Possible Mechanism and Treatment Results of Combined Pediatric Fractures of the Humeral Lateral Condyle and Ipsilateral Ulnar Olecranon
Shuai Liu, LianQi Peng these authors contributed equally to this work and should be considered co-first authors.
WeiFeng Lin, Xin Tang these authors contributed equally to this work and should be considered co-corresponding authors.
Abstract
Objective
Combined fractures of the lateral condyle of the humerus and the ipsilateral ulnar olecranon are rarely seen in children. Therefore, the mechanism and suitable treatments remain debatable. This study describes the possible mechanism of combined humeral lateral condyle and ipsilateral ulnar olecranon fractures and presents the treatment results.
Methods
Children diagnosed with combined fractures of the humeral lateral condyle and ipsilateralulnar olecranon from July 2010 to July 2020 were retrospectively analyzed. Humeral lateral condyle fractures were treated with open reduction and internal fixation with bioabsorbable pins. Ulnar olecranon fractures were treated with closed reduction and percutaneous pinning with K-wires for Mayo type IA fractures and with tension-band wiring or a locking plate for Mayo type IIA fractures. The postoperative function and appearance of the elbow were evaluated using the Flynn criteria and Mayo Elbow Performance Score (MEPS) at follow-up.
Results
The cohort comprised 19 patients aged from 4 to 11 years. Bony compression and avulsion by attached muscles and ligaments may be the leading factors causing the combined injuries, as the children fell with an outstretched and supinated elbow. The average follow-up time was 33 months. High MEPS of >90 indicated that good to excellent results were obtained without complications.
Conclusions
This study proposed a reasonable hypothesis for the mechanism of combined humeral lateral condyle and ipsilateral ulnar olecranon fractures in children. Satisfactory outcomes were achieved with bioabsorbable pins for lateral condyle fractures and closed reduction and percutaneous pinning with K-wires, tension-band wiring, or locking plate for olecranon fractures.
Introduction
Lateral condyle fractures of the humerus are common pediatric elbow fractures, accounting for 15% to 20% of all elbow fractures.1 The most common mechanism of humeral lateral condyle fractures is falling onto an outstretched hand with an extended elbow. Valgus impact or direct trauma to the elbow may also contribute to this type of injury.2 Olecranon fractures occur less frequently than humeral lateral condyle fractures, accounting for only 7% of pediatric elbow fractures.3 Olecranon fractures are often associated with concomitant elbow injuries, while isolated olecranon fractures are rare.4 Fractures of the olecranon may result from a direct blowtoa bent elbow or indirect avulsion by the tricepsmuscle.5 It is rare to encounter a lateral condyle fracture of the humerus with an associated ipsilateral olecranon fracture. Only a few studies have reported such injury patterns. Two mechanisms of injury have been identified: fall-on-outstretched hand (FOOSH) from a height and a fall with direct impact on a flexed elbow. However, the detailed mechanism of the combined injuries has not been clarified.6-12
The recommended treatment for a lateral humeral condyle fracture with an ipsilateral olecranon fracture is controversial. For displaced fractures, common treatments include closed reduction and percutaneous pinning (CRPP) with Kirschner wires (K-wires), CRPP with bioabsorbable pin fixation, and open reduction and internal fixation (ORIF) with tension-band wiring (TBW) and a locking plate.2, 13-17 However, each surgical method has its advantages and disadvantages, and no significant difference in clinical outcomes has been reported. For combined injuries with two or more fracture sites, suitable management needs to be considered more carefully and comprehensively. Lam et al.7 reviewed treatments for combined fractures of the lateral condyle of the humerus and the ipsilateral olecranon. When both fractures are nondisplaced, nonoperative methods are recommended. Surgical management should be considered if one or more fracture is displaced.
The present study aimed to (i) describe the possible mechanism of fractures of the lateral condyle of the humerus and the ipsilateral olecranon and (ii) report the clinical results of surgical management of such injuries.
Methods
A total of 19 pediatric patients (8 girls and 11 boys) with combined fractures of the lateral condyle of the humerus and ipsilateral ulnar olecranon treated in a single institute from July 2010 to July 2020 were reviewed. The inclusion criteria were (i) patient aged less than 14 years, (ii) no history of fractures in the same arm, (iii) follow-up of at least 24 months, and (iv) availability of medical records. Exclusion criteria were (i) open fracture, (ii) pathological fracture, and (iii) associated neurovascular injury. All surgeries were performed by an experienced pediatric orthopaedic surgeon and his team. Patients with lateral condyle fractures classified as Song type 4 or type 5 received surgical treatment.18 Bioabsorbable pins (D, L-lactide, CONMED Company, USA) with a diameter of 2 mm were used for fixation of the lateral condyle. For olecranon fractures, closed reduction and fixation with K-wires (2 mm) was performed for Mayo type I fractures,17 while TBW or a locking plate were used for Mayo type II fractures. All treatment methods were carried out in accordance with the relevant guidelines and regulations. Written informed consent was obtained from the legal guardians of all patients, and the study was approved by the institutional review board of our institute (IORG0003571).
