Predicting Union, Osteomyelitis, and Amputation Outcomes of Gustilo IIIC Open Tibial Fractures: A Retrospective Study
Shih-Heng Chen and Po-Hao Lien contributed equally to this work.
Abstract
Objective
Open tibial fractures are frequently encountered in high-energy traumas and can result in significant complications such as nonunion, osteomyelitis, and even amputation. Among open tibial fractures, Gustilo type IIIC cases are particularly challenging due to the concomitant occurrence of neurovascular injuries and soft tissue defects. This study aimed to assess factors that affect union time and complications in Gustilo IIIC tibial fractures.
Methods
Patients who presented at our center with IIIC open tibial fractures from January 2000 to October 2020 were eligible for this retrospective analysis. Patient demographics, fracture characteristics, and the timing, number, and type of surgical intervention were documented. Outcomes of interest included union time, occurrence of osteomyelitis, and amputation. We performed univariate analyses including chi-squared test, Fischer's exact test, analysis of variance, and Kruskal–Wallis test based on the normality of the data and multivariate analyses including Cox proportional hazards model and logistic regression analyses.
Results
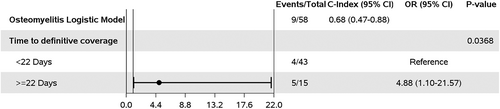
Fifty-eight patients were enrolled and grouped by fracture healing time; eight had timely union (13.8%); 27 had late union (46.6%); eight had delayed union (13.8%); three had nonunion (5.2%); and 12 underwent amputation (20.7%). Nine fractures (15.5%) were complicated by osteomyelitis. Union time was prolonged in cases of triple arterial injury, distal third fractures, multiple trauma with injury severity score (ISS) ≥ 16 points, and increased bone defect length. Additionally, a bone gap >50 mm, diabetes mellitus, low body mass index, and triple arterial injury in the lower leg were significant risk factors for amputation. A time from injury to definitive soft tissue coverage of more than 22 days was the major risk factor for osteomyelitis. A scoring system to predict union time was devised and the predicted probability of union within 2 years was stratified based on this score.
Conclusion
IIIC tibial fractures involving the distal third of the tibia, fractures with bone defects, triple arterial injury, and multiple trauma with ISS ≥16 points demonstrated delayed union, and an effective prediction system for union time was introduced in this study. Early soft tissue coverage can reduce the risk of osteomyelitis. Finally, diabetes and severe bone and soft tissue defects pose a higher risk of amputation.
Introduction
Tibial fractures are the most common type of long bone fractures, and approximately 24% of these cases are open fractures.1 Nearly 60% of open tibial fractures are Gustilo–Anderson type III fractures, indicating a high-energy breakage that often results from motor vehicle collisions or falls.2 Gustilo type III fractures are generally subdivided into IIIA (adequate soft tissue coverage of the bone), IIIB (bone exposure), and IIIC (compromised arterial circulation).3 Soft tissue severance, contamination, and vascular compromise in IIIC fractures increase the risk of subsequent infection, nonunion, and need for amputation, and may lead to psychological stress and economic difficulties.4
Adequate blood supply is a crucial factor in fracture union.5 In type IIIC tibial fractures, the anterior tibial artery (ATA), posterior tibial artery (PTA), and peroneal artery are often damaged and require immediate revascularization to avoid reperfusion injury.6, 7 After initial management to restore circulation, conversion to definitive internal fixation is best deferred until adequate soft tissue coverage of the tibia and neurovascular structures has occurred and infection has been ruled out.
Predictive tools addressing whether a severe fracture will heal successfully or whether it is likely to result in nonunion would benefit fracture-related clinical practices. An effective tool to predict the likelihood of serious complications would enable clinicians to administer relevant interventions at earlier stages. Despite the consensus that more complicated fractures and delayed soft tissue coverage might delay union,8-12 few studies have identified cut-off values to predict the outcomes of type IIIC open tibial fractures.13-16 Other studies have reported predictive outcomes for Gustilo tibial fractures in general but not specifically for IIIC tibial fractures.13-16
This study aimed to: (i) determine the prognostic factors for union time, osteomyelitis, and amputation in open IIIC tibial fractures by reviewing cases that occurred over a period of two decades in a single tertiary trauma center; and (ii) propose a scoring system created based on the analytical results to predict the union time of these types of fractures.
