fibula. If the fracture of the posterior malleolus was ≥25%, fixation with screws or support plates was performed; in cases with a fracture of the medial malleolus, routine open anatomic reduction and internal fixation were used. In addition, if significant inferior tibiofibular separation was noted, one to two 3.5 mm cortical bone screws were used for fixation within 2–4 cm above the ankle joint space.
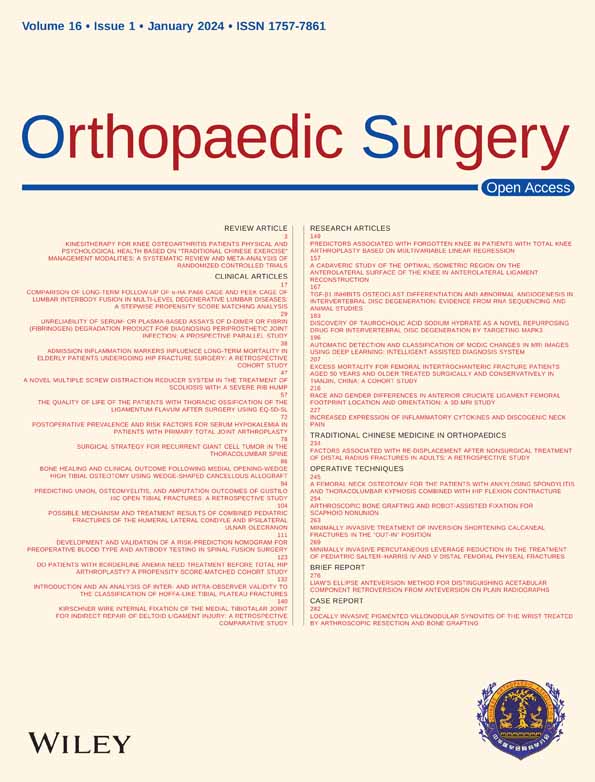
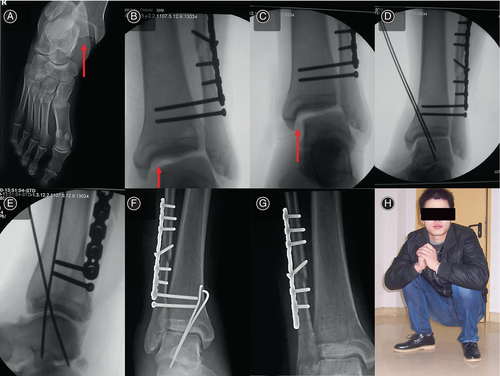
Kirschner wire repair of the medial malleolar deltoid ligament group (the repaired group): After fixation was completed, there was no obvious medial malleolus gap widening or astragalus lateral inclination, and ankle external rotation stress and Cotton tests were performed routinely. The external rotation stress test or Cotton test indicated a clear medial clear space widening (≥ 5mm) or astragalus lateral inclination (≥6°), indicating that the medial ankle joint was unstable, the medial tibiotalar joint was fixed with Kirschner wire (Figure 1). Anterior and lateral fluoroscopies of the ankle joint were performed after the reduction.
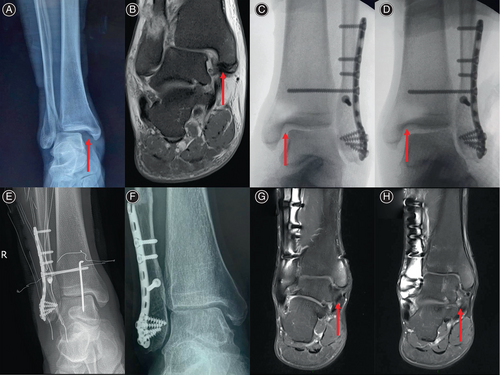
For patients in the unrepaired group, the medial malleolus clearance was normal under non-stress conditions following good reduction of ankle fractures and lower tibiofibular injuries. The external rotation stress test or Cotton test suggested medial ankle joint instability (medial clear space ≥5 mm or astragalus lateral inclination ≥6°), and still no repair was done to the medial malleolar deltoid ligament (Figure 2).
