Positioning operations in the dental safety net to enhance value-based care delivery in an integrated health-care setting
Abstract
Objectives
Impact of implementing data-driven performance metric-tracking across a 10-dental center infrastructure established by Family Heath Center of Marshfield (FHC-M) was examined for relative impact on achieving value-based care delivery in serving a patient population characterized by 88% Medicaid representation.
Methods
To track progress toward national benchmarks for preventive care delivery, dental quality analytics dashboard tracking was implemented in real time with sharing of performance metrics across centers. Compliance rate with Uniform Data Systems reporting requirements for sealant placement on permanent first molars in children aged 6-9 years of age at moderate-to-high risk of caries was targeted at FHC-M dental centers for comparison with those of other community health centers statewide and nationally. Hygienist-to-dentist ratio to support robust sealant placement capacity was further examined.
Results
Uniform Data Systems data for rate of sealant placement between 2016-2018 revealed that FHC-M consistently exceeded rates reported statewide and nationally. For this quality indicator, performance across all dental practices in 27 states reported by Centers for Medicare and Medicaid Services in 2018 achieved 23% in 2017 compared to 73% and 52% placement rates reported by FHC-M and community health centers, respectively. A 1:1 hygienist-to-dentist was documented across FHC-M dental centers compared to 0.5:1 reported nationally.
Conclusions
Implementation of quality metric dashboard and a 1:1 dentist-to-hygienist ratio supported realization of value-based dental care delivery relative to caries prevention in a moderate-to-high risk pediatric Medicaid population through achievement of robust sealant placement. Importance of adequate hygienist staffing, "same day" sealant placement and performance feedback supported by technology are highlighted.
Background
Value-based care (VBC) delivery evolved from the Triple Aim initially defined by Institute for Healthcare Improvement in 2007 visualized three goals: improving patient care experience, enhancing population health, and reducing per capita costs of health care delivery.1 In practice, this conceptualization shifts care delivery from the practice of “reactive” medicine in response to disease within a “fee-for-service” environment to the practice of comparatively more cost-effective VBC “preventive medicine.” VBC delivery often incorporates alternative care delivery models that may include integrated care delivery to medically homed patients who become activated partners in achieving health-care goals. Intrinsic aspects of VBC include operationalizing evidence-based, cost-effective, quality-centric care delivery emphasizing preventive care.2 VBC delivery functions optimally in a “health-care learning environment” supported by biomedical informaticians that function nimbly in translating technological advances from the research environment to the clinical arena.
Marshfield Clinic Health Systems (MCHS) is one of the largest private group practices in the United States, and serves an expansive, largely rurally based Wisconsin population through a network of 50 clinics providing health care in 86 specialties, including dentistry. MCHS-owned hospitals, a Healthcare Maintenance Organization and Marshfield Clinic Research Institute (MCRI), its research enterprise, constitute ancillary organizational entities.
Historically, MCHS has functioned as a learning environment, embracing technological support to optimize health-care delivery and has a demonstrated track record in leveraging VBC effectiveness. To achieve seamless integration of its clinics, MCHS pioneered health information technology implementation by physician-led design and implementation of an electronic health record (EHR) in the early 1980s, adoption of a paperless environment, and creation of an enterprise data warehouse to archive all aspects of patient care delivery in real time. MCHS further developed a clinical quality dashboard to track quality care delivery including achievement of preventive care benchmarks.
MCHS emerged as the most successful participant in the Centers for Medicare and Medicaid Services (CMS) Physician Group Practice demonstration project, earning 57 percent of the $107.6 million in gross savings realized over a 5-year period and distributed among the 10 participating institutions based on performance.3 Outcomes of the demonstration project validated the successful integration of managed and preventative care supported by application of informatics and quality tracking to deliver high quality care at reduced cost.