Surgical Technique
All surgeries were carried out with the patient under general anesthesia in the supine position. A pneumatic tourniquet was applied with the arm in forward flexion at 90° and placed on a board. An incision of approximately 3–4 cm was made over the lateral condyle of the humerus to expose the fracture ends. After fracture exposure, the surrounding hematoma was cleared and fractures were anatomically reduced under direct vision. Two 2-mm crossed K-wires were applied, and the satisfactory reduction was confirmed by fluoroscopy. After satisfactory reduction was achieved, the K-wires were replaced by two 2-mm bioabsorbable pins (D, L-lactide, CONMED Company, USA). The wound was then closed in layers.
For Mayo type IA olecranon fractures, closed reduction was attempted under fluoroscopic guidance. Two crossed 2-mm K-wires were inserted percutaneously from the apex of the olecranon and placed parallel to the ulnar axis. After confirming adequate stability, the K-wires were cut short and bent in the soft tissues.
Open reduction and internal fixation was performed for Mayo type IIA olecranon fractures. A 6–7-cm midline incision was made at the elbow while ensuring the neurovascular structures were not injured. After removal of the surrounding hematoma, the periosteum was dissected to expose the fracture ends. For patients who received TBW, we followed the technique reported by Chalidis et al.18. For patients who received ORIF with a locking plate, the fracture fragments were reduced under direct vision. A plate with appropriate length was placed on the olecranon posteriorly and fixed with screws. After a thorough wash with normal saline, the wound was closed in layers.
Postoperative Care and Follow-up
Perioperative data, including operation duration and complications, were recorded. The operated elbow was routinely immobilized at 90° in a cast for 2–4 weeks to reduce the pain and swelling. If there was no significant local tenderness or longitudinal percussion pain, and radiographs of the elbow showed significant callus growth, the cast was removed. After removal of the cast, active range of motion of the elbow was encouraged under the supervision of a physiotherapist. Implants including K-wires, TBW, and plates were removed at 6–12 months postoperatively. Patients were advised to attend regular follow-up visits at the outpatient clinic. At each follow-up visit, anteroposterior and lateral radiographs of the elbow were obtained and the postoperative function and appearance of the elbow were evaluated. The fracture healing was defined as blurred fracture lines with continuous callus passing through the fracture lines on radiological examination. We used the Flynn criteria19 and Mayo Elbow Performance Score (MEPS)20 to assess the elbow function at the latest follow-up.
Results
General Results
This retrospective study included 19 patients aged between 4 and 11 years (average age, 6.6 years). The demographic information, fracture type, and surgical outcome are summarized in Table 1. There were 12 patients with IV type and others with V type lateral condyle fractures of the humerus according to Song classification. Thirteen patients had Mayo type IA and others were Mayo type IIA olecranon fractures. The average operation duration was 65 min (range, 53–76 min). The average follow-up period was 33 months, with a minimum follow-up of 24 months. The primary etiology was a fall with the forearm contacting the ground. For Mayo type IIA olecranon fractures, three patients were treated by ORIF using TBW, while another three were treated by ORIF with a locking plate.