Postoperative Care and Outcome Assessment
The ankle joints were immobilized with short-leg braces for 6 weeks postoperatively in both groups. Weight bearing and ankle movement were contraindicated to avoid breaking the internal fixation Kirschner wire or affecting deltoid ligament healing. During these 6 weeks, rehabilitation exercises for the toes and knee joints of the affected limbs were performed, and oral anticoagulant drugs were administered to prevent deep vein thrombosis of the lower limbs. At 6 weeks, both groups underwent outpatient reexamination. In the repaired group, the Kirschner wire was removed under local anesthesia, and external fixation was removed to start nonweight-bearing ankle flexion and extension functional exercises. In the unrepaired group, the external fixation was removed to all initiation of nonweight-bearing ankle flexion and extension functional exercises. Patients in both groups visited the outpatient clinic again 12 weeks after the operation. Fracture union was confirmed by radiography and screws were removed under local anesthesia if the patient had fixation screws in the inferior tibiofibular region. Afterwards, both groups began full weight-bearing and increased ankle dorsiflexion and plantarflexion exercises. Subsequently, patients in the two groups visited the outpatient clinic for reexamination every 2–3 months. All patients were evaluated using the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score, visual analog scale (VAS) score, and a short-form 36-item questionnaire (SF-36). The medial clear space perpendicular (preoperative, postoperative, final follow-up) was used to assess the reduction outcomes in both patient groups.
Statistical Analysis
Statistical analyses were performed using SPSS (version 23.0; SPSS Inc., Chicago, Illinois, USA). The chi-square test or Fisher's exact test was used to compare categorical data. The normality of the distribution was examined using the Shapiro–Wilk test. Normally distributed continuous data were compared between groups using parametric tests (t-test or ANOVA). In the case of a skewed distribution in the numerical data, the Mann–Whitney U test was used. Statistical significance was set at p < 0.05.
Results
Baseline Characteristics
A total of 46 patients with ankle fractures who met the inclusion criteria were enrolled, including 25 in the repaired group and 21 in the unrepaired group. The mean age of the patients was 40.91 years, while the mean follow-up time was 59.32 months (range 13–112) for the repaired group and 53.43 months (range 11–94) for the unrepaired group. According to the Lauge-Hansen classification, in the repaired group, there were 14 cases of degree IV supination-external rotation fractures, six cases of degree IV pronation external rotation fractures, and five cases of III-degree pronation-abduction fractures. In the unrepaired group, there were nine cases of IV-degree supination-external rotation fractures, 11 cases of IV-degree pronation-external rotation fractures, and one case of III-degree pronation-abduction fracture. There were no significant differences in age, sex, L-H type, fracture cause, or follow-up time between the two groups (p > 0.05). The baseline patient characteristics are shown in Table 1.
| Variables | Repaired group | Unrepaired group | t/X2 | p |
|---|---|---|---|---|
| Age, year, mean ± SD | 41.36 ± 12.14 | 40.38 ± 11.90 | 0.275 | 0.785 |
| Gender, n (%) | ||||
| Male | 16 (64.00) | 14 (66.7) | 0.036 | 0.85 |
| Female | 9 (36.00) | 7 (33.3) | ||
| L-H classification, n (%) | ||||
| Supination-external rotation | 14 (56.00) | 9 (42.86) | 4.66 | 0.101 |
| Pronation external rotation | 6 (24.00) | 11 (52.38) | ||
| Pronation-abduction | 5 (20.00) | 1 (4.76) | ||
| Reasons of injury, n (%) | ||||
| Twist trauma | 3 (12.00) | 1 (4.76) | 7.638 | 0.086 |
| Sprain | 3 (12.00) | 8 (38.10) | ||
| Fall damage | 10 (40.00) | 10 (47.62) | ||
| Crushing | 2 (8.00) | 1 (4.76) | ||
| Bruises | 7 (28.00) | 1 (4.76) | ||
| Follow-up time, months, mean ± SD | 59.32 ± 24.33 | 53.43 ± 21.04 | 0.869 | 0.389 |
- Abbreviation: SD, standard deviation.