Methods
This retrospective chart review study involving human participants was conducted in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study protocol was approved by the Institutional Review Board of our hospital (IRB No.: 202000632B) that waived the requirement for informed consent due to the retrospective nature of the study.
Inclusion Criteria
Patients with open tibial fractures, who were treated in a single tertiary trauma center between January 2000 and October 2020, were eligible for inclusion. The inclusion criteria were: (i) Gustilo type IIIC tibial fractures caused by trauma; (ii) arterial injuries requiring revascularization for limb salvage, including occlusion or rupture of the ATA, PTA, peroneal artery, or popliteal artery; and fracture involving the tibial plateau, proximal and distal metaphyses, and diaphysis. The exclusion criteria were: (i) type IIIC ankle malleolar fractures; (ii) referral from other hospitals for the management of complications; (iii) re-fracture(s) due to falls or motor vehicle accidents during recovery; and (iv) insufficient clinical or radiographical data.
Data Collection
Time Points and Contents of the Follow-up
Patients who were discharged from our institution underwent follow-up at different intervals based on their recovery progress: (i) 1 week, (ii) 1 month, (iii) 3 months, (iv) 6 months, and (v) 12 months. If patients exhibited limited progression, they were scheduled for follow-up at the same interval. However, if progress was observed, the patient's revisit interval was extended. During these regular follow-ups, patients underwent radiographic examinations, received consultations for pain control, and underwent assessment for functional performance in daily activities.
Demographics and Injury Characteristics
Age, sex, body mass index (BMI), comorbidities, fracture location, associated fractures, injured vascular structure, mangled extremity severity score, length of bone defect, soft tissue defect area, surgical site infection status, and osteomyelitis status were recorded.
Surgical Interventions
Characteristics of internal and external fixations, the primarily anastomosed or revascularized artery, time from injury to definitive soft tissue coverage, and number and type of flap surgeries were also recorded. Lastly, additional interventions such as vascularized bone grafts (VBGs), non-vascularized bone grafts (NVBGs), or the Masquelet technique were recorded.
Definition of Included Variables
Proximal fractures included fractures involving the tibial plateau and proximal metaphysis of the tibia. Diaphysis fractures involved the middle third of the tibia, while distal fractures involved the distal metaphysis of the tibia, excluding malleolar fractures. Bone defect length was defined as the length between the proximal and distal ends of the fracture and measured after surgical removal of devitalized bones. Multiple trauma was defined as an injury severity score (ISS) of more than 16 points alongside internal organ laceration, intracranial hemorrhage, and/or hypovolemic shock. The soft tissue defect area was defined as the area of exposed bone requiring flap coverage.
Outcome Stratification
Patients were divided into the following groups based on the fracture healing time: on time (union within 1 year), late (union between 1 and 2 years), delayed (union >2 years), nonunion (no union or limited progress on radiographs before the patient discontinued care at our hospital), or amputation. In cases where a patient exhibited limited progress on the radiographs but discontinued care at our hospital by 1 year, they were excluded from the study. Only patients who completed a full 2-year follow-up and demonstrated limited progression were categorized into the nonunion group. Union was confirmed when partial weight-bearing on the affected bone was possible, along with a radiographic union score for tibial fractures of ≥ 10, as measured by three board-certified orthopedic surgeons.17 If the interpretations between two of the authors (junior surgeons) were consistent, the result was reported. When there was disagreement in interpretations between the junior surgeons, a senior surgeon interpreted the images for the final decision.
Statistical Analysis
Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). Univariate analysis of categorical variables was conducted using the chi-squared test or Fischer's exact test. The mean and median values of continuous variables were compared using analysis of variance or Kruskal–Wallis tests. For multivariate analysis, a Cox proportional hazards model (with a follow-up duration of 2 years), logistic regression, and stepwise modeling were conducted to identify the predictive factors for union time and adverse outcomes such as osteomyelitis and amputation. P-values of less than 0.05 were considered to indicate a significant difference. Nonunion and amputation were regarded as adverse outcomes and grouped for stepwise modeling. Since the Cox proportional hazards model is essentially a regression model for investigating the association between the survival time of patients and predictors, the beta coefficient of predictors from the stepwise modeling was chosen to create a scoring system. We determined the beta coefficients of associated injury, tibial distal third fracture, multiple injury with an ISS > 16, and bone defect to be 1.92, 0.8, 1.53, and 0.22, respectively. We then divided the beta coefficients by the lowest one and rounded the obtained values to the nearest whole number, resulting in 9, 4, 7, and 1, respectively. Then, we assigned values from 0 to 9 for every tenth percentile in the bone defect length of our cohort. Subsequently, we applied the scoring system to our cohort individually, arranged these scores in ascending order, and grouped these scores into 20 lowest, 19 intermediate, and 19 highest scores. Finally, we determined the predicted probability of union within 2 years for all the three groups, and examined whether there was statistical difference between the groups.
