A Comprehensive Review of 148 Cases of Major Salivary Gland Tumours: Critical Insights Into Metastatic Patterns, Prognostic Factors, and Treatment Outcomes
Funding: The author received no specific funding for this work.
ABSTRACT
Aim
To analyse the clinicopathological characteristics of cases of major salivary gland tumours associated with distant metastasis.
Materials and Methods
A relevant search of English literature was conducted in PubMed, SpringerLink, ScienceDirect, Scopus, and Google Scholar for distant metastasis from major salivary gland tumours.
Results
This retrospective study included 148 reported cases. Among them, 79 patients were male and 69 were female. The mean age of the patients was 53 ± 14. The parotid gland was the most frequently metastatic salivary gland, and various bones were the most common metastatic sites, followed by the lungs. Adenoid cystic carcinoma was the most common histological tumour type. The time interval between the development of a primary tumour and the diagnosis of the metastatic lesion ranged from 2 to 600 months. In most patients, the secondary lesion was diagnosed in less than 127 months. In 103 cases, the patient was alive at the time of reporting.
Conclusion
Adenoid cystic carcinoma and metastasising pleomorphic adenoma are highly aggressive major salivary gland tumours characterised by rapid growth and distant metastasis. Although distant metastasis from major salivary gland tumours is not common, it signifies a poor prognosis, with death occurring within months of detection. Therefore, greater attention should be paid to major salivary gland tumours.
1 Introduction
Major salivary gland tumours constitute 6% of all malignant tumours in the head and neck region and 0.3% of all malignancies [1]. They exhibit a wide spectrum of clinical, histological, and biological features and have a varied rate of local, regional, and distant metastases [2, 3]. The prevalence has been estimated to be between 8.7% and 50%, depending on histological types and tumour sites [4].
Metastasis is an important biological behaviour of salivary gland tumours that complicates treatment and is associated with poor prognosis [3, 5]. The lungs, bones, brain, and liver are the most common metastatic sites [3]. Undifferentiated carcinoma, followed by adenocarcinoma, is the most common tumours with distant metastasis (DM) [6]. A previous study has indicated that distant metastasis is more frequent in tumours arising in the submandibular gland than in those arising in the parotid gland [7]. Salivary gland tumours comprise a heterogeneous histological group with variable biological behaviour. Metastatic lesions are the main cause of cancer-related deaths in humans [3].
The identification of clinicopathological characteristics of salivary gland tumours associated with DM is crucial for therapeutic planning. The aim of this retrospective study was to analyse the clinicopathological characteristics of cases of major salivary gland tumours linked to distant metastasis.
2 Materials & Methods
2.1 Searching Strategy
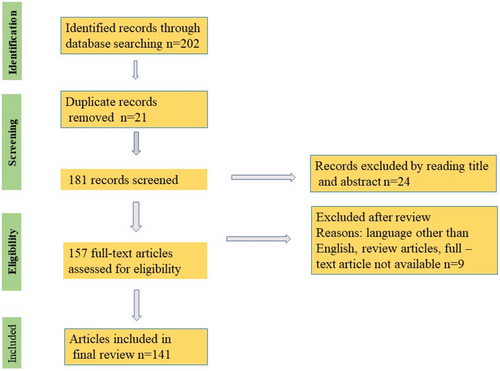
A relevant search of English literature was conducted in PubMed, SpringerLink, ScienceDirect, Scopus, and Google Scholar. The keywords: “major salivary glands”, and “distant metastasis” were searched in the title/abstract of publications, limited to the years 1970–2024. Only related case reports were included. Figure 1 illustrates the flow of the number of articles identified, included, and excluded at different stages.
All variables such as age, gender, primary and secondary tumour sites, histological type of tumour, time interval between detection of the primary tumour and diagnosis of metastasis, and survival status were analysed using the Chi-square test and Fisher's exact test.