| Case | Age (years) | Sex | Song classification | Mayo classification | Operations for humeral lateral condyle | Operations for ulnar olacranon | Operation duration (min) | Follow-up (mo) | Flynn | MEPS |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 4 | M | IV | IA | BP | CRPP | 62 | 32 | Good | 95 |
| 2 | 6 | F | IV | IIA | BP | TBW | 75 | 30 | Excellent | 95 |
| 3 | 7 | M | V | IA | BP | CRPP | 63 | 26 | Good | 95 |
| 4 | 4 | M | IV | IA | BP | CRPP | 53 | 70 | Excellent | 100 |
| 5 | 5 | F | IV | IA | BP | CRPP | 55 | 39 | Excellent | 95 |
| 6 | 4 | F | IV | IIA | BP | TBW | 72 | 36 | Excellent | 95 |
| 7 | 8 | M | V | IA | BP | CRPP | 65 | 28 | Excellent | 95 |
| 8 | 10 | M | IV | IA | BP | CRPP | 62 | 24 | Excellent | 95 |
| 9 | 7 | F | IV | IA | BP | CRPP | 66 | 36 | Good | 90 |
| 10 | 6 | M | IV | IA | BP | CRPP | 61 | 30 | Excellent | 95 |
| 11 | 11 | M | V | IIA | BP | LP | 75 | 24 | Excellent | 95 |
| 12 | 5 | M | IV | IA | BP | CRPP | 58 | 35 | Good | 95 |
| 13 | 9 | F | V | IA | BP | CRPP | 63 | 31 | Excellent | 95 |
| 14 | 6 | M | IV | IA | BP | CRPP | 70 | 27 | Excellent | 95 |
| 15 | 6 | M | V | IA | BP | CRPP | 57 | 32 | Excellent | 95 |
| 16 | 8 | F | V | IIA | BP | LP | 69 | 28 | Good | 90 |
| 17 | 9 | F | IV | IIA | BP | LP | 68 | 26 | Excellent | 95 |
| 18 | 6 | M | V | IIA | BP | TBW | 76 | 34 | Good | 95 |
| 19 | 5 | F | IV | IA | BP | CRPP | 65 | 36 | Excellent | 95 |
- Abbreviations: BP, bioabsorbable pins; CRPP, closed reduction with percutaneous pinning; F, female; LP, locking plate; M, male; MEPS, Mayo elbow performance score; TBW, tension band wires.
Complications and Clinical Outcomes
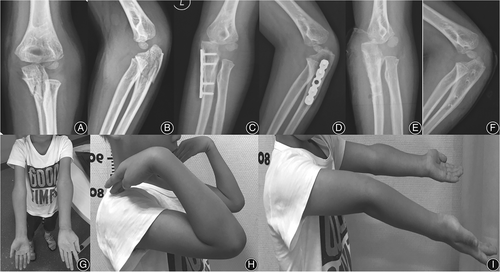
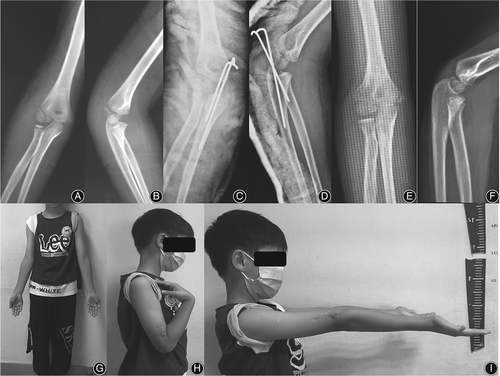
There were no complications, such as nonunion, malunion, delayed union, postoperative redisplacement, or infection. All patients achieved bony union by 12 weeks postoperatively. According to the Flynn criteria, the outcome was “excellent” in 13 cases and “good” in six cases. The MEPS was 90 points for two patients, 95 points for 16, and 100 points for one. A typical case treated with bioabsorbable pins and locking plate is shown in Figure 1. Another typical case treated with bioabsorbable pins and CRPP is shown in Figure 2.
Discussion
A reasonable hypothesis for the mechanism of combined lateral humeral condyle and ipsilateral olecranon fractures in children was proposed based on a total of 19 patients (8 girls and 11 boys) with this rare injury treated in our institute. Satisfactory clinical outcomes were achieved in an average follow-up of 33 months.
Possible Mechanism of Injury
A fracture of the lateral condyle of the humerus is the second most common pediatric elbow fracture and is less commonly seen in adults.2 In contrast, olecranon fractures are common among adults but rare in children.5 This phenomenon can be attributed to the differences in the causes of the fractures and differences in sclerotin levels among children and adults. The bone mineral density is lower in children than in adults; this makes the surrounding ligaments and muscles stronger than the bone in children, thus leading to an increased possibility of avulsion fractures in children.21-23 Moreover, compared with adult bones, pediatric bones are more flexible with a thick periosteum and more cartilage and are, therefore, more likely to be bent rather than fractured under compression force, which may explain the low prevalence of pediatric olecranon fractures.24
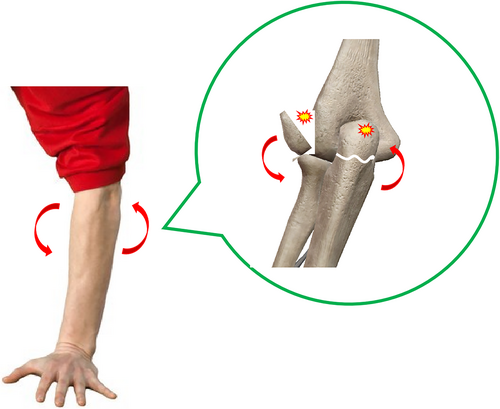
Combined fractures of the lateral condyle of humerus and ipsilateral olecranon are rarely seen, and only a few studies have reported this type of injury. The injury patterns are also debatable. The elbow is a dynamic complex joint that comprises ulnohumeral, radiocapitellar, and proximal radioulnar joints encircled within a synovial capsule.25 When one of the joints is injured, the other parts are compromised, leading to increased joint instability and the possibility of simultaneous complex injuries. Based on the present study findings, we propose the following hypothesis for the mechanism of combined fractures of the lateral humeral condyle and ipsilateral olecranon (Figure 3). Such fractures usually occur when children fall onto their outstretched and supinated elbow. Bony compression is an important contributor. During a fall, upward cubitus varus stress is transmitted axially through the ulnohumeral and radiocapitellar joints to the humerus, causing lateral condyle fracture. The olecranon is also compressed axially by the trochlea of the humerus and levered by the olecranon fossa as the forearm is relatively varus to the distal humerus when the elbow is in varus position, leading to