Exploring exercise, physical wellbeing and the role of physiotherapy: perspectives from people with narcolepsy
Summary
Narcolepsy is associated with reduced quality of life and physical performance. The study aimed to explore the attitudes of people with Type 1 narcolepsy towards exercise and physical activity, their physical wellbeing, and the potential role of physiotherapy. Semi-structured interviews were conducted with 22 people with narcolepsy attending a dedicated outpatient narcolepsy clinic located in Dublin, Ireland. Transcripts were iteratively coded; a thematic analysis was undertaken, and key themes were identified. Four themes were identified: ‘Barriers and Facilitators to Exercising’, ‘Social Concerns’, ‘Health Concerns’ and ‘Suggestions for the Role of Physiotherapy’. Future research should explore the potential role of exercise to help manage narcolepsy-related symptoms in this population.
1 INTRODUCTION
The term ‘narcolepsy’ derives from the Greek words ‘narke’ and ‘lepsis’, which translates into a fit of stiffness. Narcolepsy is a disabling neurological condition that affects an individual's ability to regulate sleep–wake patterns. This chronic sleep disorder is characterised by excessive daytime sleepiness and is frequently associated with episodic muscular weakness, known as cataplexy, following intense emotions such as laughter or anger. The presence of cataplexy is thought to be pathognomonic and is used to distinguish narcolepsy with cataplexy (Type 1 narcolepsy) from narcolepsy without cataplexy (Type 2 narcolepsy). Disrupted night-time sleep (DNS) is frequently reported by people with narcolepsy and may be associated with sleep paralysis and hallucinations (Roth et al., 2013). Narcolepsy has an incidence of 25–50 per 100,000 people, or 0.74 per 100,000 person-years (Longstreth et al., 2007). Additionally, a slight male predominance has been identified in males with incidence rates (1.6:1) and prevalence (1.8:1) in narcolepsy (Silber et al., 2002). Ireland experienced an increased number of cases of narcolepsy following the 2009–2010 H1N1 influenza (swine flu) epidemic with crude associations identified in pandemic-vaccination recipients (O'Flanagan et al., 2014). This increase in cases was also observed in other European countries such as Norway (Heier et al., 2013), Finland (Nohynek et al., 2012; Partinen et al., 2012) and Sweden (Szakacs et al., 2013).
Narcolepsy is a condition that can significantly affect an individual's overall functioning by imparting deleterious effects on their social and physical wellbeing (Schiappa et al., 2018). The significant symptom burden associated with narcolepsy can manifest in a multitude of ways, from impairment of mental health, social exclusion, increased healthcare usage, or decreased employment and education opportunities (Kapella et al., 2015). Psychiatric comorbidities are commonly reported in people with narcolepsy, with over half (57%) of this cohort reportedly exhibiting symptoms of depression (Daniels et al., 2001; Dauvilliers et al., 2009). This correlation supports the theory proposed by Morse and Sanjeev (2018) that the significant symptom overlap shared by narcolepsy and psychiatric illnesses contributes to the development of psychiatric comorbidities in people with narcolepsy. The significant symptom burden associated with narcolepsy has a major impact on the physical and psychosocial wellbeing of this cohort, and health-related quality of life (HRQoL) is often impaired as a consequence of this burden (Dodel et al., 2004; Kapella et al., 2015; Tadrous et al., 2021).
The relationship between physical functioning and symptom severity in people with narcolepsy is not fully understood and is likely complex. In a study by Matoulek et al. (2017), poorer cardiorespiratory fitness was shown to correlate with increased severity of excessive daytime sleepiness and the frequency of cataplexy attacks. In children with narcolepsy, there was a positive correlation between increased physical activity and lower body mass index (BMI), increased night-time sleep duration, higher sleep quality, and reduced frequency of napping (Filardi et al., 2018). Furthermore, considerably lower physical activity has been reported in people with narcolepsy than in the general population (Parmar et al., 2019), and this reduced physical activity has been shown to correlate with depressive symptoms in people with narcolepsy (Bruck et al., 2005). However, the studies that explored physical activity in people with narcolepsy have been cross-sectional in design, and causality between physical activity and improved symptom severity or comorbidity has not been demonstrated through prospective studies.
