Specialized medical care for people with intellectual disabilities: A retrospective cohort study in an outpatient ID practice
Abstract
People with intellectual disabilities (ID) experience complex medical care needs and high levels of multimorbidity. In mainstream healthcare, these needs might remain undetected leading to unmanaged health problems and avoidable deaths. In the Netherlands, general practitioners (GPs) can refer to specialized ID physicians when ID-specific expertise is required. Little is known about the characteristics of specialized medical care for people with ID. This study explores the characteristics of specialized medical care for people with ID, including the interplay between medical-, psychological-, and context-related problems. A retrospective cohort study using medical records of patients with ID who had visited the outpatient ID practice in Nijmegen, the Netherlands. Medical records (n = 128) were analyzed using descriptive statistics, focusing on (1) reasons for initial consultation, (2) health-related problems identified during initial consultation, and (3) disciplines involved following initial consultation. Analyses were performed separately for patients who were referred by a medical professional and patients who visited the practice for proactive health checks related to the etiological diagnosis. Patients often initially visit the outpatient ID practice for one type of complaint, most often psychological. Diverse, multiple, and interconnected problems were identified during specialized medical ID consultation. A range of specialist professionals (n = 25) were involved by the ID physician. The health-related problems of people with ID seen at the outpatient ID practice are diverse and interconnected, and originate from an interplay between medical-, psychological-, and context-related problems. This complexity is not mirrored in the reasons for referring to the outpatient ID practice. It is essential to go beyond medical views and assess health complaints in an integrated way, including the way ID can influence all levels (physical, mental, contextual) of the experienced health issue within the context of everyday life.
Abbreviations
-
- CV group
-
- consultation visit group
-
- GDPR
-
- general data protection regulation
-
- GP
-
- general practitioner
-
- HC group
-
- health check group
-
- ICPC-2
-
- international classification of primary care, second edition
-
- ID
-
- intellectual disabilities
-
- RTC
-
- Radboud technology center
BACKGROUND
People with intellectual disabilities (ID) have more complex and different medical care needs than the general population (Krahn et al., 2006; van Schrojenstein Lantman-de valk & Walsh, 2008). About 120 million people, or 1.5% of the world's population, have ID (Cooper et al., 2004; Cuypers et al., 2021; Maulik et al., 2011; World Health Organization, 2001). An ID is defined as significant limitations that originate during the developmental period in both intellectual functioning and adaptive behavior (Schalock et al., 2021). People with ID have different morbidity patterns and experience more comorbidity- and syndrome-related health problems compared with the general population (Bekkema et al., 2014; Phillips et al., 2004). The complex health problems of people with ID often reach beyond medical problems alone and are influenced by psychological- and context-related problems (Krahn et al., 2006; Sappok et al., 2019; Sullivan et al., 2006). The influence of these problems and their interactions can be easily overlooked in people with ID, because of difficulties such as atypical symptom presentations and difficulties in communication and health information exchange between patients, professionals, and informal carers (Mastebroek et al., 2014, 2016).
Not all medical care providers are familiar with the special medical care needs of people with ID. For example, general practitioners (GPs) view their current medical care provision for people with ID to be of limited quality and effectiveness and both GPs and medical specialists report a lack of initial training in providing medical care for people with ID (Bakker-van Gijssel et al., 2017; Lennox et al., 2000; Phillips et al., 2004; Pouls et al., 2022). Specialized ID training and education for medical care providers have been widely suggested as a solution to improve healthcare for people with ID (Breuer et al., 2022; Ervin et al., 2014; Krahn et al., 2006; Lennox et al., 1997; Straetmans et al., 2007). However, there is a need for rigorous studies on the role of specialist ID services in facilitating access to healthcare services or on how they may support mainstream healthcare providers in providing medical care for people with ID (Balogh et al., 2016).
The Netherlands has a specialization for medical care for people with ID. Physicians who complete a 3-year vocational postgraduate training in population-specific knowledge, skills, and attitude are registered as specialized ID physicians. The ID physician is a population-oriented general specialist with expertise in health problems related to or colored by ID, in people of all ages and ID levels (Moonen et al., 2022). ID physicians predominantly work in care organizations, but there are also outpatient clinics where ID physicians work and to which the GP or medical specialist can refer patients with ID when ID-specific expertise is required (Moonen et al., 2022).