Clinical Outcomes
All patients achieved grade A wound healing 2 weeks after the operation. The patient's internal fixation Kirschner wires and inferior tibiofibular screws did not break, and there were no other definite complications. There was no significant difference in operation time between the repaired and unrepaired groups (p > 0.05). There was no significant difference in intraoperative blood loss between the two groups (p > 0.05). In addition, the AOFAS ankle-hindfoot and SF-36 scores of the repaired group were significantly higher than those of the unrepaired group (95 vs. 86, p = 0.017), the VAS pain score of the repaired group was significantly lower than that of the unrepaired group (1 vs. 2, p = 0.049). Moreover, the Medial clear space perpendicular (postoperative, final follow-up) of the repaired group was significantly narrower than that of the unrepaired group (2.90 vs. 3.40, p = 0.022; 2.90 vs. 3.20, p 0.005). The clinical outcomes of patients are shown in Tables 2 and 3.
| Variables | Repaired group | Unrepaired group | t/Z | p |
|---|---|---|---|---|
| AOFAS score | 95 (90.0, 97.5) | 86 (77.5, 96.5) | −2.379 | 0.017 |
| VAS score | 1 (0.0, 2.0) | 2 (0.0, 4.0) | −1.972 | 0.049 |
| SF-36 score | 95 (90.0, 97.0) | 83 (74.0, 96.0) | −2.646 | 0.008 |
| Operation time(min) | 108 (100.0, 115.0) | 100 (80.0, 127.5) | −0.673 | 0.501 |
| Intraoperative blood loss (ml) | 100 (50.0, 100.0) | 100 (50.0, 100.0) | −0.795 | 0.427 |
- Note: Data were expressed as median (25%th, 75%th).
- Abbreviations: AOFAS, American Orthopaedic Foot and Ankle Society; SF-36, Short Form 36; VAS, visual analog scale.
| Medial clear space perpendicular | Repaired group | Unrepaired group | t/Z | p |
|---|---|---|---|---|
| Preoperative | 5.20 (4.25, 8.80) | 6.70 (5.45, 10.65) | −1.853 | 0.064 |
| Postoperative | 2.90 (2.60, 3.40) | 3.40 (2.90, 3.90) | −2.324 | 0.022 |
| Final follow-up | 2.90 (2.70, 3.10) | 3.20 (2.95, 3.80) | −2.827 | 0.005 |
- Note: Data were expressed as median (25%th, 75%th).
Discussion
Main Findings of this Study
This study indicated that: (1) Repairing the deep rupture of the medial deltoid ligament in ankle fractures with joint instability during stress tests can achieve better ankle joint function and medial clear space; (2) fixation of the medial tibiotalar joint with Kirschner wire can achieve high-quality indirect repair of the medial deltoid ligament, which is a simple, quick, and effective technique.
Important Role of the Deltoid Ligament of the Medial Malleolus
The deltoid ligament is one of the most important anatomical structures for the maintenance of ankle stability. The deep layer of the deltoid ligament includes the deep anterior and posterior tibiotalar ligaments, which prevent external rotation of the talus.20, 21 Currently, the optimal repair strategy for the deltoid ligament is controversial.9 Many researchers have found through in vitro mechanical tests that cutting the deep deltoid ligament significantly changes the stability of the ankle joint in all directions.22-24 If the deep deltoid ligament is kept intact and the superficial ligament, lateral collateral ligament, or compound lateral malleolus fractures are completely cut off, the talus does not shift or tilt significantly under stress. Burns et al. previously found that the inferior tibiofibular syndesmosis widened only slightly after cutting the inferior tibiofibular syndesmosis ligament, but the inferior tibiofibular syndesmosis appeared to widen significantly when the deep deltoid ligament was further cut.25 This suggests that repair of the deep deltoid ligament is crucial when the deltoid ligament is damaged.