Results
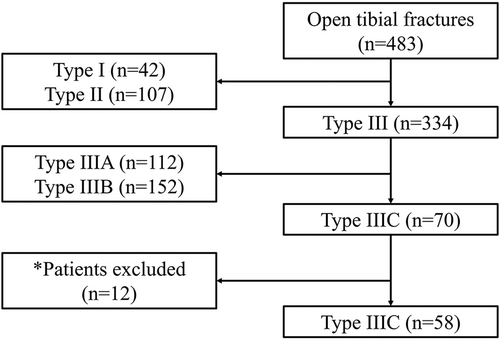
Of the 483 patients eligible for this study, 70 patients with type IIIC open tibial fracture were reviewed. Fifty-eight patients who met the inclusion criteria (45 men and 13 women) were included in the analysis. The enrollment process is illustrated in Figure 1. The demographic data and injury characteristics of the enrolled patients are shown in Tables 1 and 2.
| Characteristics | No. (%) |
|---|---|
| Mean age ± SD, years | 35.8 ± 16.6 |
| Sex | |
| Male | 45 (77.6) |
| Female | 13 (22.4) |
| BMI ± SD | 23.9 ± 4.6 |
| Diabetes mellitus | 5 (8.6) |
| Other chronic diseasesa | 4 (6.9) |
| Smoking | 19 (32.8) |
| Other substance abuse | 3 (5.2) |
- a Other chronic diseases included two patients with hepatitis C and two cases of chronic kidney disease comorbid with hypertension.
- Abbreviations: BMI, body mass index; SD, standard deviation.
| Characteristics | No. (%) |
|---|---|
| Fracture location | |
| Proximal | 8 (13.8) |
| Middle | 10 (17.2) |
| Lower | 22 (37.9) |
| Upper and middle | 4 (6.9) |
| Upper and lower | 11 (19) |
| Middle and lower | 3 (5.2) |
| Multiple trauma with ISS ≥16 points | 9 (15.5) |
| MESS ± SD | 5.6 ± 1.5 |
| Osteomyelitis | 9 (15.5) |
| Surgical site infection | 35 (60.3) |
| Length of bone defect ± SD, mm | 38.8 ± 37.6 |
| Soft tissue defect area ± SD, cm2 | 201.86 ± 148.5 |
| Type of internal fixation | |
| Intramedullary nail | 17 (29.3) |
| Plate | 29 (50) |
| Did not receive internal fixation | 12 (20.7) |
| Type of soft tissue coverage | |
| Free flap | 37 (63.8) |
| Local flap | 8 (13.8) |
| Primary closure | 3 (5.2) |
| Did not receive soft tissue reconstruction | 10 (17.2) |
| Injured arterial structure | |
| Anterior tibial artery (ATA) | 13 (22.4) |
| Posterior tibial artery (PTA) | 9 (15.5) |
| Peroneal artery (PEA) | 1 (1.7) |
| Popliteal artery (POPA) | 9 (15.5) |
| ATA and PTA | 10 (17.2) |
| ATA and PEA | 2 (3.4) |
| ATA and POPA | 2 (3.4) |
| PTA and PEA | 3 (5.2) |
| ATA and PTA and PEA | 9 (15.5) |
- Abbreviations: ATA, anterior tibial artery; MESS, mangled extremity severity score; PEA, Peroneal artery; POPA, Popliteal artery; PTA, posterior tibial artery; SD, standard deviation.
Eleven cases had popliteal artery injury, including four tibial plateau fractures, three proximal tibial shaft fractures, two tibial plateau and proximal metaphysis fractures, and two tibial diaphysis fractures with extensive avulsion injury. The mean length of bone defect, area of bone exposure requiring flap coverage, and tissue coverage details are documented in Table 2. Two fractures initially treated with free flap coverage resulted in amputation. Further, soft tissue reconstruction was not performed in 10 cases as progressive soft tissue necrosis after revascularization led to amputation. All external fixations were used as initial temporary fixations, and the duration of some external fixation applications were prolonged due to multiple traumas or large areas of soft tissue defect that required additional stabilization via external fixators.