fracture. Indirect forces exerted by muscles and ligaments may play a more important role in the etiology of combined fractures. There is opposite movement between the ulna and the humerus as the forearm externally rotates against the distal humerus; however, the shaft of the ulna is less affected and relatively fixed, making the olecranon the main stress point. When the relative motion exceeds the bearing capability of the proximal ulna, the olecranon will be compressed tightly by the trochlea both vertically and horizontally and pulled off the lateral condyle due to the tensed lateral collateral ligament complex, thus resulting in a spiral or transverse fracture of the olecranon and avulsion of the lateral condyle;7, 9-11 this was the most common fracture type in the present study. Contracted triceps muscles and arm extensors also accelerate the separation of the olecranon and lateral condyle during the process. However, a local direct blow may also cause this rare type of combined fracture in some situations.12
Surgical Management
A lateral condyle fracture with displacement of >2 mm requires surgical fixation, and K-wires or screw fixation are recommended.2, 18 However, considering the secondary damage that occurs while removing the implant, bioabsorbable pins were used for stabilization in the present study. The bioabsorbable material is compatible with tissue and avoids complications of the second surgery.26 However, longer follow-up is required to identify any bony abnormalities and inflammatory reactions in response to the bioabsorbable materials.14, 27 Furthermore, although conservative management is favored in treating minimally displaced olecranon fractures (<2 mm),28 we performed CRPP with K-wire fixation because of the joint instability caused by the associated lateral humeral condyle fracture. Most olecranon fractures classified as Mayo type IIA were treated with TBW, which is the standard method for stable fractures.29, 30 Only three patients had a locking plate inserted because they had larger fracture fragments. All patients achieved satisfactory outcomes, and there was no significant difference in surgical outcomes in terms of range of motion and appearance. This may be due to the better remodeling ability in young children and optimal surgical management.
Limitations and Strengths
The present study has some limitations, although this is the largest known published series of pediatric patients with combined fractures of the lateral humeral condyle and ipsilateral olecranon. First, there was no control group and the sample size was small due to the rarity of this injury. Second, the mechanism of injury is just a proposal that was not proved by model experiments or other methods. Third, the Mayo classification may not be appropriate for the evaluation of ulnar olecranon fractures in children. Further studies with large sample size and biomechanical studies to support the mechanism hypothesis are needed. However, the present study analyzed a number of pediatric patients and described a plausible mechanism, despite the low incidence of this rare injury. This retrospective study describes valuable experience in treating this kind of injury pattern with satisfactory clinical results during an average follow-up of 33 months.
Conclusion
Combined fractures of the lateral condyle of the humerus and the ipsilateral olecranon are rarely seen in children. We proposed a reasonable hypothesis for this unusual fracture pattern and achieved satisfactory treatment outcomes.
Acknowledgements
This research received no external funding.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The authors declare no conflict of interest.
Ethics Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Although the data were collected anonymized and centrally, all guardians of patients signed written informed consent for participate.
The Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology (IORG No: IORG0003571) gave final APPROVAL on 20 November 2019 for the study Retrospective Re-search of Surgical Methods in the Treatment of Fractures and malformation in Children conducted by Xin Tang at the Department of Orthopedic Surgery, Union Hospital of Tongji Medical College, Huazhong University of Science and Technology.
Author Contributions
Z.Z.W., L.Z.O.Y., and J.T.L. were involved in data collection and follow-up assessments. X.T. and W.F.L. were responsible for literature search and study design. S.L. and L.Q.P. drafted the manuscript., and X.T. and W.F.L. finalized the manuscript.
Disclosure Statement
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors, and all authors are in agreement with the manuscript.
Open Research
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.