Primary central nervous system lymphomas with massive intratumoral hemorrhage: Clinical, radiological, pathological, and molecular features of six cases
Corresponding Author
Seiji Yamada
Department of Diagnostic Pathology, Fujita Health University School of Medicine, Toyoake, Japan
Correspondence: Seiji Yamada, MD, PhD, Department of Diagnostic Pathology, Fujita Health University School of Medicine 1-98 Dengakugakubo, Kutsukake-cho, Toyoake, Aichi 470-1192, Japan. Email: [email protected]
Search for more papers by this authorJun Muto
Department of Neurosurgery, Fujita Health University School of Medicine, Toyoake, Japan
Search for more papers by this authorSachiko Iba
Department of Hematology, Fujita Health University School of Medicine, Toyoake, Japan
Search for more papers by this authorKazuya Shiogama
Division of Morphology and Cell Function, Faculty of Medical Technology, Fujita Health University School of Health Sciences, Toyoake, Japan
Search for more papers by this authorYuta Tsuyuki
Department of Pathology and Laboratory Medicine, Nagoya University Hospital, Nagoya, Japan
Search for more papers by this authorAkira Satou
Department of Surgical Pathology, Aichi Medical University Hospital, Nagakute, Japan
Search for more papers by this authorShigeo Ohba
Department of Neurosurgery, Fujita Health University School of Medicine, Toyoake, Japan
Search for more papers by this authorKazuhiro Murayama
Joint Research Laboratory of Advanced Medical Imaging, Fujita Health University School of Medicine, Toyoake, Japan
Search for more papers by this authorYasuo Sugita
Department of Neuropathology, St. Mary's Hospital, Kurume, Japan
Search for more papers by this authorShigeo Nakamura
Department of Pathology and Laboratory Medicine, Nagoya University Hospital, Nagoya, Japan
Search for more papers by this authorHideaki Yokoo
Department of Human Pathology, Gunma University Graduate School of Medicine, Maebashi, Japan
Search for more papers by this authorAkihiro Tomita
Department of Hematology, Fujita Health University School of Medicine, Toyoake, Japan
Search for more papers by this authorYuichi Hirose
Department of Neurosurgery, Fujita Health University School of Medicine, Toyoake, Japan
Search for more papers by this authorTetsuya Tsukamoto
Department of Diagnostic Pathology, Fujita Health University School of Medicine, Toyoake, Japan
Search for more papers by this authorMasato Abe
Department of Pathology, School of Health Sciences, Fujita Health University, Toyoake, Japan
Search for more papers by this authorCorresponding Author
Seiji Yamada
Department of Diagnostic Pathology, Fujita Health University School of Medicine, Toyoake, Japan
Correspondence: Seiji Yamada, MD, PhD, Department of Diagnostic Pathology, Fujita Health University School of Medicine 1-98 Dengakugakubo, Kutsukake-cho, Toyoake, Aichi 470-1192, Japan. Email: [email protected]
Search for more papers by this authorJun Muto
Department of Neurosurgery, Fujita Health University School of Medicine, Toyoake, Japan
Search for more papers by this authorSachiko Iba
Department of Hematology, Fujita Health University School of Medicine, Toyoake, Japan
Search for more papers by this authorKazuya Shiogama
Division of Morphology and Cell Function, Faculty of Medical Technology, Fujita Health University School of Health Sciences, Toyoake, Japan
Search for more papers by this authorYuta Tsuyuki
Department of Pathology and Laboratory Medicine, Nagoya University Hospital, Nagoya, Japan
Search for more papers by this authorAkira Satou
Department of Surgical Pathology, Aichi Medical University Hospital, Nagakute, Japan