Union Time and Related Influencing Factors
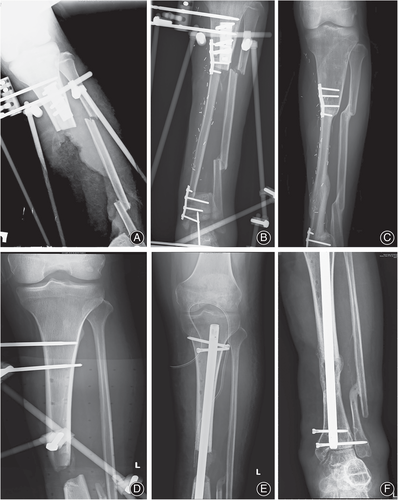
Univariate analysis results of union time are shown in Table 3. Data for the 12 amputation (20.7%) cases are not shown. The mean union time for patients with or without an ISS ≥16 points were 774 ± 348 days and 499 ± 238 days, respectively (p = 0.03). Among the nine patients with an ISS ≥16 points, six (66.7%) experienced hypovolemic shock, one (11.1%) had intracranial hemorrhage, one (11.1%) had rhabdomyolysis after trauma with resultant renal failure, and one (11.1%) had a cervical spine injury. Figure 2 demonstrates the pre-operation, post-operation, and united fracture radiographic images of our cohort.
| Covariate | Union on time |
Late union |
Delayed union | Nonunion | p-value | |
|---|---|---|---|---|---|---|
| N=8 | N=27 | N=8 | N=3 | |||
| Age, mean (SD) | 33 (16.72) | 38 (15.72) | 30.13 (12.61) | 24 (2.65) | 0.269 | |
| Sex (%) | 0.677 | |||||
| Female | 1 (12.5) | 4 (14.81) | 2 (25) | 1 (33.33) | ||
| Male | 7 (87.5) | 23 (85.19) | 6 (75) | 2 (66.67) | ||
| BMI mean (SD) | 25.43 (3.29) | 24.2 (3.41) | 26.03 (7.16) | 22.47 (7.21) | 0.661 | |
| DM (%) | 1 (12.5) | 1 (3.7) | 0 (0) | 0 (0) | 0.661 | |
| Fracture location (%) | 0.841 | |||||
| Upper | 2 (25) | 5 (18.52) | 1 (12.5) | 0 (0) | ||
| Middle | 2 (25) | 3 (11.11) | 1 (12.5) | 1 (33.33) | ||
| Lower | 3 (37.5) | 10 (37.04) | 3 (37.5) | 1 (33.33) | ||
| Upper and middle | 1 (12.5) | 2 (7.41) | 1 (12.5) | 0 (0) | ||
| Upper and lower | 0 (0) | 6 (22.22) | 2 (25) | 0 (0) | ||
| Middle and lower | 0 (0) | 1 (3.7) | 0 (0) | 1 (33.33) | ||
| ATA injury (%) | 5 (62.5) | 14 (51.85) | 5 (62.5) | 3 (100) | 0.506 | |
| PTA injury (%) | 5 (62.5) | 12 (44.44) | 5 (62.5) | 1 (33.33) | 0.623 | |
| Peroneal A injury (%) | 1 (12.5) | 5 (18.52) | 1 (12.5) | 0 (0) | 1.000 | |
| Popliteal A injury (%) | 1 (12.5) | 8 (29.63) | 1 (12.5) | 0 (0) | 0.659 | |
| Vascular injury (%) | 0.885 | |||||
| 1 artery | 5 (62.5) | 16 (59.26) | 5 (62.5) | 2 (66.67) | ||
| 2 arteries | 2 (25) | 10 (37.04) | 2 (25) | 1 (33.33) | ||
| 3 arteries | 1 (12.5) | 1 (3.7) | 1 (12.5) | 0 (0) | ||
| MESS score mean (SD) | 5.38 (2) | 5.78 (1.63) | 4.88 (0.99) | 4.33 (0.58) | 0.222 | |
| Bone gap length mean (mm) (SD) | 28.22 (24.63) | 25.94 (18.43) | 40.51 (24.1) | 39.06 (28.83) | 0.387 | |
| Soft tissue defect area mean (cm2) (SD) | 273.6 (176.89) | 238 (120.55) | 193.5 (117.52) | 228.67 (36.68) | 0.700 | |
| Deep wound infection before osteosynthesis (%) | 4 (57.14) | 12 (46.15) | 4 (50) | 0 (0) | 0.465 | |
| Deep wound infection after osteosynthesis (%) | 5 (71.43) | 15 (55.56) | 6 (75) | 2 (66.67) | 0.814 | |
| Osteomyelitis before osteosynthesis (%) | 1 (14.29) | 1 (3.7) | 1 (12.5) | 0 (0) | 0.423 | |