In the general population, relationships have been identified between exercise and sleep, with exercise acting as an effective non-pharmacological treatment option for disturbed sleep, and poor sleep contributing to lower physical activity levels (Kline, 2014). However, little is known about people with narcolepsy's attitudes towards their physical health and exercise. As such, the overall aim of this study was to ascertain this study population's attitudes towards physical health, their barriers regarding exercise and physical activity, and their perception of physiotherapy.
2 METHODS
2.1 Study design
This study conducted semi-structured interviews with people with narcolepsy attending a dedicated narcolepsy outpatient clinic at St. James's Hospital, Dublin. The Narcolepsy Clinic in St James's Hospital is home to the National Narcolepsy Centre, complete with a fully equipped state-of-the-art sleep laboratory. The dedicated narcolepsy team consists of a medical consultant, clinical nurse specialist and clinical nutritionist. Ethical approval for this study was obtained from the St. James's Hospital and Tallaght University Hospital Research Ethics Committee. This study was registered on Clinicaltrials.gov (NCT04419792). Written informed consent was obtained from each participant prior to study participation. The design and reporting of research methods used in this study were informed by the COREQ (COnsolidated criteria for REporting Qualitative research) standardised reporting guidelines (Tong et al., 2007).
2.2 Study population
Participants were required to meet the following eligibility criteria: aged 18–65 years, diagnosed with Type 1 or Type 2 narcolepsy based on the third edition of the International Classification of Sleep Disorders criteria (American Academy of Sleep Medicine, 2014) for at least 6 months prior to the study, eligibility screened by their treating clinician, and able to understand English and follow simple instructions to enable completion of interviews. Additionally, participants were required to provide signed and informed consent to participate in the study, and for the processing of their data to be eligible for participation. Individuals with sleep disorders other than narcolepsy were excluded from participating in the study.
2.3 Recruitment
Potential participants were screened by their treating clinicians in advance of their scheduled clinic visit and sent an information leaflet at least 5–7 days before their appointment if deemed eligible to participate. A follow-up call from the specialist nurse was made to answer any study-related questions. During their clinic visit, the primary study assessor (a research physiotherapist, R.T.) approached potential participants and provide additional information regarding the study. Participants were initially recruited to undertake a test battery of physical performance measures that will be reported elsewhere, and semi-structured interviews were conducted following the completion of the test battery.
2.4 Qualitative interview
A qualitative interview to explore perceptions of unmet physical health needs was carried out by the research physiotherapist (R.T.) in the Physiotherapy Department at St James's Hospital. A semi-structured interview guide was developed (Data S1), which incorporated open-ended questions to facilitate discussion. Interviews lasted ~30 min, and participants were asked several open-ended questions that were audio-recorded and transcribed verbatim by the study assessor.
2.5 Data analysis
- Data Transcription: responses were audio-recorded and transcribed verbatim by the study assessor (R.T.). Data were then read, re-read and initial ideas from the responses were noted.
- Generating Initial Themes: interesting features of the data were coded using a systematic approach across the complete data set. Interesting aspects from the responses were also noted during this phase.
- Searching for Themes: similar codes that were generated were collated into potential themes. All relevant data were grouped under these specific themes.
- Reviewing Themes: themes were reviewed in relation to the identified codes and the entire data set. In doing so, this process generated a thematic ‘map’ of the analysed data.
- Defining and Naming Themes: themes were continuously analysed and refined based on specific aspects identified to create an overall story of the analysed data. Clear definitions and names were created for each theme.
- Producing the Report: vivid and compelling extracts from responses were selected that related to the specific research questions and literature in order to produce a comprehensive report of the analysis. No repeat interviews took place and transcripts were not returned to participants for accuracy.
