The Potential Value of Monocyte to Lymphocyte Ratio, Platelet to Mean Platelet Volume Ratio in the Diagnosis of Periprosthetic Joint Infections
Grant Sources: This work was supported by the National Natural Science Foundation of China [grant numbers 8167090912].
Disclosure: All authors declare that they have no competing interests.
Abstract
Objective
To explore the possibility of obtaining more accurate information from routine blood tests for the diagnosis of periprosthetic joint infection (PJI).
Methods
This is a retrospective study. Between 2017 and 2018, a total of 246 patients who underwent total hip or knee revision surgery were included in this study. There were 146 females and 100 males, and the mean age of the patients was 62.1 ± 12.75 years. Laboratory parameters erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), D-dimer, plasma fibrinogen, serum white blood cell (WBC), and calculable ratio markers were collected. Based on leukocytes (monocyte count, neutrophil count, lymphocyte count), platelet count, and mean platelet volume Inflammation-related ratio markers were calculated, which including monocyte to lymphocyte ratio (MLR), neutrophil to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR), and platelet to mean platelet volume ratio (PMR). Follow-up of all studied cases for at least 1 year. The diagnostic value of the markers based on the receiver operating characteristic (ROC) analysis. The most optimal combinations of blood markers were selected by the prediction models. Statistical analyses and prediction models were performed using R software.
Results
Of the 246 patients, 125 were diagnosed with PJI and 121 with aseptic loosening. A higher rate of patients underwent revision surgery due to hip prosthesis loosening in the aseptic loosening group (74.4%) compared to the PJI group (45.6%, P < 0.001). ROC curves showed that the area under the curve (AUC) for classical markers, fibrinogen was 0.853 (95% confidence interval [CI], 0.805–0.901), ESR was 0.836 (95% CI, 0.785–0.887) and CRP was 0.825 (95% CI, 0.773–0.878). Followed by the PMR, PLR, NLR and MLR, which showed promising diagnostic performance with AUCs of 0.791, 0.785, 0.736, and 0.733. The AUCs of the ratio markers were higher than those of D-dimer (0.691;95% CI, 0.6243–0.7584) and serum WBC (0.622; 95% CI, 0.552–0.691). After the predictive model calculation, AUC was up to 0.923 (95% CI, 0.891–0.951) when plasma fibrinogen combined with MLR and PMR and interpreted excellent discriminatory capacity with a sensitivity of 86.40% and a specificity of 84.17%. The new combination significantly increases the accuracy and reliability of the diagnosis of PJI (P < 0.001). The AUC increased to 0.899 (95% CI, 0.861–0.931; P = 0.007) and 0.916 (95% CI, 0.880–0.946; P < 0.001), followed by CRP and ESR, respectively. All plasma fibrinogen, ESR, and CRP combined with both PMR and MLR achieved the highest specificity (89.17%) and PPV (85.34%).
Conclusion
The diagnostic performance greatly improved when plasma fibrinogen, ESR, and CRP combined with ratio markers.
Introduction
Periprosthetic joint infection (PJI) is a rare but severe complication after total joint replacement (TJA)1, 2. It is a huge economic burden not only for the individual patient but also for the global healthcare system. For primary total joint arthroplasty, the incidence of infection ranges between 1 and 3%2. The current study indicated the infection ranges after revision total joint (hips and knees) arthroplasty 3% to 8%3. However, the diagnosis of infection is still the main challenge after TJA4. Besides, accurate differentiation between septic and aseptic failure is essential to determine treatment protocols5. There is currently lacking a single gold-standard test for diagnosing PJI. Based on the 2018 International Consensus Conference on Musculoskeletal infection, Surgeons rely on a combination of a series of laboratory tests in peripheral blood and synovial fluid, microbial culture, and histopathological examinations to diagnose PJI6. Recent studies have shown that potential novel markers that need to perform joint aspiration for the diagnosis of PJI, include synovial alpha-defensin, synovial leukocyte test strips, synovial C-reactive protein7-9. However, these potential synovial markers may increase the financial burden of patients. Moreover, surgeons are often facing a lack of synovial fluid or “dry tap”, and joint aspiration is an invasive procedure with an increased risk of deep infection. Improvements in diagnostic tools, mainly to obtain more accurate diagnostic information from blood tests, are necessary.