| Osteomyelitis after osteosynthesis (%) | 1 (14.29) | 5 (18.52) | 2 (25) | 1 (33.33) | 0.766 | |
| Duration of external fixation mean (days) (SD) | 138.14 (67.19) | 104.59 (70.4) | 100.57 (57.08) | 142.67 (120.83) | 0.400 | |
| Time of injury to osteosynthesis mean (days) (SD) | 110.43 (60.58) | 67.92 (53.53) | 92 (71.11) | 98.33 (71.81) | 0.377 | |
| Exchange of internal fixation (%) | 0.437 | |||||
| 0 | 7 (100) | 21 (77.78) | 7 (87.5) | 2 (66.67) | ||
| 1 | 0 (0) | 4 (14.81) | 0 (0) | 0 (0) | ||
| 2 | 0 (0) | 1 (3.7) | 1 (12.5) | 0 (0) | ||
| 3 | 0 (0) | 1 (3.7) | 0 (0) | 1 (33.33) | ||
| Nonvascularized bone graft (%) | 2 (25) | 16 (59.26) | 6 (75) | 3 (100) | 0.089 | |
| Nonvascularized bone graft numbers (%) | 0.965 | |||||
| 1 | 2 (100) | 11 (68.75) | 4 (66.67) | 2 (66.67) | ||
| 2 | 0 (0) | 2 (12.5) | 0 (0) | 0 (0) | ||
| 3 | 0 (0) | 3 (18.75) | 2 (33.33) | 1 (33.33) | ||
| Time to definitive coverage mean (days) (SD) | 16.63 (9.47) | 14.85 (10.07) | 20.63 (10.32) | 10.67 (8.5) | 0.450 | |
| Free flap (%) | 7 (87.5) | 18 (66.67) | 7 (87.5) | 3 (100) | 0.454 | |
| Local flap (%) | 5 (62.5) | 15 (55.56) | 5 (62.5) | 2 (66.67) | 1.000 | |
| Vascularized bone graft or Masquelet (%) | 0.248 | |||||
| Neither | 5 (62.5) | 23 (85.19) | 5 (62.5) | 2 (66.67) | ||
| VBG | 1 (12.5) | 1 (3.7) | 2 (25) | 0 (0) | ||
| Masquelet | 2 (25) | 3 (11.11) | 1 (12.5) | 1 (33.33) |
- Notes: The parametric p-value was calculated by analysis of variance for numerical covariates and chi-squared test for categorical covariates. Non-parametric p-values were calculated by the Kruskal–Wallis test for numerical covariates and Fischer's exact test for categorical covariates.
- Abbreviations: ATA, Anterior tibial artery; BMI, Body mass index; DM, Diabetes mellitus; ISS, Injury severity score; MESS, Mangled extremity severity score; PTA, Posterior tibial artery; SD, Standard deviation; VBG, Vascularized bone graft.
Regarding cases with larger bone defects (mean ± standard deviation = 57.12 ± 17.76 mm), four patients underwent VBG (mean defect length ± standard deviation = 68.33 ± 7.05 mm), and seven underwent the Masquelet technique (mean defect length ± standard deviation = 52.91 ± 19.04 mm; p-value between VBG and Masquelet = 0.216). The defect length in patients who underwent either VBG or Masquelet and those who did not was 57.11 ± 17.76 mm and 27.33 ± 29.14 mm (p = 0.003), respectively. The mean union time for cases that underwent VBG and Masquelet procedures was 714 ± 449 and 540 ± 234 days, respectively (p = 0.166). The mean union times were of those who underwent either VBG or Masquelet and those who did not was 603 ± 318 and 505 ± 242 days, respectively (p = 0.190).