The setting of this outpatient clinic offers the opportunity to explore the value of specialized medical ID expertise in facilitating the identification of health-related problems in people with ID and the characteristics of specialized medical care provided to people with ID in practice. To illustrate this, we provide an example case; a GP refers a patient with behavioral problems (psychological problem) to the outpatient ID practice. During the consultation, the ID physician discovers that the patient experiences hearing difficulties. The ID physician does a medical exam and finds out that the patient's ears are clogged from wax build-up (medical problem). Not hearing, understanding, and comprehending his environment and vice versa (context-related factor) resulted in an angry and agitated patient. When the ears were cleared from earwax, the patient's behavior stabilized to the point where it was not problematic. An audiologist was engaged by the ID physician to check whether the patient needed hearing aids.
This study focuses on (1) the reasons for initially visiting the outpatient ID practice, (2) the health-related problems identified during initial consultation, and (3) the disciplines involved following this consultation.
METHODS
Setting and design
This is a retrospective cohort study using routine data from the outpatient ID practice in Nijmegen, the Netherlands. Since 2015, the outpatient ID practice has registered the provided specialized medical care for people with ID in electronic patient health records. All patient encounters have been registered electronically using a health information system (TransHIS). This system registers the reason for consultation and the main health problem(s) during consultation according to the International Classification of Primary Care, Second Edition (ICPC-2; WONCA International Classification Committee, 1998). Furthermore, ID physicians added clinical entries in an electronic journal.
The outpatient ID practice collects informed consent (opt-in) for the use of patient data for research purposes since 2020. For patients who visited the practice before 2020, informed consent was obtained via an opt-in procedure. Informed consent forms were composed in conformity with the GDPR (General Data Protection Regulation) in easy-to-read language (see Supplementary Forms S1 and S1b). If the patients did not have the capacity to consent (e.g., children or people with moderate to profound ID), their legal representative signed.
This study extracted data from the health records of patients who visited the practice between April 2015 and March 2021 when informed consent was present (preregistration https://doi.org/10.17605/OSF.IO/W8GA7). The Medical Ethical Committee (CMO regio Arnhem – Nijmegen) waived the need for further ethical assessment [2020-6090].
Study population
The patient population of the outpatient ID practice has a varying level of ID from mild to profound. Two groups of patients receive care from the outpatient ID practice in Nijmegen. The first group (consultation visit [CV] group) comprises patients referred to the outpatient ID practice by a medical professional, often a GP. These patients have a health complaint or problem requiring ID-specific expertise, thus having a specific, active care demand. The second group (health check [HC] group) comprises patients who have an etiological diagnosis of their ID (e.g., 22q11 syndrome) and visit the outpatient ID practice for proactive health checks related to the etiological diagnosis. These patients are generally referred by a developmental pediatrician and younger in age. Because of the different reasons for visiting the outpatient ID practice, the results for the two groups will be described separately.
Data
Data from initial consultations were extracted from the electronic medical records by the Radboudumc Technology Center (RTC) Health Data of the Department of Primary and Community Care. Data were pseudonymized and provided to the research team. These records include information on the reason for consultation, anamnesis, physical examination, evaluation and conclusion, and additional actions, registered in ICPC-2 codes and written text clinical entries in the electronic journal. Extracted data consisted of patient demographics, reasons for initial consultation (entered at registration), health-related problems identified during initial consultation, and disciplines involved following initial consultation. The reasons for initial consultation were extracted by combining two types of data: (1) registered ICPC-2 codes on the reasons for initial consultation and (2) clinical entries in the electronic journal (Table S1). The clinical entries consisted of open text and were manually coded by the first author using ICPC-2 codes to facilitate merging the two types of data. After merging, the complete list of reasons for initial consultation was grouped into three types: medical-, psychological-, and context related (Table S2). Medical problems concerned for example problems related to the digestive or cardiovascular system, psychological problems could be behavioral or sleep problems, and context-related problems concerned for example problems with work, housing, or social contacts.
The health-related problems identified during initial consultation were extracted by combining information from both the ICPC-2 codes assigned by the ID physician during initial consultation and the clinical entries. The health-related problems mentioned in clinical entries were coded, following a self-developed consensus coding scheme grouping medical-, psychological-, and context-related problems using ATLAS.t.i. software, by three researchers (two ID physicians and the first author; intercoder agreement = 72%). Cases of doubt were discussed with all coders until consensus was reached. The ICPC-2 codes registered by the ID physicians on health-related problems identified during initial consultation were also grouped following the three types and combined with the health-related problems identified in the clinical entries. This resulted in a complete list of health-related problems identified during initial consultation. Additionally, an automated search was performed in ATLAS.t.i. to identify disciplines involved after initial consultation on advice of the ID physician.