2.2 Quality Assessment & Data Analysis
For a more comprehensive understanding, all data were categorised into two groups: lesions in males and lesions in females. To perform statistical analysis, metastatic sites with ≤ 6 cases were combined into the miscellaneous group. In addition, histologic types with ≤ 6 cases were grouped as the miscellaneous group. All bones as metastatic sites were classified as one group: various bones.
3 Results
This retrospective study included 148 reported cases. Among them, 79 patients were male and 69 were female. The mean age of the patients was 53 ± 14 (ranging from 10 to 91 years). The parotid gland was the most frequently metastatic salivary gland (n = 105; 70%), and various bones were the most common metastatic sites (n = 31; 20%), followed by the lungs (n = 25; 16%). Adenoid cystic carcinoma (AdCC) was the most common histological tumour type (n = 40; 27%), followed by metastasizing pleomorphic adenoma (MPA) (n = 31; 20%). Interestingly, all histological types were more frequent with distant metastases from the parotid gland except for AdCC, which was more frequent with distant metastases from the submandibular glands (n = 18 vs. n = 19). The time interval between the development of a primary tumour and the diagnosis of the metastatic lesion ranged from 2 to 600 months, with a mean of 127 months. In most patients, the secondary lesion was diagnosed in less than 127 months (n = 84). In 103 cases, the patient was alive at the time of reporting.
Regarding the demographic data for males, the age ranged from 22 to 91 years, with a mean age of 54 ± 13. Additionally, the parotid gland was the most common primary site, with 58 cases, while the sublingual gland was the least frequent primary site, with 4 cases. The most frequent metastatic sites were various bones (17 cases), followed by the lungs (14 cases). The kidney was the least common metastatic site (1 case). Adenoid cystic carcinoma was the most common metastatic histologic type (n = 18), while acinic cell carcinoma was the least metastatic tumour type (n = 3). In most patients (n = 51; 34.46%), metastatic disease was found in less than 127 months. The number of patients who were alive at the time of reporting was 54.
Considering the demographic details of females, the mean age was 52 ± 15 years (ranging from 10 to 83). Additionally, the parotid gland was the most common primary site (n = 47; 31.8%), while the sublingual gland was the least common primary gland (n = 1). Various bones were the most common metastatic sites (n = 14; 9.5%). The lymph nodes were the least common metastatic site (n = 1). The most common histologic type was AdCC (n = 22; 14.9%). In 33 cases (22.3%), the time interval between the development of a malignancy and the diagnosis of the metastatic tumour was less than 127 months, and 49 patients were alive at the time of reporting.
All details are provided in Tables 1 and 2.
| Primary site (type of gland) | Metastatic site | Age range (years) | Histological type | The time interval from the detection of the primary tumour to the diagnosis of metastasis | Survival status after diagnosis till the report of case | References |
|---|---|---|---|---|---|---|
| Parotid | Lung | 26 | AdCC | 10 years | Alive | [8] |
| Parotid | Lung, bones, muscles, skin | 40 | AdCC | 15 years | Died after 2 months | [9] |