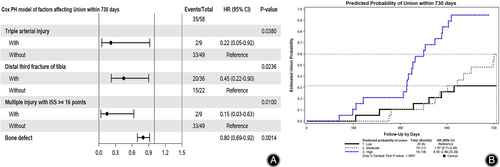
Multivariate analysis demonstrated that triple arterial injury, distal third fracture, bone defect, and multiple trauma with an ISS ≥16 points were significant adverse factors in achieving union within 2 years. A forest plot of the multivariate model is shown in Figure 3a. Based on the Cox proportional hazards model, we proposed a scoring system to predict the probability of union within 2 years (Tables 4 and 5). Furthermore, our cohort was equally divided into the following three groups: low, moderate, and high based on the estimated probability of union by the Cox proportional hazards model. The scoring system was validated using a Kaplan–Meier plot. The mean scores of each group from low to high probability of union were 15.7, 8.7, and 4.0, respectively, and the mean probabilities of union within 2 years were 19%, 79%, and 85%, respectively. Higher scores implied a higher probability of nonunion after 2 years. A significant difference was observed in the union time between the high versus moderate, and high versus low groups (p < 0.0001; Figure 3b). The results suggested significant differences between groups, indicating that valid grouping was achieved.
| Yes | No | |
|---|---|---|
| Multiple trauma with ISS ≥16 points | +9 to score | 0 points |
| Triple arterial injury | +7 to score | 0 points |
| Distal third fracture | +4 to score | 0 points |
| Bone defecta | (+ different points according to defect size) | 0 points |
- Abbreviations: ISS, injury severity score.
- a Bone defect length (mm) was stratified as follows: 0 points: < 6 mm; 1 point: 6–10 mm; 2 points: 10–16 mm; 3 points: 16–23 mm; 4 points: 23–30 mm; 5 points: 30–39 mm; 6 points: 39–41 mm; 7 points: 41–60 mm; 8 points: 60–72 mm; 9 points: >72 mm.
| Score | Probability of union within 2 years (stratified to every tenth probability percentile) |
|---|---|
| 0 to 1 | 85–95% |
| 2 | 75–85% |
| 3 to 4 | 65–75% |
| 5 | 55–65% |
| 6 | 45–55% |
| 7 to 8 | 35–45% |
| 9 to 10 | 25–35% |
| 11 to 12 | 15–25% |
| 13 to 18 | 5–15% |
| 19 to 29 | <5% |
The multivariate analysis identified key factors contributing to the occurrence of osteomyelitis and amputation. A longer time from injury to definitive soft tissue coverage (i.e., soft tissue flaps), specifically exceeding 22 days, significantly increased the risk of osteomyelitis. Regarding amputation, our analysis revealed that patients with diabetes mellitus, a bone defect larger than 50.44 mm, and triple arterial injury had a higher risk of amputation.
Discussion
Gustilo type IIIC fractures of the tibia might result in nonunion, surgical site infection, osteomyelitis, and/or amputation.4 Various factors that may influence the union time of open tibial fractures have been proposed in the literature.8, 10 In this study, we identified several factors associated with prolonged union time. These factors included triple arterial injury, distal third tibial fractures, multiple injuries, and larger bone defects. Moreover, the risk of osteomyelitis increased when definitive soft tissue coverage was delayed beyond 3 weeks. Furthermore, specific patient characteristics and injuries were found to be correlated with a higher likelihood of amputation. Patients with diabetes mellitus (DM), lower BMI, bone defects larger than 5 cm, and triple arterial injuries were more likely to undergo amputation.
Delayed Union, Nonunion, and Related Predicting Factors
Previous studies have reported predictive factors for different outcomes in cohorts with mixed type Gustilo tibial fractures13-16 (Table 6). However, this is the first retrospective study dedicated to predicting the prognosis of type IIIC tibial fractures, specifically regarding union time, development of osteomyelitis, and need for amputation. In our study, in cases where a patient presented with a higher score, more aggressive debridement and sequestrectomy might have been performed to ensure that only viable tissue was preserved. In addition, the Masquelet technique or the use of a vascularized bone flap might have been contemplated for managing potential osteomyelitis or more substantial bony and soft tissue defects. In a previous study that exclusively focused on IIIC tibial fractures, Soni et al.13 followed 18 patients with type IIIC fractures and discovered that injury to the PTA was correlated with an increased rate of nonunion. This is probably because the PTA is the major nutrient artery of the tibia, the tibial periosteum, and the posterior muscular envelope. The PTA perfuses the inner two-thirds of the diaphyseal cortex of the tibia, while the outer third is supplied by the periosteum. Thus, PTA injury, with severance of the posterior envelope in distal fractures, may prevent tibial union.