The blood test provides surgeons with important information on inflammatory markers due to its simplicity, accessibility, and short waiting time. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are minor diagnostic criteria in 2018 ICM criteria. The reliability and usefulness of ESR and CRP for diagnosing PJI have been well studied. In a meta-analysis, the researchers noted the sensitivity and specificity were 0.860 (95% CI, 0.825–0.890) and 0.723 (95% CI, 0.704–0.742) for ESR, and for CRP were 0.869 (95% CI, 0.835–0.899) and 0.786 (95% CI, 0.769–0.803) according to the diagnostic criteria for ICM10. However, McArthur et al. indicated that both ESR and CRP are negative according to current diagnostic criteria, there are still cases involving false negatives for diagnosing PJI11. One study has also shown that the false-negative rate is 9.2 and 5.3% for ESR and CRP, respectively, combined ESR and CRP the false-negative rates up to 11.1%12. Controversy still exists due to their unclear thresholds and a negative serum ESR and CRP test result does not exclude the possibility of infection, so it is essential to obtain more accurate diagnostic information from the blood test results.
In addition to the classical inflammatory markers CRP and ESR, coagulation-related markers also showed high diagnostic efficacy in the diagnosis of PJI. Plasma fibrinogen and D-dimer have been studied by researchers for use to diagnose PJI13. Fibrinogen is a positive acute reactive protein produced by the liver and an essential component of the coagulation system. Li et al. demonstrated that the diagnostic efficacy of plasma fibrinogen was comparable to that of ESR and CRP14. Similarly, D-dimer is a fibrin degradation product, which is used as a screening tool for thrombosis and is also related to inflammation15. Some researchers noted that D-dimer showed better diagnostic efficacy than ESR and CRP levels5, 16. In addition to classic blood markers, several studies have documented that platelets and mean platelet volume (MPV) play an essential role in the inflammatory process13, 17, 18. Recent literature has shown that the combination of MPV/PC with CRP and ESR significantly improves the efficacy of diagnosing PJI19. Moreover, Huang et al. reported that peripheral blood dynamic ratio neutrophil/lymphocyte ratio (NLR) and MLR correlate with inflammatory body status20. It provides a new potential method for getting sufficient information for diagnosing PJI through a single blood test. However, more studies are needed to confirm the accuracy of ratio markers in the diagnosis of PJI and there is still a need to determine the diagnostic performance of the combination of coagulation-related markers with peripheral blood ratio markers.
In most institutions, it is usually possible to obtain a routine complete blood count by blood testing, including monocyte count, neutrophil count, lymphocyte count, platelet count, and MPV. Ratio valuables are also easy to calculate. Besides, a routine blood test can perform on all patients, particularly for those patients with “dry tap”. To the best of our knowledge, there are no studies that have evaluated the use of the combination of coagulation-related markers with peripheral blood dynamic ratio for the diagnosis of PJI.
Therefore, we hypothesized that peripheral blood indicators, coagulation-related markers combined with ratio markers maybe increase the accuracy of PJI diagnosis. The main purpose of the present study was to: (i) access the diagnostic value of ESR, CRP and coagulation-related markers; (ii) select useful ratio markers and examine the differences between bacterial species for ratio markers; and (iii) evaluate whether combined measurement provides surgeons additional information in order to diagnose PJI more accurately.
Materials and Methods
Inclusion and Exclusion Criteria
The inclusion criteria were: (i) patients diagnosed with chronic PJI or aseptic loosening (AL); (ii) patient underwent revision hip or knee arthroplasty; (iii) patients divided into two groups according to the 2014 MSIS criteria21; (iv) the major evaluation peripheral blood inflammatory biomarkers included CRP, ESR, plasma fibrinogen, d-dimer, WBC, PLR, PMR, NLR, MLR; and (v) this study is a retrospective study.