Analyses
Analyses were performed separately for the two groups of patients. First, the (number of) different types of reasons for initial consultation were explored using descriptive statistics. Thereafter, we described the reasons that were most prevalent within the three types (medical-, psychological-, and context related). Second, descriptive analyses were performed to explore the (number of) different types of health-related problems identified during initial consultation. To explore a possible pattern between the reasons for initial consultation and the health-related problems identified during initial consultation, a cross-tab analysis was performed for the CV group. Third, to identify the professionals who were involved for referral, assistance, examinations, or treatment after initial consultation, descriptive analyses were performed. IBM SPSS Statistics version 25.0 was used for all statistical analyses.
RESULTS
Demographics
At extraction date, records from 526 patients were available for analysis and were asked for informed consent. A total of 128 patients provided consent and data from their health records were used for this study, with nonresponse to the informed consent being the main reason for exclusion. (Figure 1). The sex and age distribution in this study's population is representative of the total patient population at the outpatient ID practice.
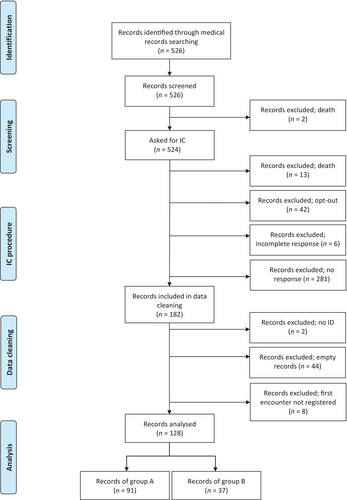
Of the 128 included patients, 91 (71.1%) belonged to the CV group and 37 (28.9%) to the HC group (Figure 1). Table 1 presents descriptive statistics of the study population for the two groups separately. The median age of patients in the CV group was higher than that of patients in the HC group: 25 (IQR: 18–40) versus 17 years (IQR: 7.5–21) years, respectively. In the CV group, 80% were younger than 50 years, with the majority between 18 and 34 years (46.2%). In the HC group, all patients were younger than 50 years at initial consultation, with the majority being younger than 18 (54.1%). Of the patients in the CV group, 34.1% had a known etiological diagnosis, whereas in the HC group the corresponding figure was 89.2%.
| CV group N = 91 | HC group N = 37 | |
|---|---|---|
| Sex, N (%) | ||
| Males | 48 (52.7) | 17 (45.9) |
| Females | 43 (47.3) | 20 (54.1) |
| Age at initial consultation | ||
| Median (interquartile range) | 25 (18–40) | 17 (7.5–21) |
| Age groups at initial consultation, N (%) | ||
| 0–17 years | 21 (23.1) | 20 (54.1) |
| 18–34 years | 42 (46.2) | 16 (43.2) |
| 35–49 years | 10 (11) | 1 (2.7) |
| 50 years or older | 18 (19.8) | 0 |
| Number of consultations during year of initial consultation, N (%) | ||
| 1 | 15 (16.5) | 26 (70.3) |
| 2 | 16 (17.6) | 7 (18.9) |
| 3–4 | 18 (19.7) | 2 (5.4) |
| 5–7 | 18 (19.7) | 1 (2.7) |
| 8–11 | 14 (15.4) | 1 (2.7) |
| ≥12 | 10 (11) | 0 |
| Etiological diagnosis known, N (%) | ||
| Yes | 31 (34.1) | 33 (89.2) |
| No | 60 (65.9) | 4 (10.8) |
Reasons for initial consultation
CV group
The categorization of reasons for initial consultation shows that patients in the CV group most often had a psychological reason for initial consultation (45.1%; Table 2) Regarding psychological reasons for initial consultation, 40% of the referrals concerned behavioral problems. Most found medical reasons were musculoskeletal (21.4%), neurological (17.9%), and digestive (14%). In 22% of the CV group, having an ID was the only reason for initial consultation without an additional question. Of the patients in the CV group, 68.1% had a single type of reason for initial consultation: either medical, psychological, or context related. When multiple types of reasons for initial consultation were present (9.9% of the cases), this always concerned a psychological reason combined with another type of reason for initial consultation.