| Parotid | Eyes | 52 | AdCC | Same time | Alive | [10] |
| Parotid | Eye | 64 | AdCC | 5 years | Alive | [11] |
| Parotid | Brain | 60 | AdCC | 10 years | Died after 8 months | [12] |
| Parotid | Brain | 62 | AdCC | 12 years | Alive | [13] |
| Parotid | Brain | 52 | AdCC | 27 years | Alive | [14] |
| Parotid | Skin | 39 | AdCC | 8 years | Alive | [15] |
| Parotid | Splenium, corpus callosum | 43 | AdCC | 5 years | Alive | [16] |
| Parotid | Lung | 58 | MPA | 34 years | Alive | [17] |
| Parotid | Lung | 55 | MPA | 39 years | Alive | [18] |
| Parotid | Lung, liver | 57 | MPA | 7 years | Alive | [19] |
| Parotid | Skin | 31 | MPA | 8 years | Alive | [20] |
| Parotid | Skin | 56 | MPA | 8 years | Alive | [21] |
| Parotid | Supraclavicular LN | 61 | MPA | 28 years | Alive | [22] |
| Parotid | Back of the neck | 36 | MPA | 18 years | Alive | [23] |
| Parotid | Maxillary gingiva, bone | 36 | MPA | 21 years | Alive | [24] |
| Parotid | Maxillary sinus | 32 | MPA | 12 years | Alive | [25] |
| Parotid | Spine | 65 | MPA | 7 years | Alive | [26] |
| Parotid | Calvaria | 33 | MPA | 16 years | Alive | [27] |
| Parotid | Lung, spleen | 66 | CaXPA | 3 years | Alive | [28] |
| Parotid | Eyes | 34 | CaXPA | 1 year | Alive | [29] |
| Parotid | Eye | 65 | CaXPA | 6 months | Died after 2 years | [30] |
| Parotid | Brain | 36 | CaXPA | 19 months | Died after 2 months | [31] |
| Parotid | Abdomen | 72 | CaXPA | 15 months | Died after 3 months | [32] |
| Parotid | Liver | 55 | CaXPA | Same time | Died after 3 months | [33] |
| Parotid | Colon | 78 | CaXPA | Same time | Alive | [34] |
| Parotid | Skin | 40 | SDC | 18 months | Alive | [35] |
| Parotid | Skin | 71 | SDC | 2 years | Alive | [36] |
| Parotid | Skin | 69 | SDC | 2 months | Alive | [36] |
| Parotid | Lung | 65 | SDC | 12 years | Alive | [37] |
| Parotid | Stomach | 67 | SDC | 1 year | Died after 8 months | [38] |
| Parotid | Mandibular gingiva | 67 | SDC | 11 months | Died after 1 month | [39] |
| Parotid | Spine | 44 | SDC | 3 years | Died after 7 months | [40] |
| Parotid | Eye | 43 | SDC | 6 years | Alive | [41] |
| Parotid | Eye | 56 | SDC | Same time | Alive | [42] |
| Parotid | Bones, liver, CLN | 68 | SDC | Same time | Alive | [43] |
| Parotid | Brain | 61 | SDC | 4 years | Alive | [44] |
| Parotid | Bulbar conjunctiva | 65 | MEC | 10 months | Alive | [45] |
| Parotid | Cerebellopontine | 72 | MEC | 4 years | Died after 9 months | [46] |
| Parotid | Colon | 59 | MEC | 10 years | Alive | [47] |
| Parotid | Eyes | 45 | NOS | 1 year | Alive | [48] |
| Parotid | Eye | 91 | NOS | 2 years | Died after 5 months | [49] |
| Parotid | Endobronchial | 43 | NOS | 9 months | Alive | [50] |
| Parotid | Lung | 64 | MyCa | Several months | Alive | [51] |
| Parotid | Kidney | 56 | MyCa | 22 months | Alive | [52] |
| Parotid | Cavernous sinus | 46 | MyCa | 3 years | Alive | [53] |
| Parotid | Iliac crest | No data | ACC | 3 years | Alive | [54] |
| Parotid | Vertebra | 40 | ACC | 4 months | Alive | [55] |
| Parotid | Skull | 53 | ACC | 7 years | Alive | [56] |
| Parotid | CLN | 74 | CyAd | 1 year | Alive | [57] |
| Parotid | Intra-parotid LN | 47 | CyAd | 2 years | Alive | [57] |
| Parotid | Lung, brain | 32 | BCA | 5 years | Alive | [58] |
| Parotid | Hand | 67 | BCA | 2 years | Alive | [59] |
| Parotid | Lung | 63 | EMC | 14 years | Alive | [60] |
| Parotid | CLN | 47 | CaS | Same time | Died after a few months | [61] |