Search for more papers by this authorShigeo Ohba
Department of Neurosurgery, Fujita Health University School of Medicine, Toyoake, Japan
Search for more papers by this authorKazuhiro Murayama
Joint Research Laboratory of Advanced Medical Imaging, Fujita Health University School of Medicine, Toyoake, Japan
Search for more papers by this authorYasuo Sugita
Department of Neuropathology, St. Mary's Hospital, Kurume, Japan
Search for more papers by this authorShigeo Nakamura
Department of Pathology and Laboratory Medicine, Nagoya University Hospital, Nagoya, Japan
Search for more papers by this authorHideaki Yokoo
Department of Human Pathology, Gunma University Graduate School of Medicine, Maebashi, Japan
Search for more papers by this authorAkihiro Tomita
Department of Hematology, Fujita Health University School of Medicine, Toyoake, Japan
Search for more papers by this authorYuichi Hirose
Department of Neurosurgery, Fujita Health University School of Medicine, Toyoake, Japan
Search for more papers by this authorTetsuya Tsukamoto
Department of Diagnostic Pathology, Fujita Health University School of Medicine, Toyoake, Japan
Search for more papers by this authorMasato Abe
Department of Pathology, School of Health Sciences, Fujita Health University, Toyoake, Japan
Search for more papers by this authorAbstract
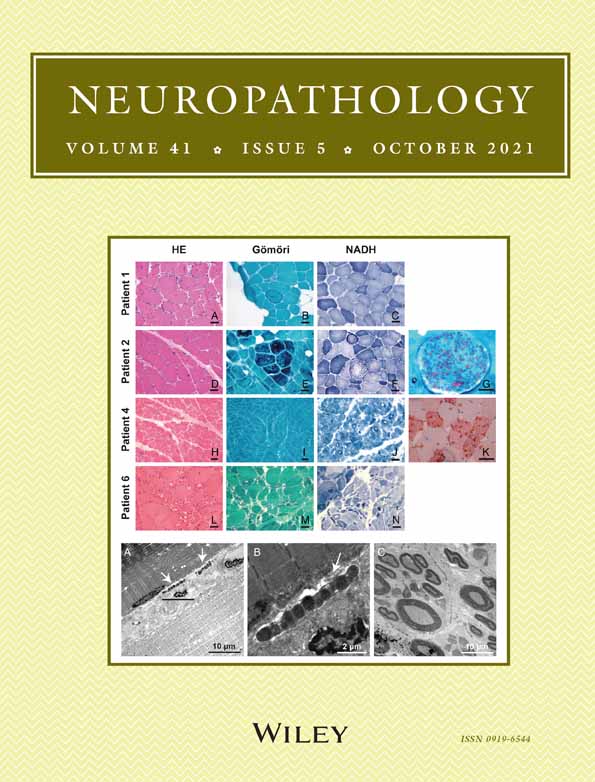
Primary central nervous system lymphomas (PCNSLs) rarely exhibit intratumoral hemorrhage. The differential diagnosis of hemorrhagic neoplasms of the central nervous system (CNS) currently includes metastatic carcinomas, melanomas, choriocarcinomas, oligodendrogliomas, and glioblastomas. Here we present the clinical, radiological, pathological, and molecular genetic features of six cases of PCNSL associated with intratumoral hemorrhage. The median age of patients was 75 years, with male predominance. While conventional PCNSLs were associated with low cerebral blood volume (CBV), perfusion magnetic resonance imaging (MRI) revealed elevated CBV in three cases, consistent with vascular proliferation. All six cases were diagnosed pathologically as having diffuse large B-cell lymphoma (DLBCL) with a non-germinal center B-cell-like (non-GCB) phenotype; marked histiocytic infiltrates and abundant non-neoplastic T-cells were observed in most cases. Expression of vascular endothelial growth factor and CD105 in the lymphoma cells and the small vessels, respectively, suggested angiogenesis within the neoplasms. Neoplastic cells were immunohistochemically negative for programmed cell death ligand 1 (PD-L1), while immune cells in the microenvironment were positive for PD-L1. Mutations in the MYD88 gene (MYD88) (L265P) and the CD79B gene (CD79B) were detected in five and one case, respectively. As therapeutic modalities used for PCNSLs differ from those that target conventional hemorrhagic neoplasms, full tissue diagnoses of all hemorrhagic CNS tumors are clearly warranted.
REFERENCES
- 1 DN Louis, H Ohgaki, OD Wiestler, WK Cavenee, (eds). WHO Classification of Tumours of the Central Nervous System. Lyon: International Agency for Research on Cancer, 2016.
- 2 SH Swerdlow, E Campo, NL Harris et al., (eds). WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon: International Agency for Research on Cancer, 2017.
- 3Ball MK, Morris JM, Wood AJ, Meyer FB, Kaszuba MC, Raghunathan A. Ventricle-predominant primary CNS lymphomas: Clinical, radiological and pathological evaluation of five cases and review of the literature. Brain Tumor Pathol 2020; 37: 22–30.
- 4Schlegel U. Primary CNS lymphoma. Ther Adv Neurol Disord 2009; 2: 93–104.