3 RESULTS
3.1 Recruitment
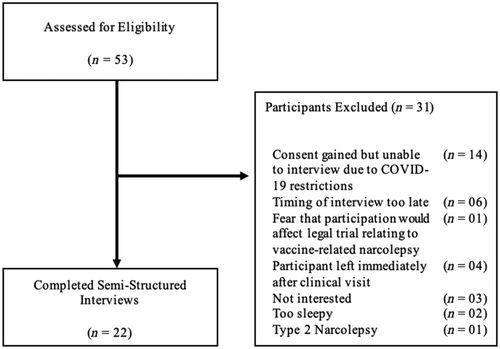
A total of 22 participants undertook semi-structured interviews (Figure 1). The demographic characteristics of the study participants are reported in Table 1. Just over half of the sample was female (n = 12 [56.52%]), and all participants were diagnosed with narcolepsy with cataplexy. The mean (SD, range) age of the participants was 31.4 (13.2, 20–63) years. The majority of participants lived with their families (n = 19 [86.36%]), and 45.45% (n = 10) were in full-time education.
| Demographics | Value |
|---|---|
| Gender, n (%) | |
| Males | 10 (45.45) |
| Females | 12 (54.55) |
| Age, years | |
| Mean (SD) | 31.4 (13.2) |
| Range | 20–63 |
| Median | 25 |
| Living arrangements, n (%) | |
| Alone | 1 (4.55) |
| Partner | 2 (9.01) |
| Family | 19 (86.36) |
| Highest educational achievement, n (%) | |
| Second-levela | 12 (54.55) |
| Third-levelb | 10 (45.45) |
| Current education/employment status, n (%) | |
| Currently enrolled as a student | 10 (45.45) |
| Employed | 9 (40.91) |
| Unemployed/retired | 3 (12.64) |
| Medications (n = 37), n (%) | |
| Modafinil | 12 (32.43) |
| Venlafaxine | 9 (24.32) |
| Wakix | 5 (13.51) |
| Concerta | 4 (10.81) |
| Ritalin | 4 (10.81) |
| Other | 3 (8.12) |
- a Comprising of secondary, vocational, community or comprehensive schools.
- b Higher education in universities and colleges, or further education through other courses.
3.2 Thematic analysis of open-ended responses
Four main themes were identified from their responses. The four main themes were: ‘Barriers and Facilitators to Exercise’, ‘Social Concerns’, ‘Health Concerns’, and ‘Suggestions for the Role of Physiotherapy’ (Table 2).
| Theme | Subthemes | Illustrative quotes, patient number (sex, age) |
|---|---|---|
| 1. Barriers and facilitators to exercise | Barriers | |
| Psychological barriers limiting participation in exercise | ‘My anxiety-getting out can be quite difficult.’ | N06 (F, 45 years) ‘My mood can be quite low, or apathetic. I feel this has been a major barrier to exercising, like I can do it, but I could not care to do it.’ | N03 (F, 24 years) ‘If I feel like I do not know what I'm doing, and people are staring at me it can really put you off going.’ | N07 (F, 26 years) |
|
| Fatigue and tiredness limiting ability to exercise | ‘At the end of the day, I just want to go to bed instead of going for a run/going to the gym.’ | N01 (F, 25 years) ‘I hate using this excuse, but I just feel tired.’ | N03 (F, 24 years) ‘It's very difficult to exercise when sleepy. I like to exercise in the morning but am unable to when I sleep poorly.’ | N05 (F, 42 years) |
|
| Fear of cataplexy limiting participation in exercise | ‘I’m scared to do things because of my cataplexy. I had one bad attack in a gym before, and that's made me more anxious overall.’ | N03 (F, 24 years) ‘Feeling weak, anxious or self-conscious, particularly in a gym, can greatly increase my likelihood of experiencing cataplexy.’ | N07 (F, 26 years) ‘I used to love playing football when I was younger. I get cataplexy attacks when I'm surprised or excited. If running to catch a bus is enough to trigger it, I think exercise would do the same.’ | N08 (M, 59 years) |
|
| Accessibility limiting participation in exercise | ‘Time constraints, making time to do things can be difficult. I have access to a gym, but I use it sparingly.’ | N19 (M, 19 years) ‘I used to exercise in a gym for 40 min, but the price is too high.’ | N15 (F, 63 years) ‘The cold weather really discourages me, especially when it is dark.’ | N22 (F, 20 years) |
|
| Facilitators | ||
| Career/education | ‘I'm not letting narcolepsy stop me from pursuing my career.’ | N01 (F, 24 years) ‘My fitness matters a lot to me, also my family and education-keeping on top of everything at the moment really.’ | N12 (F, 24 years) ‘My health and my career are my priorities. I wanted to do something that benefited my health, and that's why I changed careers.’ | N07 (F, 26 years) |
|
| Social wellbeing | ‘Staying on top of my work and finding time to socialise and exercise.’ | N11 (F, 22 years) ‘My family-I want to be able to do stuff with my children.’ | N06 (F, 45 years) ‘I want to keep a healthy balance with everything; my family, my social life, my hobbies and exercise, and my relationships.’ | N10 (M, 22 years) |
|