MCHS service areas fall within designated medical and dental health professional shortage areas. Leading up to the year 2000, challenges in gaining dental health-care access escalated for multiple disparity populations and the substantive Medicare and Medicaid-eligible populations living within MCHS's service areas and adjacent Wisconsin counties. Faced with a statewide growing dental care access crisis, State officials approached Family Health Center of Marshfield (FHC-M), a federally qualified community health center (CHC), to identify innovative solutions. FHC-M launched grassroots collaboration with local communities and strategically established a dental safety net infrastructure comprised of 10 dental centers. FHC-M partnered with MCHS to ensure integrated, cross-disciplinary, holistic, VBC delivery across their closely aligned service areas.4 FHC-M dental clinics offer patients access to care irrespective of insurance status or ability to pay. A nominal payment is charged for patients in poverty, and a sliding fee for patients up to twice the poverty level. Further, the research enterprise advanced clinical interoperability by creating and integrating a dental EHR with MCHS's medical EHR.5
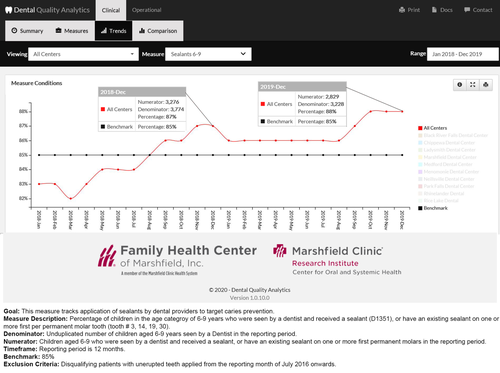
MCHS/FHC-M's Dental Quality Improvement Initiative targeted development of the oral/dental health measures to expand capacity for integrated medical-dental VBC care delivery. MCRI biomedical informaticians pioneered creation of an unprecedented dental quality analytics dashboard (DQAD) emphasizing capacity to track progress towards benchmarks set for preventive dental care delivery. A steering committee comprised of dental providers, operational leaders, researchers, and health IT leaders reviewed oral health quality measures including sealant placement, and caries risk assessment previously defined by the National Network for Oral Health Access and Health Resources and Services Administration (HRSA) and selected metrics for implementation within DQAD. The DQAD web application provides a near real-time visual and analytical platform that assists users in monitoring baseline clinical performance and compares outcomes to a defined benchmark to achieve a defined percentage of performance improvement. Data-driven performance metric-tracking across the 10 dental centers was established and following beta testing and piloting in 2015, DQAD was adopted for quality effectiveness monitoring in 2016. Definitions of trends surrounding key clinical and operational performance measures across each MCHS/FHC-M dental practice were designed to track center and dentist-level performance to systematically communicate relative progress in achievement of benchmarks to the clinical team. These capabilities helped establish FHC-M's dental enterprise as an early adopter of oral health VBC.
Compelling evidence cited >80 percent preventive efficacy following sealant placement over 2 years, with sustained efficacy documented up to 5 years, as supported by systematic review.6, 7 Clinical practice guidelines strongly advocate sealant placement as a cost-effective measure for prevention of caries in school-aged children. Accordingly, FHC-M dental practices prioritized sealant placement to prevent or reduce dental caries risk. As described in this report, FHC-M has consistently exceeded placement rates tallied by CHCs in response to annual HRSA Uniform Data System (UDS) reporting requirements that align with the electronically specified Clinical Quality Measures specified by CMS for children enrolled in Medicaid.8 This practice brief further emphasizes how strategic clinical staffing and informatics-supported quality tracking factored into achieving robust sealant placement in VBC delivery to a disproportionately high representation of Medicaid-eligible patients (4-year mean: 87%) with elevated dental caries risk in the population served by FHC-M.
Methods
Retrospective data analysis
Reports submitted by FHC-M in compliance with HRSA's UDS annual data reporting requirements on sealant placement rates from 1/1/2016 to 12/31/2019 were queried. These data summarized the number of sealant procedures performed on patients aged 6 through 9 years at moderate-to-high risk of caries who met eligibility for sealant placement on their first molar. Patients with unerupted teeth who met age requirements in any given year during the study period with no existent sealants did not meet eligibility requirements and were excluded from the denominator in that year. Determination of first molar eruption was based on tracking of documented presence of the tooth in the tooth chart in the electronic dental record (EDR). Relative performance of the FHC-M's sealant placement rates was further assessed by comparison with annually reported rates achieved by CHCs statewide and nationally.