The exclusion criteria were: (i) acute PJI (defined as infection occurs within 3 months after the surgery); (ii) inflammation-related diseases include rheumatoid arthritis, systemic lupus erythematosus, and ankylosing spondylitis; (iii) revision due to periprosthetic fracture or dislocation; (iv) severe liver dysfunction or the presence of malignant tumors; and (v) insufficient serum marker data.
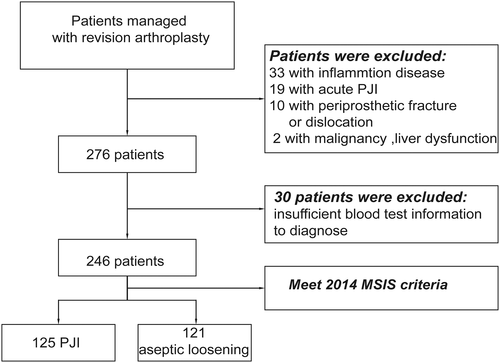
Demographics
Our institution's research ethics board approved this retrospective observational study. We enrolled patients who were managed with revision surgery after hip or knee arthroplasty from January 2017 to December 2018 at a single institution. Ultimately, 246 patients were included, of which 125 were diagnosed with PJI, and 121 were aseptic loosening (Fig. 1). The clinical records of the patient's information that included age, Body mass index (BMI), gender, surgery type (knee or hip), Charlson comorbidity index (CCI) were showed in Table 1.
| Variables | PJI group (n = 125) | Aseptic loosening group (n = 121) | P value |
|---|---|---|---|
| Age (year) | 62.8 ± 12.7 | 61.2 ± 12.8 | 0.251 |
| BMI (kg/m2) | 25.7 ± 3.9 | 25.2 ± 3.7 | 0.417 |
| Gender (%) | 0.570 | ||
| Female | 72 (57.6%) | 74 (61.2%) | |
| Male | 53 (42.4%) | 47 (38.8%) | |
| Joint | <0.001 | ||
| Knee | 68 (54.4%) | 31 (25.6%) | |
| Hip | 57 (45.6%) | 90 (74.4%) | |
| CCI (%) | 0.266 | ||
| <4 | 94 (72.8%) | 106 (87.6%) | |
| ≥4 | 31 (27.2%) | 15 (12.4%) |
- BMI, body mass index; CCI, Charlson comorbidity index; PJI, periprosthetic joint infection.
Laboratory Tests
Blood Testing and Details
As part of our routine preoperative testing, blood samples are collected the morning after admission and then sent to the Medical Laboratory Center for testing. In addition to record ESR, CRP, fibrinogen, D-dimer, WBC as main peripheral markers; we also recorded lymphocyte count, neutrophil count, platelet count, and MPV to calculate PLR, PMR, NLR, MLR as adjunct ratio markers for diagnosing PJI. The CRP level was analyzed with a special protein analyzer PA-990 (Sysmex). The ESR was measured with an automated sed rate screener SRS 100/II (Greiner Bio-One). WBC count, platelet, and MPV were determined with an automated hematology analyzer, the Sysmex XN-20 modular system (Sysmex). Plasma fibrinogen and D-dimer were quantified with an STA R Max Evolution analyzer (Diagnostica Stago). A BACT/ ALERT 3D blood culture system (BioMerieux) was used for culture, and a matrix-assisted laser desorption ionization-time of flight mass spectrometry system, VITEK-MS (BioMerieux), was used for microorganism identification.
Other Tests
Other tests include cultures, synovial leukocyte (WBC) counts, percentage of polymorphonuclear neutrophils (PMN%), and histological analysis. During the surgical procedure, about 3–5 samples (synovial fluid, deep tissue, and bone) were obtained for aerobic and anaerobic, and fungal cultures. The samples were sent to the medical laboratory center and each sample was inoculated for 14 days unless microorganisms were detected. Culture results were used for correlation analysis with ratio markers.