| Health and wellbeing | ‘I want to lose weight, be happier and improve my life in order to have the energy to do what I want.’ | N03 (F, 24 years) ‘My health is my biggest priority… I need to get back to a normal weight.’ | N17 (M, 25 years) ‘Not letting my symptoms get any worse, I can just about handle how it is at the moment.’ | N02 (M, 20 years) |
|
| 2. Social concerns | Impact of narcolepsy on career and education | ‘Getting a job-I'm focused on developing my career at the moment.’ | N16 (M, 22 years) ‘My career, I'm not really focusing on my health at the moment. I would like to increase this focus going forwards.’ | N14 (M, 20 years) ‘I'm worried if I'll still be able to do what others are able to do in 10 years’ time when my youthful energy fades.’ |N01 (F, 25 years) |
| Impact of narcolepsy on familial relationships | ‘My son, it's difficult falling asleep when I'm spending time with him.’ | N21 (M, 27 years) ‘I want to be able to do stuff with my children, I need to work around everything with my narcolepsy.’ | N06 (F, 45 years) ‘It's not as easy as it used to be, my children are getting older. Life does not get easier with age; I feel time is slipping away.’ | N08 (M, 59 years) |
|
| Impact of narcolepsy on social life | ‘I want to keep a healthy balance with everything, my family, my social life, my hobbies and exercise, and my relationships. It can be difficult to manage due to narcolepsy, but I'll try my best anyways.’ | N10 (M, 22 years) ‘It feels like you have to work so much harder than others. You only have a limited amount of energy, so oftentimes I have to choose between socialising or studying.’ | N01 (F, 25 years) ‘Staying on top of my work and housework, finding time to socialise and exercise. I feel exercise was more important to me previously, but I changed jobs recently and have been finding it difficult.’ | N11 (F, 22 years) |
|
| 3. Health concerns | Weight gain following diagnosis | ‘My weight, definitely, I try not to worry about it, but it is an issue.’ | N04 (F, 46 years) ‘I gained 5 stone after I was diagnosed with narcolepsy 19 years ago, and I’ve been fighting to lose it ever since.’ | N15 (F, 63 years) ‘I have put on 10 stone since I’ve been diagnosed. I do not like the way I look; I am self-conscious about my weight.’ | N17 (M, 25 years) |
| Reduction of physical fitness | ‘I have not played sport since I finished college 2 years ago.’ | N13 (F, 24 years) ‘I need to be more active. I do Zumba three times per week, but for the rest of the week I'm doing nothing except housework.’ | N06 (F, 45 years) ‘My biggest concern is that I’m not going to the gym regularly enough. It's difficult after a long day at work to not get into a slump.’ | N11 (F22 years) |
|
| Pain | ‘I am concerned about the weight that I've gained as it's affecting me. I now have pain in my shoulders, hips, back and neck from the weight gain.’ | N03 (F, 24 years) ‘I need to be more active. I'm studying for exams at the moment and just sitting at a desk all day is causing me shoulder and back pain.’ | N10 (M, 22 years) |
|
| 4. Suggestions for the role of physiotherapy | Advice on reintroducing exercise | ‘I have no experience with exercise, I would not know what to do. I think it would be great to improve my awareness and knowledge with exercise and show me how to ease into exercising.’ | N08 (M, 59 years) ‘Advice on how to get back to exercising, how to fit it into your schedule, activities to do at home or around my community.’ | N13 (M, 43 years) |
| Physiotherapist prescribed exercise program | ‘I'm fed up with doing the same exercises all the time. My knowledge regarding exercise is quite limited.’ | N15 (F, 63 years) ‘Provision of “lighter” exercises would be useful. I feel it would help motivate you to do something if you are unable to complete an entire workout, that less is better than none.’ | N01 (F, 25 years) |
|
| External source of motivation to promote adherence | ‘It's easier to come up with an excuse than it is to exercise. If I need to be at a meeting, I physically need to be there. But with exercise it's self-directed, and I find myself taking the easy way out.’ | N20 (F, 44 years) ‘I would greatly appreciate one-to-one sessions to help gain confidence with exercising.’ | N07 (F, 26 years) ‘It would greatly improve my motivation to get back exercise, even just having someone check in would boost my commitment.’ | N22 (F, 20 years) |
|
- Abbreviations: F, female; M, male; N, participant number.
