Integration is opening the door to a new journey toward oral health value-based care
Abstract
Oral health is a key component of overall health and there is a cost to not including it in the value-based transformation conversation. Health care needs to break down the silos that exist between dentistry and medicine so we can leverage integration to achieve value-based care.
Everyone knows that taking care of your oral hygiene keeps you healthy – or do they? The journey toward good oral health is quite varied for most people and often is dependent upon how oral health is viewed within the continuum of care, how it is managed by providers, and even one's early experiences with dental care. I had an experience as a young boy that shaped my passion for good oral care and made me a strong advocate for the integration of oral health into primary care.
I was visiting my grandparents in New York City and getting ready to go on a trip to Coney Island with my grandfather. That morning my grandmother let me brush my teeth with her, something I did not mind doing but always wanted to get done in a hurry. I was really impressed when I saw her take out her teeth and brush them. I thought, “How convenient is that?” For the next few weeks, I tried over and over to take my teeth out of my mouth to brush them. After repeated failed attempts, I wondered what was wrong with me. I shared my disappointment with my mother, and after giving me a smile only a mother could do, she explained dentures to me. I wondered how anyone could lose their teeth! I decided that was never going to happen to me! It was then that I began to pay attention to my teeth and I still do so to this day. When I was asked to write about oral health as part of value-based care (VBC), I jumped at the opportunity. Arizona's Federally Qualified Health Centers (FQHCs) have been pioneers in VBC on the medical side, but VBC in oral health has yet to be explored and I hope to change that.
I have been in health care since 1978 when I graduated with a nursing degree, thanks to the GI Bill. I was one of three Vietnam veterans in my nursing class but sadly the only one to graduate. We were the first wave of male veterans entering the university's nursing school. I majored in philosophy and picked up nursing in my junior year. It was a good marriage of my curiosity about life and my desire to learn more about health care and ultimately help others. This led to a 42-year career pathway, from delivering clinical care to becoming a quality professional, practice manager and hospital executive, and finally a primary care administrator. With all of the many health care improvement initiatives I have seen over the years, it seems the “person” has gotten lost. We have divided health care around body parts, hence losing an integrated and whole-person care approach. That is what is happening with oral health today – the mouth has been removed from the rest of the body and continues to remain in a silo. But just maybe, a reunification is starting!
It reminds me of what happened with diabetes care in the early 90s. Some of you reading this article might have been part of the collaborative that the Institute for Healthcare Improvement (IHI) started when Don Berwick was the Director. I was fortunate enough to participate in the diabetes collaborative in the late 90s and I learned a great deal about integrating diabetes management into a broader approach to care in hospitals and eventually primary care. For years, the need to better manage patients with diabetes was not well understood or adopted in primary care. It was the job of the endocrinologist to take care of patients with diabetes. However, we learned that good diabetes care must begin with primary care and be integrated with mental health, physical health, and other elements of preventive health like screenings and testing. Diabetes initiatives helped health professionals understand how important prevention and chronic disease management are to minimizing comorbidities and preventable complications while extending one's quality of life. Poorly managed diabetes leads to multiple complications like heart disease, blindness, renal insufficiency, and more. But, if you manage the diabetes patient well, you can significantly decrease complications. It is even possible to help prevent type II diabetes in the first place by becoming more comfortable with talking to patients about lifestyle changes such as weight control.1
We can learn from this parallel and apply it to oral health. Many health professionals may not fully appreciate how addressing the oral health needs of patients with chronic diseases can lead to improved outcomes. As an example, periodontitis can make diabetes management more challenging due to its impact on the body's ability to control blood glucose levels and it can also increase the risk of stroke.2, 3 In one study patients with diabetes and cardiovascular disease who received periodontal therapy experienced a significant reduction (20–40 percent) in cost and hospitalizations.4 Despite what we know about the impact of oral health care on systemic health, medical and dental professionals are educated separately, use completely different language, and usually operate on different electronic health record systems. As a result, primary care has abrogated oral health to the dentist, leaving the door for integrated care nearly closed.