Statistical Analysis
All the statistical analyses were performed with the statistical software packages R (http://www.R-project.org, The R Foundation). Categorical variables were expressed as frequencies and percentages, and continuous variables were expressed as mean ± standard deviation. A comparison of the clinical characteristics between the PJI group and AL group was performed using the independent t-test or the chi-square test. The diagnostic value of each marker for PJI assessment was determined by receiver operating characteristic ROC curve analysis. Curves are considered valuable when AUC ≥ 0.7. The Youden index was used to determine the optimal threshold for classical markers (fibrinogen, ESR, CRP, D-dimer) and ratio markers (PLR, PMR, NLR, MLR). Predictive models were utilized to screen the best combination of indicators. The statistical significance was defined as P < 0.05.
Results
General Results
Demographic information is shown in Table 1. This study included 246 patients, of whom 125 (50.8%) diagnosed with PJI and 121 (49.1%) with aseptic loosening. Of these, 99 patients underwent total knee revisions, and 147 patients undergone hip revisions. The mean ages of the PJI group and AL group were 62.8 ± 12.7 years and 61.2 ± 12.8 years (P = 0.251). There were no significant statistical differences between gender (P = 0.570), BMI (P = 0.471), and CCI (P = 0.266). The aseptic loosening group had more hip joints than the PJI group (90 [74.4%] vs 57 [45.6%]; P < 0.001).
Clinical Results
Routine Blood Tests
The concentration of blood markers plasma fibrinogen, CRP, ESR, D-dimer, serum WBC, neutrophil count, monocyte count, the platelet count in the PJI group higher than the aseptic loosening group, except for lymphocyte count and mean platelet volume with statistically significant differences (P < 0.001) (Table 2).
| Markers | PJI group | Aseptic loosening group | P value | ||
|---|---|---|---|---|---|
| Mean ± SD | Median (Min-Max) | Mean ± SD | Median (Min-Max) | ||
| CRP (mg/L) | 36.74 ± 48.05 | 19.22 (0.94–257.00) | 5.77 ± 11.78 | 1.92 (0.50–81.00) | <0.001 |
| ESR (mm/h) | 42.36 ± 28.33 | 36.00 (2.00–113.00) | 13.02 ± 11.42 |
10.00 (0.20–63.00) | <0.001 |
| D-dimer (μg/mL) | 1.80 ± 1.19 |
1.63 (0.15–6.99) | 1.33 ± 1.58 |
0.84 (0.16–11.36) | <0.001 |
| Plasma Fibrinogen (g/L) | 5.74 ± 8.18 | 4.82 (2.40–95) | 3.3 ± 0.79 | 3.1 (1.73–5.50) | <0.001 |
| WBC (109/L) | 6.88 ± 2.30 |
6.36 (2.16–18.00) | 5.97 ± 1.42 | 5.75 (2.63–9.50) | <0.001 |
| Neutrophil count (109/L) | 4.65 ± 2.05 | 4.24 (1.49–14.87) | 3.57 ± 1.09 |
3.33 (1.53–6.55) | <0.001 |
| Lymphocyte count (109/L) | 1.54 ± 0.55 | 1.51 (0.20–2.86) | 1.77 ± 0.48 |
1.70 (0.75–2.85) | <0.001 |
| Monocyte count (109/L) | 0.47 ± 0.20 |
0.43 (0.20–1.66) | 0.37 ± 0.12 |
0.36 (0.17–0.74) | <0.001 |
| Platelet count (109/L) | 293.43 ± 79.79 | 279 (106–511) | 224.28 ± 52.19 | 22 (104–364) | <0.001 |
| Mean Platelet Volume (fl) | 9.97 ± 1.01 | 9.90 (7.00–15.70) | 10.67 ± 1.06 | 10.55 (8.30–14.20) | <0.001 |
| NLR | 3.52 ± 2.82 |
2.72 (1.06–25.47) | 2.14 ± 0.81 | 2.01 (0.85–5.32) | <0.001 |
| MLR | 0.36 ± 0.22 |
0.28 (0.12–1.14) | 0.22 ± 0.08 |
0.21 (0.03–0.50) | <0.001 |
| PLR | 236.60 ± 195.11 | 185.01 (108.12–1712.74) | 135.19 ± 46.57 | 123.99 (55.08–290.47) | <0.001 |
| PMR | 29.73 ± 8.68 |
27.96 (10.00–56.09) | 21.36 ± 6.01 | 21.68 (7.70–37.62) | <0.001 |
- CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; MLR, monocyte to lymphocyte ratio; NLR, neutrophil to lymphocyte ratio; PLR, platelet to lymphocyte ratio; PMR, platelet to mean platelet volume ratio; WBC, white blood cell.