3.3 Theme 1: Barriers to exercise
All participants (n = 22) reported exercising on a weekly basis. Respondents were asked what the main barriers they encounter that prevent them from exercising. From the responses obtained from participants, four main barriers were identified.
3.3.1 Psychological barriers limiting participation in exercise
Participants expressed several psychological barriers towards exercising. For some participants, their anxiety towards exercising prevented them from participating in regular activities. For others, low mood posed a considerable barrier towards regularly engaging in exercise. Other participants expressed that their lack of confidence made them reluctant to exercise.
3.3.2 Fatigue and tiredness limiting ability to exercise
Narcolepsy-related fatigue and tiredness were frequently reported by participants as considerable barriers towards exercise. One participant described their difficulties with managing a finite amount of energy, whereas another described the stigma surrounding narcolepsy and experiencing fatigue as a young adult. DNS was also reported to contribute to fatigue and tiredness and presented a considerable barrier to engaging in exercise.
3.3.3 Fear of cataplexy limiting participation in exercise
Cataplexy was a frequently reported barrier to exercising among participants. Several respondents reported having prior experiences with cataplexy in public spaces that discouraged them from exercising. Another participant expressed that feeling self-conscious whilst exercising exacerbated their cataplexy, whilst others expressed that their cataplexy prevented them from participating in previously enjoyed hobbies.
3.3.4 Accessibility
Accessibility-related issues were the final barrier towards exercising reported by this sample. Some participants expressed that timing was an issue, particularly with managing fatigue and other commitments. For others, the financial costs associated with exercising prevented them from exercising. The last major accessibility-related barrier reported by participants related to poor weather conditions, particularly in winter.
3.4 Motivators
Participants expressed several factors that motivated them to exercise and be active. These motivators ranged from their career or education, prevention of the progression of their condition, and their physical and social wellbeing.
3.4.1 Career/education
The vast majority of the younger participants reported that advancing their careers and their education mattered to them the most at this stage in their lives. Some expressed that, to them, exercise, and their physical wellbeing were integral to achieving this, with one participant expressing they changed careers to something more active to help manage their physical wellbeing.
3.4.2 Social wellbeing
Maintaining interpersonal relationships was one of the most frequently reported priorities expressed by participants. Several participants expressed that their motivation for improving their physical wellbeing was to ensure that they could spend time with their loved ones. Additionally, maintaining balance and control over their lives was a common sentiment expressed by several participants.
3.4.3 Health and wellbeing
Maintaining their overall health and wellbeing was a major priority and motivator that was reported by participants in this sample. Participants expressed concern regarding the progression of their narcolepsy-related symptoms and improve their overall wellbeing.
3.5 Theme 2: Social concerns
The impact of narcolepsy on social wellbeing was frequently reported by people with narcolepsy in this sample. These social concerns ranged from the impact of narcolepsy on their career, family and relationships, and social life.
3.5.1 Impact on career and education
Given the young age of the sample, participants were focused on developing their careers. Several participants expressed concern about how narcolepsy would affect their careers. Sometimes, the pursuit of developing their career was prioritised ahead of their health. Other participants were worried about the impact of narcolepsy-related symptoms as they get older.
3.5.2 Impact on familial relationships
Participants expressed the considerable impact narcolepsy can have on their relationships with their families. A parent of a young child expressed how their symptoms were affecting their relationship with their child, such as sleeping when they are meant to be spending time together. This sentiment of trying to spend quality time with their children was also shared by other parents. Additionally, one participant, who was diagnosed with narcolepsy over 30 years ago, expressed how the difficulties associated with being a parent with narcolepsy have increased with age.
3.5.3 Impact on social wellbeing
Difficulty with managing their social wellbeing was frequently reported by participants. Participants expressed that keeping their commitments to friends, family, hobbies and education or employment was very important to them. Other participants reported the difficulties of maintaining a healthy social life when living with narcolepsy, particularly with competing commitments and that oftentimes socialising and exercise would be neglected to prioritise education or employment.