FQHCs, however, recognize the importance of comprehensive, integrated care. Many FQHCs have dental clinics on site along with primary care, behavioral health, pharmacy, and other preventive and wellness services. Unfortunately, there is an insufficient amount of data available to demonstrate the value of this integrated approach to care. As part of FQHC federal grant compliance, all health centers report indicators annually through the Uniform Data System (UDS) – a standardized national database for comparative analysis and to support health center understanding and documentation of VBC. Oral health is not a significant component of UDS and measures related to caries management and the treatment of gingivitis are not incorporated under the landscape of chronic disease management. We need to start putting measurement infrastructure in place to identify quality and cost indicators utilizing a combination of population health data, Medicaid data and peer reviewed quality research studies that will allow us to demonstrate the impact of FQHC dental programs and the oral health services they are providing.
Quality of care is an important component of VBC but cost must also be considered. FQHCs are paid in a unique way compared to other private primary care providers. Congress established the FQHC Prospective Payment System (PPS) in 2001, which allows FQHCs to get paid a flat bundled rate for all Medicaid visits. The PPS helps FQHCs reserve federal grant funds to help offset the cost of serving uninsured patients, rather than subsidizing care for patients on Medicaid. In Arizona, we have done something distinctive by incorporating quality measures into the PPS rate. Three years ago, we started working with our state Medicaid Director to implement an alternative payment methodology (APM) addendum to our state plan for VBC incentives using UDS indicators as performance measures for FQHCs. Based on performance with three mutually agreed upon UDS indicators (see Table 1), FQHCs can increase their PPS rate a total of 1.5 percent annually. This is 0.5 percent for meeting each minimum performance standard (MPS). There was a great deal of discussion around which indicators to use based on cost, quality, minimum performance challenges, and other factors. UDS indicators were ultimately selected because they have associated MPSs and are part of a national standardized reporting system.
| UDS clinical quality measure | MPS |
|---|---|
| Patients with colorectal cancer screening | >65% |
| Patients with diabetes poor control (HbA1c > 9%) | <41% |
| Weight assessment and counseling for nutrition and | >55% |
| physical activity for children and adolescents (ages 3–7) |
Through this new APM, we have engaged all Arizona FQHCs in value-based payment efforts that align with our state Medicaid program's goals for value-based purchasing, including incentivizing outcomes over utilization, prioritizing population health issues, and decreasing costs. The addendum submitted to CMS September 2018 is pending approval, but FQHCs agreed to move forward with the 5-year demonstration project prior to receiving final approval. The pilot went live October 1, 2018.
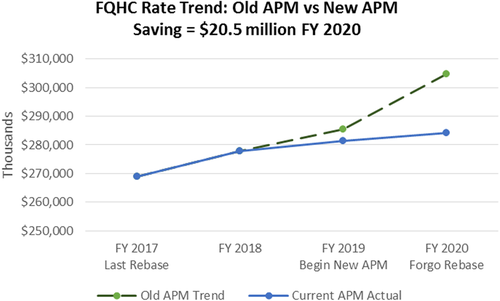
Arizona is one of the first states in the country to use HRSA UDS indicators to set PPS rates. Although FQHCs represent <3 percent of the overall Arizona state Medicaid budget, our ability to bend the cost curve while maintaining or improving quality of care is already evident (see Figure 1).
After the pilot comes to a close, we will evaluate our value-based payment journey by assessing if we did what we set out to do – validate the value of the FQHC model of care. If there is mutual agreement to move forward, another three UDS indicators for measuring value and setting the PPS rates for Arizona's FQHCs will be selected. At that time, our hope is to add oral and behavioral health to the minimum performance indicators so we can measure how those services help reduce overall health care costs and improve patient outcomes. We have yet to determine specific oral health measures that could be included in the APM due to the lack of nationally recognized MPSs within dentistry. Oral health measures that do have MPSs, such as the UDS sealant measure, the Annual Dental Visit HEDIS measure, and CMS eCQM 75v8 may be considered. FQHCs also have the potential to explore several measures that demonstrate the value of integrated care. If diabetic patients receive oral health services, for example, does it result in lower A1C scores? If a pregnant patient receives periodontal care, is there a decreased likelihood of low-birth weight? Next steps are contingent upon CMS's approval of the APM as proposed in Arizona's state Medicaid plan, but we are hopeful about what the future holds for our FQHCs. We need to understand that there is a cost to not integrating oral health into the value-based integrated care model. I am glad that in Arizona, we are on this oral health journey and hope others will follow. It is simply the right thing to do for our patients!