Patients with Unstable Ankle Joints Suggested by Stress Test Need to Repair their Broken Medial Malleolus Deltoid Ligament
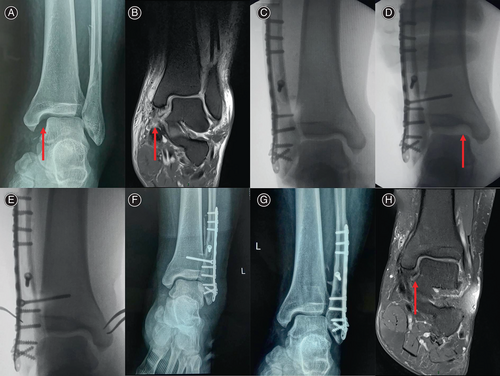
During surgery, we found that in patients with injuries to all three ankle structures, if only two lateral structures were repaired without repairing a deep rupture of the medial deltoid ligament, the ankle in some patients did not stabilize, as reported by Bloemer et al.,26 but still showed extreme instability. In the present study, although the ankle joint of the patient matched normally without stress, it was abnormally matched under the condition of external rotation or internal and external traction of stress, indicating that the ankle joint was unstable. In addition, some patients with deltoid ligament injuries have normal ankle joint spaces after surgery; however, the medial malleolus space gradually widens, and the medial malleolus experiences pain after long-term walking or walking on uneven surfaces. Pain in the medial malleolar region when passive external rotation was applied indicated poor healing of the medial malleolar deltoid ligament. MRI demonstrated poor deep healing of the deltoid ligament (Figure 3). In the present study, 46 patients with deltoid ligament injury and internal and external malleolus fractures who still had medial instability following reduction and fixation were treated with medial malleolar Kirschner wire fixation with indirect repair of the deltoid ligament and without repair of the deltoid ligament. Long-term follow-up showed that the recovery in patients in the deltoid ligament repaired group was significantly better than that in patients in the unrepaired group. The insertion process of Kirschner wires is simple, and there is no need to explore the medial clear space, with research indicating that the operation time and blood loss were not significantly different from those of the unrepaired group. Therefore, we recommend selective repair of the ruptured medial deltoid ligament.
Reasons for Using Kirschner Wire Fixation of the Medial Tibiotalar Joint to Repair the Deltoid Ligament
Inspired by Anchor Staple Techniques
Repair methods for deltoid ligament rupture mainly include direct silk suture, anchor suture for reconstruction, anchor suture for the medial malleolus transosseous tunnel, and tendon reconstruction.27, 28 Currently, the suture anchor technology is the most widely used technique, and its effect is better. However, owing to the narrow medial clear space and deep position of the deltoid ligament, application of the suture anchor technique significantly increases the operation time.29 Suture Anchors Technology restores the continuity of the deltoid ligament. To some extent, suture anchor technology reconstructs the deltoid ligament, eliminates abnormal stress of the talus valgus and external rotation, restores the normal anatomical position of the talus, and facilitates healing of the ligament without tension.30 In this study, based on the principles of suture anchor technology, a simpler and more convenient method involving medial Kirschner wire fixation of the tibial joint was adopted. After reduction and fixation of the inner and outer malleoli and the lower tibia and fibula of the ankle joint were completed during the operation, a stress test was performed. If the test showed that the medial structure was still unstable,19 there was no need to expose the deltoid ligament, and one to two Kirschner wires were inserted into the medial half of the talus 1–2 cm above the medial malleolus. Based on this, the normal anatomical position of the talus could be effectively maintained immediately, the normal gap of the medial malleolus and continuity of the deep and superficial layers of the deltoid ligament can be maintained, and immediate stability of the ankle joint and the normal resting length of the deltoid ligament can be obtained. This ensured a high-quality healing of the medial deltoid ligament.