| Type of reasons, N (%) | N = 91 |
|---|---|
| Psychological reasons | 41 (45.1) |
| Medical reasons | 19 (20.9) |
| Context-related reasons | 2 (2.2) |
| Psychological and medical reasons | 4 (4.4) |
| Psychological- and context-related reasons | 5 (5.5) |
| Unspecified intellectual disability related reasons | 20 (22) |
HC group
The most prevalent reason for initial consultation in the HC group was a health assessment (81.1%). The rest of the HC group had additional reasons for initial consultation during their health assessment appointment: 10.8% had medical reasons, 5.4% had psychological reasons, and 2.7% had context-related reasons.
Health-related problems identified during initial consultation
CV group
Table 3 presents the type of health-related problems identified during initial consultation. For 71.5% of the patients in the CV group, two or three types of health-related problems were identified during initial consultation. This primarily involved medical and psychological problems, in respectively 78.0% and 73.6% of the cases. The most prevalent single type of problems identified during initial consultation was medical problems (17.6%).
| Type of health-related problems identified, N (%) | CV group N = 91 | HC group N = 37 |
|---|---|---|
| Medical-, psychological-, and context-related problems | 27 (29.7) | 1 (2.7) |
| Medical and psychological problems | 23 (25.3) | 12 (32.5) |
| Medical problems | 16 (17.6) | 13 (35.1) |
| Psychological- and context-related problems | 10 (11) | 0 |
| Psychological problems | 7 (7.7) | 4 (10.8) |
| Medical- and context-related problems | 5 (5.5) | 1 (2.7) |
| Unspecified intellectual disability-related problems | 2 (2.2) | 6 (16.2) |
| Context-related problems | 1 (1.1) | 0 |
- Abbreviations: CV, consultation visit; HC, health check.
HC group
Table 3 presents that for 83.8% of the patients in the HC group, medical-, psychological-, and/or context-related problems were identified during the initial consultation. In 45.9% of the patients, this involved a single type of problem. In 72.9% of the patients, medical problems were identified. Psychological problems were identified in 45.9% of the patients. For the remaining 16.2% of the patients in the HC group, no specified health-related problems were identified during initial consultation.
Pattern between reasons for initial consultation and health-related problems identified during this consultation for the CV group
Table 4 contrasts the reasons for initial consultation with the three types of health-related problems identified during initial consultation for the CV group. For 72.6% of the CV patients who visited the outpatient ID practice for one type of reason, additional types of problems were identified during initial consultation. For 83% of the patients with only psychological reasons for initial consultation, additional problems were identified during initial consultation. In contrast, for half of the patients with only medical reasons for initial consultation (52.6%), only medical problems were identified during initial consultation. For the majority of the CV group patients who consulted the practice without a specified reason (90%), medical-, psychological-, and/or context-related problems were identified during initial consultation.
| Health-related problems identified during initial anamnesis, N (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| One type of problem | Two types of problems | Three types of problems | |||||||||
| Med | Psy | Con | Med and psy | Med and con | Con and psy | Con, psy, and med | Unspecified problems | Total | |||
| Reason for initial consultation, N(%) | One type of reason | Med | 10 (52.6) | 0 | 0 | 3 (15.8) | 2 (10.5) | 0 | 4 (21.1) | 0 | 19 (100) |
| Psy | 0 | 7 (17,1) | 0 | 10 (24,4) | 0 | 8 (19,5) | 16 (39) | 0 | 41 (100) | ||
| Con | 0 | 0 | 0 | 0 | 0 | 0 | 2 (100) | 0 | 2 (100) | ||
| Two types of reasons | Med and psy | 0 | 0 | 0 | 4 (100) | 0 | 0 | 0 | 0 | 4 (100) | |
| Con and psy | 0 | 0 | 0 | 0 | 1 (20) | 2 (40) | 2 (40) | 0 | 5 (100) | ||
| Unspecified reasons | 6 (30) | 0 | 1 (5) | 6 (30) | 2 (10) | 0 | 3 (15) | 2 (10) | 20 (100) | ||
| Total | 16 | 7 | 1 | 23 | 5 | 10 | 27 | 2 | 91 | ||
- Abbreviations: Con, context related; med, medical; psy, psychological.