ROC Curves Analysis for Various Laboratory Markers
Utilizing ROC curves to analyze the ability of major blood markers and adjunct ratio markers to diagnose PJI (Fig. 2). And calculating the AUC and the specificity, sensitivity, PPV, NPV of Blood markers. The AUC of plasma fibrinogen was 0.853 (95% CI, 0.805–0.901), followed by ESR 0.836 (95% CI, 0.785–0.887) and CRP 0.825 (95% CI, 0.773–0.878), respectively. While the AUCs of adjunct ratio markers were NLR 0.736 (95% CI, 0.674–0.798), MLR 0.733 (95% CI, 0.671–0.796), PLR 0.785 (95% CI, 0.729–0.840) and PMR 0.792 (95% CI, 0.736–0.847), which were more accurate than D-dimer 0.691 (95% CI, 0.624–0.758) and serum WBC 0.622 (95% CI, 0.552–0.692), respectively.
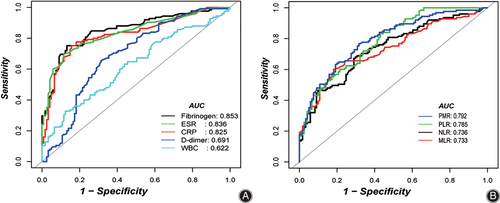
Comparison of Sensitivity and Specificity in PJI Group with AL Group
The plasma fibrinogen optimal threshold (4.13 g/L) demonstrated a sensitivity and specificity of 75.20 and 86.78%, respectively. CRP and ESR had optimal cutoff of 7.34 mg/L (75.19% sensitivity, 84.30% specificity) and 26.0 mm/h. (69.60% sensitivity, 88.43% specificity), respectively. PLR had an optimal threshold of 129.33 (83.20 and 57.02%). The optimal threshold of MLR at 0.26 (60.00% sensitivity, 81.82% specificity) and the optimal threshold of PMR at 23.42 (79.80% sensitivity, 68.33% specificity). The WBC and D-dimer were unable to demonstrate comparable diagnostic efficacy to the adjunct ratio indicators (Table 3).
| Test | AUC (95%CI) | Best threshold | Specificity | Sensitivity | Postive-pv | Negative-pv |
|---|---|---|---|---|---|---|
| Plasma Fibrinogen (g/L) | 0.8531 (0.8051–0.9011) | 4.1300 | 0.8678 | 0.7520 | 0.8545 | 0.7721 |
| CRP (mg/L) | 0.8252 (0.7725–0.8780) | 7.3350 | 0.8430 | 0.7519 | 0.8319 | 0.7669 |
| ESR (mm/h) | 0.8359 (0.7852–0.8865) | 26.00 | 0.8843 | 0.6960 | 0.8614 | 0.7379 |
| D-dimer (μg/mL) | 0.6913 (0.6243–0.7584) | 1.2350 | 0.6860 | 0.6560 | 0.6833 | 0.6587 |
| Serum WBC (109/L) | 0.6219 (0.5521–0.6917) | 7.5500 | 0.8760 | 0.3280 | 0.7321 | 0.5579 |
| NLR | 0.7358 (0.6739–0.7977) | 2.4185 | 0.7107 | 0.6720 | 0.7059 | 0.6772 |
| MLR | 0.7332 (0.6707–0.7957) | 0.2550 | 0.8182 | 0.6000 | 0.7732 | 0.6644 |
| PLR | 0.7846 (0.7292–0.8399) | 129.3250 | 0.5702 | 0.8320 | 0.6667 | 0.7667 |
| PMR | 0.7918 (0.7362–0.8473) | 23.4150 | 0.6833 | 0.7980 | 0.7164 | 0.7387 |
- MLR, monocyte to lymphocyte ratio; NLR, neutrophil to lymphocyte ratio; PLR, platelet to lymphocyte ratio; PMR, platelet to mean platelet volume ratio.