| IIIC case numbers | Other type case numbers | Prolonged union time | Deep infection | Amputation | Additional findings | |
|---|---|---|---|---|---|---|
| Soni et al.13 | 18 | Nil | Distal tibial fracturesa | Nil | Nil | MESS was the predictor of functional outcome |
| Chua et al.14 | 8 | 81 type IIIB | Flap coverage time was irrelevant | Flap coverage time beyond 72 hours | Flap coverage time was irrelevant | Nil |
| Rounds et al.15 | 3 | 1 type I, 9 type II, 1 type IIIA, 16 type IIIB | Nil | Nil | Nil | Local flap was the predictor of ambulation at discharge |
| Whiting et al.16 | 6 | 393 type I 398 type II 208 type IIIA 55 type IIIB |
Nil | Longer time from injury to definitive surgery; Longer time from injury to wound closure | Nil | Nil |
- a When associated with posterior tibial artery damage.
We observed that 5.2% of patients still had nonunion at their two-year follow-up, comparable with findings of 7.4% and 6.8% nonunion in tibial fractures of all types, as reported previously.18, 19
In our cohort, the proportion of cases with multiple trauma or triple arterial injury that achieved union within 2 years was significantly lower compared with that of those without either condition. One patient had multiple trauma and triple arterial injury simultaneously. A slightly longer mean union time was noted for distal third tibial fractures compared with fractures that did not involve the distal tibia, but this difference was not statistically significant. Bone defect length significantly affected union time in univariate analysis and the multivariate model, and the probability of union within 2 years decreased with increases in bone defect length.
Location of Fracture Sites
Distal third tibial fractures have been proposed to adversely affect the healing of open tibial fractures.13, 20-22 Stranix et al.20 proposed that these fractures are commonly complicated by damage to the PTA and peroneal artery, which usually implies more serious impacts during trauma than injuries to the ATA at the middle third of the tibia. A study of 18 patients with type IIIC fractures found that PTA injury was associated with an increased rate of nonunion.13 Fractures with PTA injury generally required more than 2 years to unite and required higher rates of amputation compared with that observed with those without PTA injury; however, these results were not statistically significant.
Multiple Associated Injury
Six patients with an ISS ≥16 points, which was a risk factor for nonunion in this study, had trauma-associated hypovolemic shock, and reconstructions were deferred until the patient's vital signs had stabilized. Bundkirchen et al.23 evaluated healing processes after hemorrhagic trauma in a mouse model, which revealed a reduced callus density. Subsequently, they concluded that healing is impeded when severe hemorrhagic shock occurs.
Length of Bone Defect
A bone gap >40 mm was associated with delayed union or nonunion/amputation in the multivariate model, while fractures with a bone gap <30 mm tended to heal within 2 years. A randomized controlled trial of tibial fractures proposed 1 cm or 50% of the circumference of the tibial diaphyseal defect as a critical cut-off for bone defect size.24 However, a systematic review by Azi et al.25 found no direct relationship between the bone defect size and union rate when an NVBG was applied in open fractures of long bones. Similarly, although patients who underwent the VBG or Masquelet technique had a longer bone gap than that had by other patients in our cohort, the difference in the union time was not statistically significant between the two groups, which supports our theory that bone gap might not be the most important factor affecting union time.
Osteomyelitis and Related Predicting Factors
Stepwise modeling of multivariate logistic regression of nine cases of osteomyelitis revealed that time from injury to definitive soft tissue coverage which exceeded 22 days (the third interquartile in our data) significantly increased the risk of osteomyelitis (Figure 4).
Despite the consensus that soft tissue coverage within 1 week improves outcomes of severe tibial fractures,9, 26 soft tissue coverage may be delayed for many reasons.27 In our cohort, a 22-day cut-off represented the third interquartile range of time for definitive soft tissue coverage. Of the fractures with osteomyelitis, 44.4% had definitive soft tissue coverage more than 22 days after the initial trauma—these fractures were complicated by multiple traumas which delayed the timing of soft tissue coverage. Our results were consistent with a previous study, which proposed that severely traumatized tissue commonly requires more debridement to obtain a clear margin for better wound healing potential, which often delays the definitive coverage to > 2 weeks, and longer times for wound coverage independently predict infection.28 In contrast, Stranix et al. found that the timing from injury to flap coverage was not associated with increased rates of major complications in their study; however, their study focused on flap failure rate rather than infection.20
Amputation and Related Predicting Factors
Five cases of early amputation (within 1 day) and seven delayed amputations (after 1 day) were recorded within our cohort. Among the 12 amputations, nine were performed despite initial revascularization attempts, and three did not receive revascularization due to extensive soft tissue loss or avulsion injury. Multivariate logistic regression showed that diabetes, bone gap >50 mm, lower BMI, and triple arterial injury increased the risk of amputation in IIIC tibial fractures, despite attempts at revascularization (Figure 5).