MCHS's enterprise data warehouse was also retrospectively mined to capture associated demographic data including age, sex, race, and ethnicity of study-eligible children. Eligibility criteria included patients aged 6–9 years whose dental record recorded a Current Dental Terminology (CDT) procedure code: D1351 indicating sealant placement, or EO code, designating an existent sealant, during any of the 4 years across the defined temporal window. FHC-M dental providers routinely conduct dental caries risk assessment using American Dental Association's standardized caries risk assessment tool and document the identified caries risk as one of the three CDTs (low risk = D0601, moderate risk = D0602, and high risk = D0603) within the EDR. The additional criteria for the moderate to high risk for caries for this dental measure were determined based on the dental provider documented CDT codes for moderate risk (D0602) and high risk (D0603) for dental caries within the EDR.
During the defined 4-year study period, sealant procedures were performed by practicing FHC-M dental hygienists or dentists. Total full time equivalent (FTE) for dental hygienists and dentists practicing at point-of-care at each of the 10 FHC-M dental centers during the study period to support robust sealant placement capacity was examined. In each year, the ratio of dental hygienists to dentists across operational FHC-M dental centers was tracked to examine the composition of the dental care delivery team in place to optimize sealant placement during daily clinical care delivery.
Sealant tracking by DQAD
DQAD data surrounding the rate of sealant placement or documentation of an existing sealant on any of the four permanent first molars irrespective of caries risk level, and insurance status of the patients receiving sealants were retrieved for the temporal window 1/1/2016 through 12/3/2019. Granular sealant placement tracking across the 10 FHC-M dental centers during the temporal window was monitored to gauge performance and impact on clinical practice over time.
Results
FHC-M sealant placement performance: UDS reporting outcomes
A total of 5,678 of 7,761 (73 percent; range: 71.1–74.7 percent) qualifying patients 6–9 years of age at moderate to high risk for caries received a sealant on their permanent first molar between 1/1/2016 and 12/30/2019. Table 1 shows the distribution of the subset of patients at moderate-to-high risk for dental caries who met criteria for UDS reporting and who received placement of a sealant on their permanent first molar by FHC-M dental providers, with the majority of placement performed by dental hygienists. Number of patients receiving a sealant are reported in column two under “FHC-M data,” while column one shows the total number of eligible 6–9 year old patients (denominator). The rate of placement achieved at FHC-M dental centers was further compared with available UDS-reported data over a four-year period (see “rate” columns in Table 1).
| Year | FHC-M data | Average FTE | Hygienist:dentist ratio | Reported UDS sealant placement rate* | |||||
|---|---|---|---|---|---|---|---|---|---|
| Total patients with moderate to high risk for dental caries | Total at-risk patients receiving a sealant on their first permanent molar | Dentists | Dental hygienists | FHC-M | National* | FHC-M* | State* | National* | |
| 2016 | 2,121 | 1,508 | 43.00 | 37.28 | 0.87:1 | 2200.4:4475.5 0.49:1 |
71.1% | 57.3% | 42.7% |
| 2017 | 2,156 | 1,611 | 44.90 | 35.70 | 0.80:1 | 2497.9:4882.4 0.51:1 |
74.7% | 60.2% | 50.7% |
| 2018 | 1,875 | 1,373 | 41.00 | 35.27 | 0.86:1 | 2682.8:5099.7. 0.53:1 |
73.2% | 61.8% | 52.8% |
| 2019 | 1,609 | 1,186 | 41.95 | 32.53 | 0.78:1 | Pending | 73.7% | Pending | Pending |
- * Data from Health Resources & Administration (HRSA) Health Center Program 2018 National Health Center Data https://bphc.hrsa.gov/uds/datacenter.aspx (cited 2020 Jun 11).
Workforce composition
The combined annual FTE for dentists and hygienists across all operational dental centers in each of the 4 years are also shown in Table 1 (see “average FTE” columns). The average FTE ratio of hygienist to dentist across the 4 years was 0.83 (range: 0.78–0.87).