Disciplines involved after initial consultation
The initial consultation led to the involvement of 25 professionals besides the ID physician for referral, assistance or treatment, and examinations (see Table 5). Involvement of disciplines occurred most often for the CV group and often concerned a GP (for 35.2% of the patients), a behavioral expert (34.1%), or a clinical geneticist (28.6%). Within this group, an average of two disciplines is involved per patient after initial consultation at the outpatient ID practice.
| Involved disciplines, N (%) | CV group N = 91 | HC group N = 37 |
|---|---|---|
| General practitioner | 32 (35.2) | 3 (8.1) |
| Behavioral expert/psychologist | 31 (34.1) | 2 (5.4) |
| Clinical geneticist | 26 (28.6) | 6 (16.2) |
| Neurologist | 11 (12.1) | 1 (2.7) |
| Rehabilitation physician | 7 (7.7) | 2 (5.4) |
| ENT doctor | 5 (5.5) | 1 (2.7) |
| Psychiatrist | 5 (5.5) | 0 |
| Speech therapist | 5 (5.5) | 0 |
| Nutritional expert | 5 (5.5) | 0 |
| Eye expert | 4 (4.4) | 3 (8.1) |
| Dentist | 4 (4.4) | 3 (8.1) |
| Pediatrician | 4 (4.4) | 1 (2.7) |
| Internist | 3 (3.3) | 1 (2.7) |
| Gynecologist | 3 (3.3) | 1 (2.7) |
| Orthopedic surgeon | 3 (3.3) | 0 |
| Epileptologist | 3 (3.3) | 0 |
| Physiologist/physiotherapist | 2 (2.2) | 1 (2.7) |
| Sexologist | 2 (2.2) | 0 |
| Gastroenterologist | 1 (1.1) | 1 (2.7) |
| Dermatologist | 1 (1.1) | 1 (2.7) |
| Neuropsychologist | 1 (1.1) | 0 |
| Urologist | 1 (1.1) | 0 |
| Cardiologist | 1 (1.1) | 0 |
| Occupational therapist | 1 (1.1) | 0 |
| Endocrinologist | 0 | 3 (8.1) |
- Abbreviations: CV, consultation visit; HC, health check.
DISCUSSION
This study is the first to explore the characteristics of specialized medical care for people with ID provided at a specialized outpatient ID practice. Results show that (1) patients often initially visit the outpatient ID practice for one type of complaint, most often psychological, (2) diverse, multiple, and interrelated health problems were identified during specialized medical ID consultation, and (3) a range of specialists professionals were involved by the ID physician. This highlights the value of specialized medical ID expertise and indicates a need for multidisciplinary approaches in the healthcare of people with ID.
Interpretation of findings
This study shows that people with ID often experience multiple and multifaceted health problems at the same time. The patient's history and context, in which ID is an underlying factor, play a major role in adequately assessing health problems. It is essential to go beyond medical views and assess health complaints in an integrated way. This includes taking into account the way ID can influence all levels (physical, mental, contextual) of the experienced health issue within the context of everyday life. This is important, because ID, related comorbidities, and the patient's context can influence the expression of symptoms, which can complicate the diagnostic process and treatment of various other medical and psychological problems. These problems might go unnoticed if the focus is on just the ID or on a specific medical or behavioral problem, risking over-, under- or misdiagnosis, and -treatment (Mason & Scior, 2004). Despite the broad focus on medical-, psychological-, and context-related issues, GPs have acknowledged to experience challenges in treating patients with ID (Lennox et al., 2000; Phillips et al., 2004) This study indicates that this is where specialized medical ID expertise, such as provided by ID physicians, can make a difference in improving healthcare for this patient group.
Professionals with specialized medical ID expertise, such as ID physicians, are of value in assessing health complaints in a holistic way, including the specific multimorbidity of people with ID, their context, special medical and psychological care needs, and the etiology of ID (Moonen et al., 2022). This expertise can be seen as complementary to the expertise of the GP. Effective collaboration between both professionals will help improving the healthcare as well as reducing the burden on either profession (Tinselboer et al., 2012). The referral reasons of the CV group indicate that GPs often refer to specialized ID physicians in the case of psychological problems, which frequently concern behavioral problems, suggesting that GPs especially encounter challenges in assessing these problems in people with ID. Dutch GPs are not always aware that they can refer to specialized ID physicians when facing these challenges. Patients were also referred to the outpatient ID practice without specification of a reason other than having ID. This could be because GPs often suspect that ID play a role in patients' health complaints, but do not know in what manner. A qualitative follow-up study can investigate this further.