| Parotid | Cerebellopontine Angle | 61 | OC | 6 months | Died after 1 year | [62] |
| Submandibular | Liver | 55 | AdCC | 1 year | Died after 3 years | [63] |
| Submandibular | Liver | 76 | AdCC | 5 years | Alive | [64] |
| Submandibular | Spine | 45 | AdCC | 11 years | Alive | [65] |
| Submandibular | Spine | 62 | AdCC | 7 years | Died after a few months | [66] |
| Submandibular | Lung | 53 | AdCC | 5 years | Alive | [8] |
| Submandibular | Great toes | 52 | AdCC | 12 years | Alive | [67] |
| Submandibular | Sternum | 52 | AdCC | 10 years | Alive | [68] |
| Submandibular | Lungs | 49 | MPA | 11 years | Alive | [69] |
| Submandibular | Pelvis | 59 | MPA | 44 years | Alive | [70] |
| Submandibular | Spine | 35 | CaXPA | Same time | Died after a few months | [71] |
| Submandibular | Kidney | 63 | CaXPA | 30 years | Alive | [72] |
| Submandibular | Vertebra | 67 | OC | 30 years | Alive | [73] |
| Submandibular | CLN | 47 | OC | Same time | Alive | [74] |
| Submandibular | Lung | 51 | EMC | 3 years | Died after 30 months | [75] |
| Submandibular | Choroid plexus | 46 | NOS | 5 months | Alive | [76] |
| Submandibular | CLN | 69 | CyAd | 7 months | Alive | [57] |
| Submandibular | Skin | 22 | MyCa | No data | Alive | [77] |
| Submandibular | Spine | 50 | BCA | 5 years | Alive | [78] |
| Sublingual | Lung | 52 | AdCC | 20 years | Died after 2 years | [79] |
| Sublingual | Liver | 70 | AdCC | 3 years | Alive | [80] |
| Sublingual | Brain | 64 | CaXPA | 11 months | Died after 6 months | [81] |
| Sublingual | Pituitary gland | 52 | NOS | 6 years | Alive | [82] |
- Abbreviations: ACC, acinic cell carcinoma; AdCC, adenoid cystic carcinoma; BCA, basal cell adenocarcinoma; CaS, carcinosarcoma; CaXPA, carcinoma ex pleomorphic adenoma; CLN, cervical lymph node; CyAd, cystadenocarcinoma; EMC, epithelial- myoepithelial carcinoma; LN, lymph node; MEC, mucoepidermoid carcinoma; MPA, metastasizing pleomorphic adenoma; MyCa, myoepithelial carcinoma; NOS, not otherwise specified; OC, oncocytic carcinoma; SDC, salivary duct carcinoma.
| Primary site (type of gland) | Metastatic site | Age range (years) | Histological type | The time interval from the detection of the primary tumour to the diagnosis of metastasis | Survival status after diagnosis till the report of case | References |
|---|---|---|---|---|---|---|
| Parotid | Lung | 45 | MPA | 17 years | Alive | [21] |
| Parotid | Lungs | 33 | MPA | 23 years | Alive | [83] |
| Parotid | Lungs | 40 | MPA | 12 years | Alive | [84] |
| Parotid | Lung | 54 | MPA | 3 years | Died after 5 years | [85] |
| Parotid | Kidney | 40 | MPA | 16.9 years | Alive | [86] |
| Parotid | Kidney | 68 | MPA | 28 years | Alive | [87] |
| Parotid | Kidney | 49 | MPA | 29 years | Alive | [88] |
| Parotid | Kidney | 62 | MPA | 13 years | Alive | [89] |
| Parotid | Liver | 65 | MPA | 20 years | Alive | [90] |
| Parotid | Liver | 28 | MPA | 11 years | Alive | [91] |
| Parotid | Mediastinal ln | 43 | MPA | 27 years | Alive | [92] |
| Parotid | Cervical area | 36 | MPA | 15 years | Alive | [93] |
| Parotid | Brain | 10 | MPA | 3 years | Alive | [94] |
| Parotid | Sacrum | 75 | MPA | 25 years | Alive | [95] |
| Parotid | Supraspinatus muscle | 65 | MPA | 24 years | Died after 5 months | [96] |
| Parotid | Liver | 60 | AdCC | 3 years | Died after 2 years | [97] |
| Parotid | Liver | 30 | AdCC | 10 years | Alive | [98] |