There was a 20.7% amputation rate in our cohort, which was similar to the findings of 19.4% and 21% in previous studies.21, 29 Although injured arterial structures were not predictive of the union time, triple arterial injury was a risk factor for amputation in the multivariate analysis. Three of six triple arterial injury cases received immediate amputation in our cohort.
A low BMI was a significant risk factor for amputation in the multivariate analysis. Literature regarding multiple trauma has shown an “obesity paradox,” in which overall survival appeared to be higher in obese patients than in underweight patients.30, 31 One study found that a BMI < 18.4 kg/m2 was associated with increased mortality after multiple trauma.31 We surmised that a lower BMI was correlated with less subcutaneous fat coverage to cushion or protect neurovascular and bony structures.
DM has been proposed to impair healing and cause chronic wounds.32 A significantly higher amputation rate was noted in patients with DM (60%) compared with those without DM (4.3%). Piwnica-Worms et al.33 found a significant relationship between DM and amputation rate in 129 patients with lower extremity trauma who required free flap reconstruction, which corroborated our findings.
Limitations and Prospects
The present study, which focused exclusively on Gustilo IIIC fractures may serve as a preliminary investigation. Nevertheless, it is also important to acknowledge the limitations of this study due to its retrospective design. Some of the parameters included in the present study may not have been assessed accurately and may have potential reporting bias. For instance, soft tissue damage might not have been evaluated precisely and might have been underestimated. Additionally, some factors, such as postoperative rehabilitation, patient compliance, and surgeon's discrepancies, were difficult to objectively quantify for statistical analyses. Furthermore, the progression of hardware exhibited variation over the 20-year study duration. The locking plate fixation had just been reinvented and was not widely applied in the beginning of the year 2000. In addition, it is notable that fixation by locking plate gained increasing prevalence after 2010 in our cohort, potentially impacting the union rates. A prospective study design may facilitate more comprehensive and accurate parameter evaluations. Using a prospective methodology, future studies can refine the results of the present study and uncover additional predictors contributing to the promotion of treatments and outcomes.
Conclusion
In conclusion, IIIC tibial fractures with distal third tibial fractures, triple arterial injury, bone defect, or multiple trauma with an ISS ≥16 points are likely to cause delayed union. Early soft tissue coverage could be the primary intervention for reducing the risk of osteomyelitis. Lastly, severe bone and soft tissue defects, DM, and low BMI are correlated with a higher risk of amputation.
Acknowledgments
The authors want to express their gratitude for the contributions of Drs. Chen-An Hsu and Chih-Wei Chen for determining the radiographic union scores for tibial fractures in our cohort and providing valuable comments regarding the present study.
Conflict of Interest Statement
The authors declare that there is no conflict of interest regarding the publication of this paper. No funding was provided for this study.
Ethical Statement
This retrospective chart review study involving human participants was conducted in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study protocol was approved by the Institutional Review Board (IRB No.: 202000632B) of Chang Gung Memorial Hospital, Taoyuan City, Taiwan, China. The informed consent was waived due to the retrospective nature of the study by the Institutional Review Board (IRB No.: 202000632B) of Chang Gung Memorial Hospital, Taoyuan City, Taiwan, China.
Author Contributions
S.H.C., P.H.L., C.C.H., and Y.H.Y contributed to the study conception and design. Investigation, data collection, and analysis were performed by S.H.C., P.H.L, and C.Y.L. The manuscript was written by S.H.C., P.H.L, and Y.H.Y. The study was reviewed and supervised by C.H.L, Y.T.L, C.H.L., and Y.H.Y. All authors have read and approved the final manuscript. S.H.C and P.H.L. contributed equally to this work.
Funding
No funding was received for the research presented in this article.
Authorship Declaration
All authors listed meet the authorship criteria according to the latest guidelines of the International Committee of Medical Journal Editors. All authors agree with the manuscript.