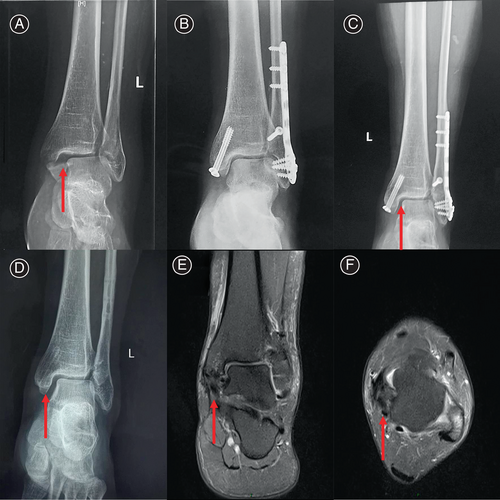
Supported by Anatomical Structure
Clinically, patients commonly show significant medial space expansion (≥5 mm) or lateral inclination of astragalus (≥6°) following good reduction and fixation of ankle fractures and lower tibiofibular injuries. In the present study, we found that good results could still be obtained by placing one to two Kirschner wires with diameter of 2–2.5 mm directly on the medial malleolus for 2–3 cm to fix the tibiotalar joint (Figure 4). Importantly, Kirschner wires provide good reduction in the externally rotated talus. During fixation, the ankle joint was maintained in a neutral position with 90° dorsalis extension, and the automatic reduction of the talus was obviously felt during Kirschner wire injection into the talus from the upper inner part of the medial malleolus. Because the ankle is a saddle joint, the talar dome is trapezoidal, wide anteriorly, and narrow posteriorly. During dorsal extension, the wedge-shaped trajectory of the talar dome formed a stable bone-to-bone joint connection with the distal tibial dome. At this time, a Kirschner wire was inserted, which was only needed to correct the abnormal external rotation of the talus, and could easily fix the talus directly below the articular surface of the distal tibia without deviation. It is as if the saddle joint of the distal tibia is used as a template and the Kirschner wire is driven in, pulling the talus in and automatically sliding it into the most stable position, which is the anatomic position of the talus. Current biomechanical and clinical data indicate that restoring and maintaining the talus directly below the articular surface of the distal tibia is the most important factor in determining the prognosis of ankle fractures. These patients were followed-up and achieved good ankle function. These cases further confirm the effectiveness of the Kirschner wire in the indirect repair of the trigonal ligament of the medial malleolus.
The Truth of Good Reduction and High-Quality Healing
Some scholars believe that after the deltoid ligament ruptures, the broken end may become stuck in the joint, affecting talar reduction.10, 31, 32 However, Bucholz et al. found that the deltoid ligament rarely hindered talar reduction. In our study, we did not explore the medial clear space in any of the patients, and instead directly performed Kirschner wire fixation at the medial malleolus-superior tibiotalar joint to obtain normal matched ankle joints. Therefore, we believe that the deltoid ligament seldom interferes with talar reduction without probing it. Based on the above reasons, we propose that this method is simple and effective and greatly reduces the operation time.
Although this study only conducted indirect repair of the deltoid ligament, the Kirschner wire could use the tibial fornix as a template to pull the talus closer to the tibia during the process of insertion, ultimately leading to good reduction of the talus in the ankle mortise, and good reduction and tight combination of the broken deltoid ligament. This repositioning is strictly maintained, and to some extent, there is a compression effect similar to the primary healing of the shaft fracture under the action of the compression plate, which easily promotes high-quality healing of the ligament and avoids healing of the ligament in the loose position, thus avoiding the potential instability of the ankle joint to the greatest extent possible (Figure 1G,H). Owing to the deep location of the internal ankle deltoid ligament, direct suturing is difficult and the quality of the suture is difficult to guarantee. Anchor staple suture is the mainstream direct or indirect repair method; however, in practice, the problem of subsequent laxity of the staple knot and healing of the ligamentous laxity after the anchor staple suture must also be considered.