| Parotid | Kidney | 21 | AdCC | 7 years | Alive | [99] |
| Parotid | Kidney | 40 | AdCC | 5 years | Died after 10 years | [100] |
| Parotid | Skin | 63 | AdCC | 4 years | Died after 2 months | [101] |
| Parotid | Intrasellar area | 78 | AdCC | 4 years | Alive | [102] |
| Parotid | Brain | 43 | AdCC | 15 years | Alive | [103] |
| Parotid | Spine | 71 | AdCC | 37 years | Alive | [104] |
| Parotid | Pituitary gland | 72 | AdCC | 26 years | Alive | [105] |
| Parotid | Lung | 53 | ACC | 2 years | Died after 6 months | [106] |
| Parotid | Lung | 65 | ACC | No data | Died after 2 years | [107] |
| Parotid | Pancreas | 46 | ACC | 7 years | Alive | [108] |
| Parotid | Eye | 54 | ACC | Same time | Alive | [109] |
| Parotid | Skin | 59 | ACC | 20 years | Alive | [110] |
| Parotid | Vertebra | 72 | ACC | 6 years | Alive | [111] |
| Parotid | Spine | 71 | ACC | 15 months | Died after 8 months | [112] |
| Parotid | Ilium | 78 | ACC | 1 year | Alive | [113] |
| Parotid | Mandible | 41 | CaXPA | Same time | Alive | [114] |
| Parotid | Brain | 66 | CaXPA | 40 years | Died after 18 months | [115] |
| Parotid | Kidney | 32 | CaXPA | 3 years | Died after 2 years | [116] |
| Parotid | Lung | 80 | SDC | Same time | Died after 11 months | [117] |
| Parotid | Uterus | 61 | SDC | 3 years | Alive | [118] |
| Parotid | Brain | 52 | PDC | 1 year | Alive | [119] |
| Parotid | Pelvic, femur | 19 | PDC | 8 months | Alive | [120] |
| Parotid | Spine | 41 | EMC | 1 year | Alive | [121] |
| Parotid | Vertebra | 65 | EMC | 18 months | Alive | [122] |
| Parotid | Skull | 55 | MEC | 6 years | Alive | [123] |
| Parotid | Ovaries, peritoneum | 28 | MEC | 11 years | Died after 14 months | [124] |
| Parotid | Lung | 52 | NOS | Same time | Died after 15 months | [125] |
| Parotid | Skin | 83 | NOS | 50 years | Died after 1 month | [126] |
| Parotid | Scalp | 58 | BCA | 2 years | Alive | [127] |
| Submandibular | Eyes | 45 | AdCC | 11 years | Died after 5 weeks | [128] |
| Submandibular | Eyes | 56 | AdCC | 2 years | Died after 6 weeks | [129] |
| Submandibular | Eyes | 51 | AdCC | 2 years | Alive | [130] |
| Submandibular | Eye | 50 | AdCC | 5 years | Died after 4 months | [131] |
| Submandibular | Liver | 51 | AdCC | 2 years | Alive | [132] |
| Submandibular | Liver | 52 | AdCC | 30 years | Alive | [133] |
| Submandibular | Ovary | 30 | AdCC | 10 years | Alive | [134] |
| Submandibular | Lung, choroid | 43 | AdCC | 5 years | Alive | [135] |
| Submandibular | Larynx | 46 | AdCC | 9 years | Alive | [136] |
| Submandibular | Spine | 54 | AdCC | 17 years | Alive | [137] |
| Submandibular | Breast | 67 | AdCC | 5 years | Died after a few months | [138] |
| Submandibular | Toe | 62 | AdCC | 8 years | Alive | [139] |
| Submandibular | Skin | 57 | MPA | 3 months | Alive | [140] |
| Submandibular | Vertebra | 35 | MPA | 11 years | Alive | [21] |
| Submandibular | Lung, sternum | 40 | MPA | 7 years | Alive | [141] |
| Submandibular | Breast | 64 | SDC | 3 years | Alive | [142] |
| Submandibular | Bone marrow | 33 | PDC | 3 years | Alive | [143] |
| Submandibular | Vertebra, lung | 39 | PDC | 4 months | Alive | [144] |
| Submandibular | Brain, vertebra | 60 | NOS | 41 months | Alive | [119] |
| Submandibular | Skin | 68 | MyCa | 5 years | Died after 1 year | [145] |
| Submandibular | Eyes | 52 | MEC | 6 years | Died after 5 months | [146] |