A possible explanation for the referral reasons being narrower than the problems identified during initial consultation could be that problems are overlooked or “diagnostically overshadowed” by the ID (Beange et al., 1995; Lennox et al., 2007; Mason & Scior, 2004). This concerns the tendency to address symptoms primarily to the ID, which might contribute to missed diagnoses. Misunderstandings on how a person with ID expresses themselves, or reacts to stress, overburdening, and overstimulation might result in incorrect diagnoses as well. Physicians without specialized ID expertise may not always recognize the presence of ID in their patients since this is often not registered, or know the multiple ways in which an ID can influence the presentation of health-related problems. This increases the risk of misdiagnosing complaints and applying diagnostic processes and treatments that are not tailored to the patient with ID (Pouls et al., 2023).
This study identified 25 different healthcare professionals that can be involved in referral, assistance, examinations, or treatment, which indicates a significant need for combined expertise in providing medical care for people with ID (Ervin et al., 2014). This is indicative for the need of multidisciplinary approaches in the healthcare of people with ID (Meijer et al., 2004). The broad range of healthcare professionals that people with ID can encounter makes it imperative that mainstream professionals are equipped with some basic tools and skills to provide effective and compassionate care for this population. Awareness that ID can cause different presentations of health problems, that people with ID have complex medical care needs, and that the expertise of specially trained medical professional is available would help both patients with ID and healthcare professionals. Furthermore, medical professionals should be able to recognize a patient with ID. This can be included in both pre- and postgraduate training for medical and paramedical professionals. Furthermore, teaching medical professionals about how to assess the combination of medical-, psychological-, and context-related problems and how ID can be the underlying interaction in this interplay.
Strengths and limitations
This study used routinely collected data at the outpatient ID practice that was not collected for research purposes specifically. This resulted in two limitations. First, the registration was not fully standardized, leading to missing or inadequately registered data. Second, a GP system was used that did not allow for registration of multiple reasons for consultation and did not include ID-specific codes for registered reasons of consultation. These items were added by the ID physicians in free-text clinical notes and included in our data as described in the Methods section. This allowed us to obtain better insight in consultations and gave a first idea about what specific ID-related codes could be helpful to add in future development of the registration system. The manual coding of clinical entries on health-related problems identified during initial consultation in terms of broader categories (medical-, psychological-, and context-related) limited insights into the specifics of these problems.
The start of the COVID-19 (Coronavirusdisease-19) pandemic challenged obtaining retrospective informed consent, which impacted the number of patients that could be included. Consequently, this study's findings are based on 24.3% of the patients who visited the outpatient ID practice before the extraction date. The sex and age distribution in this study's population is representative of the total patient population at the outpatient ID practice, but limitations in data about the ID population make it difficult to judge the generalizability of our results.
This study has been performed in the Netherlands, and it is important to acknowledge that the findings might not be directly applicable to other countries. Despite this limitation, the Dutch setting provided a unique opportunity to explore the value of specialized medical ID expertise and gave insight in the often multifactorial undiscovered health-related problems that people with ID encounter.
CONCLUSION
This study illustrates the role of specialized ID expertise in medical care for people with ID. Having ID impacts a person's life beyond their health in multiple areas that can in turn affect health as well. Specialized medical ID expertise helps to assess the health problems of people with ID in the broader context of a patient's everyday life. Physicians or nurses specialized in ID can help to adequately assess the combination of medical-, psychological-, and context-related problems that can be easily overlooked in people with ID. Additionally, this study shows that specialized medical ID expertise is of value in organizing multidisciplinary care for people with ID. Examining specialized medical ID consultations provided the opportunity to learn about the complex health-related problems of people with ID.
ACKNOWLEDGMENTS
The authors would like to acknowledge the contribution of patients who have provided informed consent for participation in this research.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
The Medical Ethical Committee (CMO regio Arnhem – Nijmegen) waived the need for further ethical assessment (2020–6090).
PERMISSION TO REPRODUCE MATERIAL FROM OTHER SOURCES
Permission granted.
Open Research
DATA AVAILABILITY STATEMENT
Data (in Dutch) are available upon reasonable request.