3.6 Theme 3: Health concerns
Three main health concerns were identified from the open-ended responses. These concerns included weight gain, pain, and reduced physical activity.
3.6.1 Weight gain
Several participants reported that their weight was the biggest concern regarding their health, with many reporting considerable weight gain following receiving a diagnosis of narcolepsy. Participants reported having great difficulty with attempting to lose this weight and the considerable impact this weight gain had on their physical and mental wellbeing.
3.6.2 Reduced physical activity
Inactivity was the second most reported concern regarding the respondent's physical health. Some participants reported being more physically active in the past as a result of having access to sports through university. Others reported that although they were physically active and exercising several times per week, it was their sedentary behaviour that was concerning them. Exercising in the evenings was reported to be particularly difficult, owing to tiredness associated with employment or education.
3.6.3 Pain
Pain was also a frequently reported health concern. Common causes of pain reported by participants included weight gain following diagnosis causing musculoskeletal pain and following prolonged periods of sedentary behaviour associated with education or employment.
3.7 Theme 4: Role of physiotherapy
Participants were asked how they felt that physiotherapy could address the aforementioned concerns with their physical health. Responses included physiotherapist-designed exercise programmes, advice on how to reintroduce exercise, and providing external sources of motivation.
3.7.1 Advice on reintroducing exercise
Many participants reported considerable difficulty when trying to reintroduce exercise following receiving their diagnosis of narcolepsy. For some, these difficulties arose from a lack of knowledge regarding exercise and how to reintroduce exercise into their routine. Other participants suggested advice on how to structure exercise around their schedule and advice on exercising at home and in the community.
3.7.2 Physiotherapist prescribed exercise programmes
Participants who were familiar with exercising expressed that they would like exercise programmes prescribed by a physiotherapist to complete independently. Participants expressed that programmes should be designed to require little equipment to help overcome the financial barrier associated with gyms. Participants suggested the provision of exercise programmes that varied in intensity to accommodate the fluctuating nature of fatigue in people with narcolepsy.
3.7.3 External source of motivation to promote adherence
Difficulties with escaping the vicious cycle of sedentary behaviour were frequently reported by participants. This issue seemed to stem from a lack of motivation and challenges with making oneself accountable for engaging in regular exercise. With a lack of self-confidence being a major psychological barrier towards exercising as reported by participants, a common suggestion by participants to encourage exercise and promote adherence was one-to-one physiotherapy sessions. One participant expressed how this external source of motivation would assist her in returning to exercise.
4 DISCUSSION
To our knowledge, this is the first qualitative study that has explored the attitudes of people with narcolepsy towards exercise, physical activity, and the potential role of physiotherapy in managing their physical wellbeing. This study focused on people with Type 1 narcolepsy, given the established associations between obesity in people with Type 1 narcolepsy (Bassetti et al., 2019), particularly in those who do not regularly exercise (Filardi et al., 2018), as highlighted during the COVID-19 pandemic (Postiglione et al., 2021).
Exercise has the potential to be a powerful, non-pharmacological management strategy for people with narcolepsy. A bidirectional relationship between physical activity and sleep has been identified, with physical activity demonstrating the ability to improve sleeping and promote wakefulness, and poor sleep resulting in reduced physical activity (Kline, 2014). Additionally, physical activity is associated with longer sleep duration, higher sleep quality, reduced BMI and nap frequencies in people with narcolepsy (Filardi et al., 2018). There is a potential interrelationship present between physical wellbeing and mental wellbeing in people with narcolepsy (Morse & Sanjeev, 2018), with less physical activity in people with narcolepsy being linked to poorer mood (Bruck et al., 2005). People with narcolepsy typically have reduced opportunities to exercise due to time constraints related to sleepiness and social isolation (Kapella et al., 2015), and considerably lower physical activity has been reported in people with narcolepsy compared with the general population (Parmar et al., 2019). A vicious cycle can be established with sedentary behaviour promoting increased sleepiness severity (Golden & Lipford, 2018), and this increased symptom burden further reduces habitual levels of physical activity and HRQoL (Matoulek et al., 2017). The impact of physical activity levels on physical and mental wellbeing in this population warrants further exploration.