| Sublingual | Lung | 66 | AdCC | No data | Alive | [147] |
- Abbreviations: ACC, acinic cell carcinoma; AdCC, adenoid cystic carcinoma; BCA, basal cell adenocarcinoma; CaXPA, carcinoma ex pleomorphic adenoma; EMC, epithelial- myoepithelial carcinoma; LN, lymph node; MEC, mucoepidermoid carcinoma; MPA, metastasizing pleomorphic adenoma; MyCa, myoepithelial carcinoma; NOS, not otherwise specified; PDC, poorly differentiated carcinoma; SDC, salivary duct carcinoma.
Table 3 summarises statistically significant results based on Chi-square and Fisher's exact tests.
4 Discussion
Distant metastasis is a complex process and a late event in tumour progression. It results from the seeding of circulating tumour cells in certain organs. According to Paget' theory, the distribution of metastatic cells in specific organs is not random, leading to the proposing of the seed and soil theory [148].
Due to the rarity of salivary gland tumours, knowledge about the progression of these tumours is limited [149]. In the present study, similar to a prior study, DM was predominantly found in males (64% vs. 53% in females) [4]. This finding may suggest that men present with more advanced stages of tumours at the time of diagnosis.
In the current analysis, the mean age of the patients was 53 ± 14; however, in a prior study, the mean age of the patients was 61 years (range, 15–88) [4]. Furthermore, it has been established that DM is more common in elderly cancer patients (65 years and older) [150]; nonetheless, in the current series, only 29 patients were older than 65 years (19.5%). Notably, 32 patients (21.6%) were 40 years old or younger. A previous investigation showed that DM is not correlated with gender and age but is related to the tumour site [9]. However, the current study demonstrated a relationship between gender and age with other studied variables (see Table 3).
In the present series, the parotid was the most common salivary gland with DM (70.9%), but a previously published work found the submandibular gland to be the most prevalent salivary gland metastasising to other organs (42%). The metastatic route of parotid tumours is unclear, but it is suggested that the maxillary artery, which travels through the parotid gland, may serve as a vascular spread route [114]. A prior study on 103 cases of parotid tumours found DM in 24% of cases, primarily in the lungs (68%), followed by the bones (24%) [15]. However, the current series indicated metastases to the bones and lungs in 20.9% and 16.9% of cases, respectively. It is generally accepted that the lungs and bones are the two most common sites for distant metastasis [16]. A very recent systematic review found 19 cases of spinal metastasis with a mean age of 54 years. The most common histopathological subtypes were ACC, followed by AdCC [151]. The current study identified 10 cases of spinal metastasis with a mean age of 53.6 (range, 35–71). The most common salivary gland tumour with spinal metastasis was AdCC with 4 cases. Spinal metastasis from ACC was reported in one case.
Metastasis is not a random process; before the spread of cancer cells, a premetastatic niche, a supportive environment, must be established. For example, VEGF receptor 1 (VEGFR1)-positive BM-derived haematopoietic progenitor cells accumulate in the premetastatic tissue before the arrival of cancer cells [152].