Distribution of Ratio Markers between Bacterial Species
Differences between Gram-positive and Gram-negative bacteria in inflammatory predictive markers were presented in Table 4. This result highlights no significant differences in peripheral blood markers between microorganisms.
| Types | Gram-positive (N = 91) | Gram-negative (N = 9) | P value |
|---|---|---|---|
| PMR | 29.21 ± 8.52 | 27.21 ± 11.39 | 0.227 |
| PLR | 235.09 ± 191.99 | 318.98 ± 320.20 | 0.608 |
| MLR | 0.35 ± 0.19 | 0.47 ± 0.36 | 0.529 |
| NLR | 3.34 ± 1.86 | 6.54 ± 8.03 | 0.468 |
- MLR, monocyte to lymphocyte ratio; NLR, neutrophil to lymphocyte ratio; PLR, platelet to lymphocyte ratio; PMR, platelet to mean platelet volume ratio.
Results of the Prediction Model
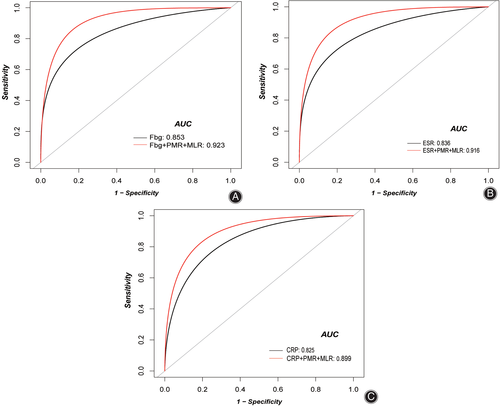
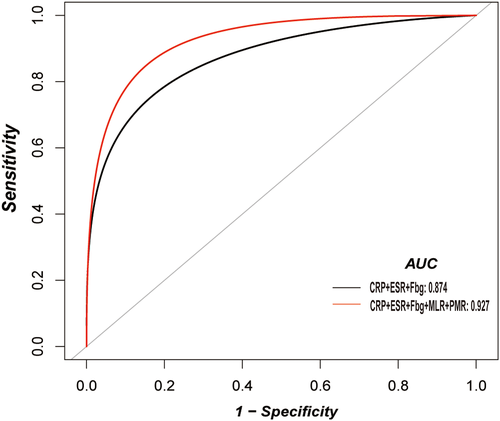
The combination of PMR and MLR was selected as the best ratio indicators combination among all ratio markers based on the prediction model calculation (Table 5, Fig. 3). The result of single main variables combined with both PMR and MLR are as follows, plasma fibrinogen achieved the highest AUC of 0.923 (95% CI, 0.891–0.951), which resulted in a sensitivity, specificity, PPV, and NPV of 0.864, 0.841, 0.850, and 0.856, respectively. Similarly, PMR, MLR combined with ESR and CRP, the AUC raised to 0.91 (95% CI, 0.880–0.946), 0.899 (95% CI, 0.861–0.931), respectively. When multiple variables including all peripheral main markers (plasma fibrinogen, CRP, ESR, D-dimer, serum WBC) and ratio markers (NLR, PLR, MLR, PMR) were placed in the prediction model, the best combination was plasma fibrinogen, ESR, and CRP, PMR, and MLR. The new combination results in good sensitivity, specificity, PPV, and NPV are 0.824, 0.892, 0.888, and 0.823, respectively (Fig. 4). Compared with the use of plasma fibrinogen, CRP, and ESR alone, the combined use of ratio markers shows a good diagnostic value (P < 0.001). A combination of single ratio markers with single main markers shown in Table S1.