The main health concerns reported by those interviewed were weight gain, reduced physical activity, and pain. Studies have shown that people with narcolepsy have a higher incidence of obesity (Dahmen et al., 2001), are more likely to experience chronic pain (Cremaschi et al., 2019), and have lower physical activity levels than the general population (Parmar et al., 2019). In the general population, exercise is routinely used to manage these health concerns (Wiklund, 2016; Zdziarski et al., 2015). The main barriers to exercising are related to fatigue and mental wellbeing. Participants reported feelings of anxiety and depression limiting their ability to partake in exercise, both of which have been reported to increase the perception of pain (Michaelides & Zis, 2019). Similarly, the relationship between fatigue, physical activity, and weight gain has been established (Engberg et al., 2017). Addressing these barriers to exercise in an attempt to increase exercise levels and target the aforementioned health concerns could improve their overall wellbeing, as the most affected HRQoL domains in people with narcolepsy were physical role limitations and emotional role limitations (Tadrous et al., 2021). Addressing fatigue and providing mental wellbeing support may assist people with narcolepsy in increasing their exercise levels and assist in addressing their health concerns.
The other main barriers to exercising included cataplexy and accessibility-related issues. Some participants reported that they avoided exercise due to their cataplexy, citing that feeling anxious, self-conscious, or nervous increased the likelihood of having a cataplexy attack. Although less common than positive emotions such as laughing, negative emotions such as fear and anxiety can result in cataplexy episodes (Pelayo & Lopes, 2016). This fear associated with exercising was exacerbated by a lack of knowledge on how to exercise, and what exercises were appropriate. However, participants perceived these barriers as surmountable that was highlighted by the responses obtained relating to the desired roles of physiotherapy, which centred around education, tailored exercise advice, and lifestyle behaviour change. Furthermore, the barriers relating to the inaccessibility of exercise such as time constraints and financial constraints in people with narcolepsy could potentially be addressed through the provision of tailored exercise prescriptions that can be completed at home.
This study was limited by the homogeneity of the recruited sample, with the majority of participants being aged 20–30 years, and with all being diagnosed with Type 1 narcolepsy. As such, the transferability of these findings may be limited, particularly for children and older people with narcolepsy, and further research is warranted in these populations. Additionally, participation bias must be considered. Convenience sampling was used rather than purposive sampling, as participants were initially recruited to undertake a test battery of physical performance measures, which will be reported elsewhere, and semi-structured interviews were conducted following the completion of the test battery. As such, individuals who agreed to participate may have been more actively pursuing strategies to optimise their physical wellbeing already. Consequently, the results obtained from this sample must be cautiously interpreted as they may not be wholly representative of the general population of people with narcolepsy.
People with narcolepsy are generally not referred to physiotherapists for specialised exercise recommendations. Given their expertise in exercise prescription, the potential role of physiotherapists in the interdisciplinary management of narcolepsy is promising. However, a significant knowledge gap must first be overcome, as the awareness of physiotherapists regarding the management of sleep disorders is limited. From the open-ended responses, participants identified issues they perceived physiotherapy could assist them with, namely physical activity and exercise advice, and lifestyle behaviour change. Further research is warranted in this cohort to assist in justifying the role of physiotherapy in the management of narcolepsy. This additional research should focus on exploring the potential modulating effects of exercise on narcolepsy-related symptoms in this cohort.
AUTHOR CONTRIBUTIONS
Tadrous, R: Investigation; writing – original draft; methodology; writing – review and editing; formal analysis; project administration. O’ Rourke D: Conceptualization; methodology; writing – review and editing; supervision. Murphy N: Conceptualization; funding acquisition; resources. Quinn G: Conceptualization; writing – review and editing; supervision. Quinn C: Formal analysis; writing – review and editing. Slattery L: Project administration. Broderick, J: Conceptualization; writing – review and editing; methodology; supervision.
ACKNOWLEDGEMENTS
This review was completed as part of Mr Ragy Tadrous’ Master of Science (MSc) degree in Trinity College Dublin. This degree was co-sponsored by the Physiotherapy Department in St James's Hospital, Dublin. Open access funding provided by IReL.
CONFLICT OF INTEREST STATEMENT
All authors declare that they have no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.