Rarely, head and neck cancer spreads via blood vessels. Therefore, cervical lymph node metastasis is expected to be the most common event [2]; nevertheless, the present case series found that metastasis to the cervical lymph nodes occurred in 3.4% of patients. A prior systematic analysis on cervical lymph node metastases from AdCC identified only 4 studies showing cervical lymph node metastasis in 17% of patients. Additionally, this systematic review found that AdCC from minor salivary glands has a higher rate of cervical lymph node metastasis. The authors concluded that elective neck dissection is not necessary for patients with major salivary gland AdCC [153].
In this investigation, various bones were the most frequent metastatic sites (21%), followed by the lungs (16.9%). These findings are not consistent with a previous study that showed the lungs as the most prevalent metastatic sites, followed by the bones [154].
In the current analysis, the most common histotype with DM was AdCC with 40 cases (27%), followed by MPA with 31 cases (20.1%). Additionally, AdCC was the most common histological tumour type metastasising to various tissues in both genders. The incidence of DM from AdCC varies between 5% and 54.9%, and the lungs, bones, liver, and brain are the most common sites for metastases. AdCC accounts for approximately 10% of salivary gland neoplasms and affects both the parotid and submandibular glands [155]. In this review, AdCCs metastasised mainly from submandibular glands, not the parotids (47% vs. 45%). It has been suggested that submandibular AdCCs have a greater ability to induce tumour angiogenesis [156]. Furthermore, it has been documented that the myoepithelial cells in submandibular AdCC have a higher rate of proliferation and are less differentiated than those in the parotid AdCC. These findings may explain the increased aggression of the submandibular AdCC [157]. Notably, AdCC has the ability to invade adjacent structures as well as to demonstrate DM. In addition, a unique characteristic of AdCC that differentiates it from other salivary tumours is perineural invasion [157].
In the present analysis, there were 31 cases (21%) of DM from MPA with 18 cases in females (12.1%). Among these, 26 cases (17.6%) were from parotid tumours. Moreover, in 9 cases (6%) DM from MPA occurred in the lungs, and in 6 cases (4%), it occurred in various bones. There are several reports of locally aggressive pleomorphic adenomas that metastasised to regional lymph nodes and exhibited DM, despite their benign histologic appearance. PA may undergo malignant transformation in 2% to 9% of cases, whether a long-standing primary tumour or a recurrent tumour. It is suggested that the proliferation of myoepithelial cells may alter the tumour's nature [20]. It is unclear how a benign tumour such as PA metastasises to other organs. Perhaps the most accepted hypothesis is the accumulation of key genetic alterations that cause histological and biological changes. For example, the cumulative loss of chromosomal loci at 3p, 9p, and 17p has been observed in MPAs [85]. Additionally, it has been proposed that prior radiation of the primary tumour or surgical manipulation allows tumour cells to enter blood vessels [141]. These findings suggest that cases histologically diagnosed as AdCC or MPA are the most significant candidates for further follow-up.
5 Conclusion
Adenoid cystic carcinoma and metastasising pleomorphic adenoma are highly aggressive major salivary gland tumours characterised by rapid growth and distant metastasis. Although distant metastasis from major salivary gland tumours is uncommon, it signifies a poor prognosis, with death occurring within months of detection. Therefore, greater attention should be paid to major salivary gland tumours. Understanding the clinical history and histopathologic characteristics of salivary metastatic tumours is critical for achieving an accurate diagnosis, which is essential for appropriate patient management.
Acknowledgements
The author would like to thank Hamadan University of Medical Sciences for continued support. Open access publishing facilitated by Griffith University, as part of the Wiley - Griffith University agreement via the Council of Australian University Librarians.
Conflicts of Interest
The author declares no conflicts of interest.
Open Research
Data Availability Statement
The author has nothing to report.