| Main markers vs combination with ratio markers | AUC (95%CI) | Specificity | sensitivity | PPV | NPV | P-value |
|---|---|---|---|---|---|---|
| Plasma fibrinogen vs plasma fibrinogen + PMR + MLR | 0.9233 (0.8909–0.9508) | 0.8417 | 0.8640 | 0.8504 | 0.8559 | <0.001 |
| CRP vs CRP + PMR + MLR | 0.8994 (0.8606–0.9307) | 0.8167 | 0.8400 | 0.8268 | 0.8305 | 0.0072 |
| ESR vs ESR+ PMR + MLR | 0.9159 (0.8804–0.9456) | 0.8250 | 0.8640 | 0.8372 | 0.8534 | <0.001 |
| Plasma fibrinogen + ESR + CRP vs plasma fibrinogen + ESR + CRP+ PMR + MLR | 0.9269 (0.8909–0.9547) | 0.8917 | 0.8240 | 0.8879 | 0.8295 | <0.001 |
- AUC, area under the curve.
Discussion
PJI is a devastating complication after TJA. It is estimated that the rate of PJI approximately 1% to 3% of patients who undergo primary TJA, and it will increase the mental and financial burden of patients2, 4, 22, 23. Recent studies indicate that novel tests such as leukocyte esterase (LE), alpha-defensin, and next-generation genome sequencing show very promising diagnostic efficacy, but these tests are expensive, require specialized equipment, and cannot be implemented in all institutions7-9, 24, 25. Also, these tests cannot be used as a single gold standard for the diagnosis of PJI, and according to the 2018 MSIS criteria combination of various clinical examination approaches is still recommended. Therefore, identifying reliable and accurate potential markers for the diagnosis of PJI is the key to the preoperative diagnosis and the development of an appropriate treatment plan. The primary purpose of this study was to determine the diagnostic value of ratio markers and evaluate the performance of the combined diagnosis of PJI with classical inflammatory and coagulation-related markers.
Diagnostic Value of ESR, CRP, and Coagulation-related Markers
The results of the classical inflammation-related markers ESR, CRP, and coagulation-related marker plasma fibrinogen were consistent with previous studies, demonstrating promising diagnostic efficacy (AUCs > 0.8)14. However, the findings of the D-dimer of the current study do not support the previous research that D-dimer outperformed both the ESR and the CRP5, 16. There were two possible explanations, one is D-dimer concentration is different in races, another is the previous study use the plasma as the tested sample, but in our study, we use serum sample as a tested sample, which may result in different levels of D-dimer. In our study, the diagnostic power of the inflammation ratio indicators (AUCs > 0.7) was significantly better than the D-dimer (AUC: 0.691). As we find, one of the factors influencing peripheral blood parameters is bacterial species.
Differences of Ratio Markers Between Bacterial Species
In a previous study, Abe et al.26 demonstrated that blood inflammation markers CRP and IL-6 had significantly higher Gram-negative bacteremia than Gram-positive bacteremia. These findings suggest that differences in host response and virulence mechanisms to different pathogenic microorganisms should be taken into account when using peripheral blood ratio indicators. The findings of Kalbian et al. confirm the prevailing view that Gram-negative PJI is associated with poorer overall results than Gram-positive PJI27. Therefore, determining the diagnostic efficacy of markers is very important, and different bacterial species may influence other indicators. However, our study indicated no significant differences in peripheral blood markers between microorganisms. As a ratio indicator, they may not be significantly affected by Gram-positive versus Gram-negative bacteria according to the present result. Another possible explanation for this might be that delayed infections may be associated with low-virulent organisms, and differences between bacterial species cannot be easily detected28.
The Role of Ratio Markers in Inflammation-related Diseases
The data of ratio indicators can be obtained from the routine blood test, and these exciting data could be analyzed to increase the diagnostic accuracy without additional cost. Our study showed that NLR, MLR, PLR, and PMR in the PJI group were significantly higher than the aseptic loosening group. It could demonstrate the association of the ratio indicators with the state of inflammation and infection in the body. Several studies have indicated that PLR, NLR, MLR, and PMR are associated with inflammatory status in the body. Djordjevic et al. demonstrated that MLR, PLR, and MPV/PC are very effective predictors of the outcome and nature of bacteremia29. Naess et al. reported that NLR and MLR were higher in hospitalized patients with fever due to bacterial infection30. They concluded that both NLR and MLR could be used to diagnose bacterial infections with AUCs of 0.688 and 0.708, respectively. This also accords with our findings, which showed that the AUC for the diagnosis of PJI is 0.736 (95% CI, 0.674–0.797), 0.733 (95% CI, 0.671–0.796), respectively. Yombi et al. demonstrated similar findings in a high level of NLR may association with the inflammatory or infectious problem31.