- 5Jenkins CN, Colquhoun IR. Characterization of primary intracranial lymphoma by computed tomography: An analysis of 36 cases and a review of the literature with particular reference to calcification haemorrhage and cyst formation. Clin Radiol 1998; 53: 428–434.
- 6Coulon A, Lafitte F, Hoang-Xuan K et al. Radiographic findings in 37 cases of primary CNS lymphoma in immunocompetent patients. Eur Radiol 2002; 12: 329–340.
- 7Haldorsen IS, Kråkenes J, Krossnes BK, Mella O, Espeland A. CT and MR imaging features of primary central nervous system lymphoma in Norway, 1989-2003. Am J Neuroradiol 2009; 30: 744–751.
- 8Haldorsen IS, Espeland A, Larsson EM. Central nervous system lymphoma: Characteristic findings on traditional and advanced imaging. Am J Neuroradiol 2011; 32: 984–992.
- 9Fukui MB, Livstone BJ, Meltzer CC, Hamilton RL. Hemorrhagic presentation of untreated primary CNS lymphoma in a patient with AIDS. AJR Am J Roentgenol 1998; 170: 1114–1115.
- 10Kim IY, Jung S, Jung TY, Kang SS, Choi C. Primary central nervous system lymphoma presenting as an acute massive intracerebral hemorrhage: Case report with immunohistochemical study. Surg Neurol 2008; 70: 308–311.
- 11Kimura N, Ishibashi M, Masuda T et al. Primary central nervous system lymphoma with cortical laminar hemorrhage. J Neurol Sci 2009; 287: 281–284.
- 12Rubenstein J, Fischbein N, Aldape K, Burton E, Shuman M. Hemorrhage and VEGF expression in a case of primary CNS lymphoma. J Neurooncol 2002; 58: 53–56.
- 13Streletz LJ, Terzic D, Salem K, Raza A, Deleu DT. CNS lymphoma masquerading as hemorrhagic stroke. Clin Neurol Neurosurg 2012; 114: 262–264.
- 14Matsumoto Y, Kashimura H, Aso K, Saura H, Osakabe M, Kurose A. Primary central nervous system lymphoma presenting as growing intracerebral hemorrhage. World Neurosurg 2018; 116: 155–158.
- 15Bureta C, Higa N, Makino R et al. Diffuse large B-cell lymphoma of the central nervous system manifesting with intratumoral hemorrhage: A case report and literature review. World Neurosurg 2020; 143: 490–494.
- 16Ohba S, Murayama K, Nishiyama Y et al. Clinical and radiographic features for differentiating solitary fibrous tumor/hemangiopericytoma from meningioma. World Neurosurg 2019; 130: e383–e392. https://doi.org/10.1016/j.wneu.2019.06.094
- 17Hans CP, Weisenburger DD, Greiner TC et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 2004; 103: 275–282.
- 18Makino K, Hirai T, Nakamura H et al. Differentiating between primary central nervous system lymphomas and glioblastomas: Combined use of perfusion-weighted and diffusion-weighted magnetic resonance imaging. World Neurosurg 2018; 112: e1–e6. https://doi.org/10.1016/j.wneu.2017.10.141
- 19Saini J, Kumar Gupta P, Awasthi A et al. Multiparametric imaging-based differentiation of lymphoma and glioblastoma: Using T1-perfusion, diffusion, and susceptibility-weighted MRI. Clin Radiol 2018; 73: 986.e7–986.e15.
- 20Suh CH, Kim HS, Jung SC, Park JE, Choi CG, Kim SJ. MRI as a diagnostic biomarker for differentiating primary central nervous system lymphoma from glioblastoma: A systematic review and meta-analysis. J Magn Reson Imaging 2019; 50: 560–572.
- 21Lin X, Lee M, Buck O et al. Diagnostic accuracy of T1-weighted dynamic contrast-enhanced-MRI and DWI-ADC for differentiation of glioblastoma and primary CNS lymphoma. Am J Neuroradiol 2017; 38: 485–491.
- 22Kitai R, Hashimoto N, Yamate K et al. Lymphomatosis cerebri: Clinical characteristics, neuroimaging, and pathological findings. Brain Tumor Pathol 2012; 29: 47–53.
- 23Kim WY, Lee HY. Brain angiogenesis in developmental and pathological processes: Mechanism and therapeutic intervention in brain tumors. FEBS J 2009; 276: 4653–4664.
- 24Machein MR, Plate KH. VEGF in brain tumors. J Neurooncol 2000; 50: 109–120.