Outcome of DQAD tracking and patient characteristics
DQAD-tracked sealant placement rates on any eligible permanent first molar in a 6–9 year old patient documented 3,927(placed)/4,609 (eligible) (85 percent) between 1/1/2016 and 12/31/2016 and 3,674/4,423 (83 percent) between 1/1/2017 and 12/31/2017. Figure 1 provides a screen shot illustrating DQAD quality tracking capability for sealant placement across all of the FHC-M dental centers spanning a two-year window (1/1/2018–12/31/2019). DQAD documented incremental increase in sealant placement in the eligible population over time (Figure 1), capturing rates of 3,327/3,855 (86 percent) between 1/1/2018 and 12/31/2018 and 2,874/3,248 (88 percent) between 1/1 and 12/31/2019. Across all 4 years, DQAD-recorded insurance status at the time of a sealant placement visit in each year showed a consistent average distribution that included: 88 percent Medicaid; 9 percent private insurance and 3 percent either self-pay or sliding fee coverage assisted by safety net funding for qualifying patients who meet federal poverty level definitions. Additional demographic characteristics of the FHC-M population who qualified for, or received, sealants retrieved from the data warehouse documented: 49 percent are female, 88 percent are Caucasian/White and 85 percent were non-Hispanic/Latino.
Discussion
Dental disease remains the number one unmet treatment need of US children despite demonstrated efficacy of sealants in caries prevention and placement cost estimated at only one-third of treatment cost. Median rates of 23 percent in 6–9 year-old children were reported by CMS for the Medicaid/CHIP populations in 20179 and rates of untreated dental caries exceeded 20 percent among 5–11 year-old children.7 Moreover, despite the success of school-based sealant programs, only about 25 percent of US States have adequately instituted these programs in eligible schools.10
UDS-reported data show the national average for sealant placements via the CHC infrastructure tasked with delivering dental care to underserved populations to be more than twice the overall national rate reported by CMS for the Medicaid/CHIP population and well over the Healthy People 2020 target (Table 1). Current study outcomes highlighted robust sealant placement in a population with 88 percent Medicaid representation. Between 2016 through 2019, FHC-M achieved a 73 percent annual average sealant-placement rate in the subset of 6–9 year old patients at moderate to high caries risk qualifying for UDS reporting. By comparison, average national and state rates reported by CHCs between 2016 and 2018 were 49 and 60 percent, respectively. Moreover, DQAD tracking of sealant placement between 2016 and 2019 across the FHC-M dental enterprise on any eligible permanent first molar, irrespective of caries risk in 6–9 year-old patients, averaged 86 percent.
The importance of hygienists to achieving successful sealant placement rates was highlighted. FHC-M dental hygienists, motivated to practice preventive care delivery in a supportive environment characterized by consistency in workflow, largely accomplished sealant placement. Hygienist:dentist ratio across FHC-C dental centers between 2016 and 2019 averaged 0.8:1.0 compared to 0.51:1 reported nationally by CHCs between 2016 and 2018 (Table 1). Engagement of the entire clinical team supported sealant placement by hygienists as documented by an 89 percent sealant placement rate in eligible patients during scheduled preventive care visits supported by proactive emphasis on “same-day placement” for appointed patients. Routine DQAD data reportedly engender “friendly competition” among hygienists across dental centers, who embrace the mission-driven “patient first” perspective, with emphasis on prevention to achieve VBC delivery.
This practice briefly documented the achievability of high rates of sealant placement in Medicaid populations in a CHC setting, contributing to VBC delivery and defined convergent elements that substantively contributed to high rates of sealant placement. Convergent elements included: an adequate motivated hygienist:dentist ratio practicing in a supportive environment; technological support including a dental EHR and quality tracking to provide performance feedback; and strong commitment to preventive care delivery to underserved populations.
Acknowledgments
This study was supported by funding from the Marshfield Clinic Research Institute, Family Health Center of Marshfield, Health Resources and Services Administration (HRSA), and Delta Dental of Wisconsin in establishing DQAD capability. The authors also acknowledge assistance from Mary Dorsch, Director of Operations, Family Health Center of Marshfield, in provision of USD reporting data, Harshad Hegde, Informatics Research Architect, Center for Oral and Systemic Health, at Marshfield Clinic Research Institute, for assistance with analysis and summary of DQAD data and Tena Springer, FHC-M Dental Division Administrator, for assistance with administrative data retrieval.