Ratio Indicators as Promising Biomarkers for the Diagnosis of PJI
Up to now, far too little attention has been paid to utilize MLR in diagnosing PJI. PLR has also been confirmed as the better predictor or diagnostic tool for inflammatory states32-34. The diagnostic value of the PC to MPV ratio in PJI patients was evaluated by Paziuk and coworkers19. They demonstrated that PC to MPV ratio had a high value on diagnosing PJI when combined with ESR and CRP at the optimal threshold 31.7 (AUC: 0.877, sensitivity: 0.802, specificity: 0.821). In contrast, our data showed (Table S1) lower optimal threshold 23.42 but with higher AUC (0.901; 95% CI, 0.876–0.944) and specificity (0.875).
Diagnostic combination illustrates the additional information that can be obtained from routine blood tests to improve diagnostic accuracy further. In a recent study, Tirumala et al. confirmed that a combination of multiple tests for infection biomarkers could be used to diagnose PJI with excellent performance. They reported that PLR and PVR combined with ESR, CRP, synovial WBC, and synovial PMN% increased diagnostic sensitivity and specificity comparable to alpha defensin35. They observed that the ROC analysis showed sensitivities of NLR, MLR, PLR, PMR greater than ESR, and some comparable to CRP. In our study, the diagnostic performance of NLR, MLR, PLR, PMR just only better than D-dimer and serum WBC; the most promising markers still are plasma fibrinogen, ESR, and CRP in our study.
Routine blood tests are paid great attention in our study as the first line and the most important tools to diagnose PJI. One of the reasons is that blood tests can be performed on all patients compared to joint synovial fluids. Moreover, the literature reports that the incidence of “dry tap” ranges up to 46%, especially in the hip, and accurate information obtained from blood tests is crucial in this group of patients36. In the present study, we selected more inflammation-related markers, including CRP, ESR, Plasma fibrinogen, D-dimer, serum WBC. Furthermore, a predictive model is performed to select the optimal combination. In contrast to previous studies, in our study, according to the prediction model, not a single ratio indicator was chosen but MLR and PMR as the optimal combination. The combination of CRP, ESR, plasma fibrinogen with MLR and PMR greatly improved the diagnostic value. Among them, plasma fibrinogen combined with MLR and PMR achieved the highest diagnostic efficacy (sensitivity: 0.842, specificity:0.864, PPV: 0.851, and NPV: 0.856). And ESR, CRP had improved the accuracy when combined with MLR and PMR. Besides, we tested the best combinations in all variables. Finally, the three main indicators CRP, ESR, and plasma fibrinogen with MLR and PMR combinations, showed the highest specificity and PPV of 0.892 and 0.888, respectively.
Limitations
There are some limitations to this study. First, this was a retrospective study, and was inherently subject to selection bias. Electronic medical records may contain incorrect or non-existent information for individual patients. Second, Peripheral blood ratio markers are influenced by factors other than bacterial species, as well as medication use, age, and some unnoticed comorbidities. Third, this was a single-center study. The discrepancy between the results of our research and the same type of study may be related to races. Finally, the effect of bacterial species on the ratio indicator may not be detected because of the small sample size. Therefore, a large sample size, cross-national multicenter studies are needed.
Conclusions
In conclusion, our study confirms that ratio markers (MLR and PMR), when used in combination with fibrinogen, achieve better diagnostic performance, especially for patients with “dry tap” can benefit from it. Routine serologic markers more accurately diagnose potential infections through a new combination of models. Blood tests are easy to obtain, will not increase financial burden, and provide surgeons with the possibility of obtaining more accurate information from a single test.
Acknowledgements
We would like to thank all staff from the participating departments.