- 25Shweiki D, Itin A, Soffer D, Keshet E. Vascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis. Nature 1992; 359: 843–845.
- 26Plate KH, Breier G, Weich HA, Risau W. Vascular endothelial growth factor is a potential tumour angiogenesis factor in human gliomas in vivo. Nature 1992; 359: 845–848.
- 27Yoshimura F, Kaidoh T, Inokuchi T, Shigemori M. Changes in VEGF expression and in the vasculature during the growth of early-stage ethylnitrosourea-induced malignant astrocytomas in rats. Virchows Arch 1998; 433: 457–463.
- 28Fonsatti E, Altomonte M, Nicotra MR, Natali PG, Maio M. Endoglin (CD105): A powerful therapeutic target on tumor-associated angiogenetic blood vessels. Oncogene 2003; 22: 6557–6563.
- 29Sugita Y, Takase Y, Mori D, Tokunaga O, Nakashima A, Shigemori M. Endoglin (CD 105) is expressed on endothelial cells in the primary central nervous system lymphomas and correlates with survival. J Neurooncol 2007; 82: 249–256.
- 30Smith SJ, Tilly H, Ward JH et al. CD105 (Endoglin) exerts prognostic effects via its role in the microvascular niche of paediatric high grade glioma. Acta Neuropathol 2012; 124: 99–110.
- 31Iwai Y, Ishida M, Tanaka Y, Okazaki T, Honjo T, Minato N. Involvement of PD-L1 on tumor cells in the escape from host immune system and tumor immunotherapy by PD-L1 blockade. Proc Natl Acad Sci U S A 2002; 99: 12293–12297.
- 32Iwai Y, Terawaki S, Honjo T. PD-1 blockade inhibits hematogenous spread of poorly immunogenic tumor cells by enhanced recruitment of effector T cells. Int Immunol 2005; 17: 133–144.
- 33Andorsky DJ, Yamada RE, Said J, Pinkus GS, Betting DJ, Timmerman JM. Programmed death ligand 1 is expressed by non-hodgkin lymphomas and inhibits the activity of tumor-associated T cells. Clin Cancer Res 2011; 17: 4232–4244.
- 34Chen BJ, Chapuy B, Ouyang J et al. PD-L1 expression is characteristic of a subset of aggressive B-cell lymphomas and virus-associated malignancies. Clin Cancer Res 2013; 19: 3462–3473.
- 35Miyoshi H, Kiyasu J, Kato T et al. PD-L1 expression on neoplastic or stromal cells is respectively a poor or good prognostic factor for adult T-cell leukemia/lymphoma. Blood 2016; 128: 1374–1381.
- 36Ishikawa E, Nakamura M, Shimada K et al. Prognostic impact of PD-L1 expression in primary gastric and intestinal diffuse large B-cell lymphoma. J Gastroenterol 2020; 55: 39–50.
- 37Tsuyuki Y, Ishikawa E, Kohno K et al. Expression of programed cell death ligand 1 by immune cells in the microenvironment is a favorable prognostic factor for primary diffuse large B-cell lymphoma of the central nervous system. Neuropathology 2020. https://doi.org/10.1111/neup.12705 [Epub ahead of print].
- 38Yamada S, Ishida Y, Matsuno A, Yamazaki K. Primary diffuse large B-cell lymphomas of central nervous system exhibit remarkably high prevalence of oncogenic MYD88 and CD79B mutations. Leuk Lymphoma 2015; 56: 2141–2145.
- 39Nakamura T, Tateishi K, Niwa T et al. Recurrent mutations of CD79B and MYD88 are the hallmark of primary central nervous system lymphomas. Neuropathol Appl Neurobiol 2016; 42: 279–290.
- 40Zheng M, Perry AM, Bierman P et al. Frequency of MYD88 and CD79B mutations, and MGMT methylation in primary central nervous system diffuse large B-cell lymphoma. Neuropathology 2017; 37: 509–516.
- 41Nayyar N, White MD, Gill CM et al. MYD88 L265P mutation and CDKN2A loss are early mutational events in primary central nervous system diffuse large B-cell lymphomas. Blood Adv 2019; 3: 375–383.
- 42Takano S, Hattori K, Ishikawa E et al. MyD88 mutation in elderly predicts poor prognosis in primary central nervous system lymphoma: Multi-institutional analysis. World Neurosurg 2018; 112: e69–e73. https://doi.org/10.1016/j.wneu.2017.12.028