Surgical Techniques to Avoid Complications
The Kirschner wire repair technique is most likely to result in complications, such as internal fixation Kirschner wire breakage, articular cartilage damage, ankle stiffness, etc. If a Kirschner wire breaks, catastrophic consequences may occur. Because fractures are most likely to occur in the joint, it is difficult to remove the broken Kirschner wire, which is very likely to cause articular cartilage wear, eventually resulting in severe osteoarthritis. To prevent such complications, strict external fixation with braces was performed for 6 weeks after surgery in the present study, and weight bearing and trauma were strictly prohibited. In addition, the K-wires were maintained at a certain thickness, and K-wires with a diameter of 2–2.5 mm were used in this study. Owing to proper measures, there were no cases of K-wire breakage in this study. Articular cartilage may be damaged by Kirschner wire insertion. To minimize cartilage damage, the Kirschner wire should be as thin as possible while avoiding breakage. Therefore, a Kirschner wire fixation with a diameter of 2–2.5 mm was used in this study. In this study, the average 59.32-month follow-up of 25 patients in the Kirschner wire fixation group showed that the AOFAS, VAS pain, and SF-36 scores were excellent, indicating that damage to the medial malleolar cartilage was negligible. The ankle joint plantar flexion position was fixed for a long time, and joint stiffness was easily achieved. If plantar flexion fixation can be avoided, stiffness can be avoided. In the present study, dorsiflexion of the ankle joint was maintained at 90° during Kirschner wire insertion to avoid ankle stenosis. After the removal of the Kirschner wire and external fixation, active functional exercises were encouraged. Finally, ankle range of motion was significantly recovered, and ankle stiffness was avoided.
In addition to the potential complications mentioned above, damage to structures such as the great saphenous vein, posterior tibial vessels, and tibial nerve may occur. If the Kirschner wire penetrates too deeply, stiffness of the tibiotalar joint may result. prolonged fixation with Kirschner wires and external fixation devices may lead to deep vein thrombosis in the lower limb. To avoid damage to these vascular and neural structures, the entry point for the wire should be strictly controlled to be near the midpoint of the tibial surface above the medial malleolus, and the soft tissues near the entry point should be dissected and protected with a guide. The depth of the Kirschner wire should be strictly limited to avoid affecting the subtalar joint and causing stiffness. To prevent lower limb deep vein thrombosis, in addition to active movement of the toes, knee joint, and hip joint, isometric exercises of the ipsilateral calf muscles should be performed, and appropriate anticoagulant medication should be taken.
Limitations and Strengths of this Study
This study had a limited number of cases, and further increasing the sample size is necessary. The feasibility of this method requires confirmation through multicenter, large-sample, prospective studies. However, through reasonable clinical assessment and the application of Kirschner wire fixation to achieve indirect reduction and fixation of the deltoid ligament, high-quality healing can be achieved, resulting in a clinically functional and stable ankle joint. This method is simple, quick, and effective. It also provides a new approach for trauma orthopaedic surgeons advocating for the repair of deep ruptures of the medial deltoid ligament.
Conclusion
Tibiotalar joint fixation using Kirschner wires is a simple and effective technique that can indirectly reduce and repair the deltoid ligament and stabilize the ankle. This method also provides a new idea for trauma orthopaedic surgeons who advocate for deep repair of ruptured medial malleolus triangles. However, the number of cases in this study was small, and the sample size needs to be further increased. Prospective randomized controlled trials with larger sample sizes are required to confirm the results of this study.
Acknowledgements
We would like to show our gratitude to everybody for their assistance in this study, and thanks to the reviewer for their valuable comments.
Conflict of Interest Statement
The authors declare that there is no conflict of interest in this study.
Ethics Statement
This study was approved by the ethics committee of Affiliated Hospital of Jining Medical University (IRB No. 2022C229), and all patients signed informed consent.
Author Contributions
Yifeng Zhao and Chunyang Meng conceived and designed the study; Yifeng Zhao, Haibin Wang, Bin Wu, and Dailiang Jia performed the surgical procedure and provided the case; Fenghua Zhu performed patient telephone follow-up; Tao Yang performed conducted data collection, statistical processing, and writing the manuscript; Chunyang Meng contributed to the surgical guidance and revised the article. All authors contributed to the article and approved the submitted version.
Open Research
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding authors.