Minor painful procedures in extremely preterm infants admitted to a tertiary neonatal intensive care unit: Opportunities to improve pain mitigation
Conflict of interest: None declared.
Abstract
Aim
This study aims to characterise current pain management practices in extremely preterm infants (gestational age less than or equal to 28 weeks) admitted to neonatal intensive care unit (NICU).
Methods
Retrospective audit pertaining to patient characteristics, as well as minor painful procedures (MPP), pain mitigation and pain scoring in 25 extremely preterm infants admitted to a tertiary NICU in 2016 over the first 14 days of NICU admission. Opportunities to bundle MPP were identified according to pre-specified criteria. Bayley Scales of Infant Development, Third Edition (BSID-III) cognitive, language and motor composite scores were available from the neurodevelopmental follow-up clinic at 12- and 24-months of corrected age. Linear mixed methods regression was used to examine for correlation between increased exposure to MPP and BSID-III scores at follow-up.
Results
Extremely preterm infants underwent an average of 11.24 ± 4.12 MPP per day for the first 14 days of NICU admission. Opportunities to bundle MPP were missed 75.98% (408/537) of the time; most of these were invasive blood collections. A total of 12.2% (481/3933) of MPP occurred within 4 h of pharmacological or non-pharmacological pain mitigation. BSID-III motor composite score was associated with an 11.75 (95% confidence interval 1.99, 21.27) decrease in patients experiencing more than or equal to the third quartile of MPP in the 14 days post-NICU admission (P = 0.0329, n = 42). Association was not found for BSID-III cognitive and language composite scores.
Conclusions
There is readily scope for quality improvement initiatives to reduce harm in extremely preterm infants admitted to NICU.
What is already known on this topic
- Preterm infants are routinely exposed to painful procedures in NICU.
- Non-pharmacological pain mitigation, such as swaddling, kangaroo care and sucrose administration are efficacious in this setting.
What this paper adds
- Extremely preterm infants are routinely exposed to painful procedures in NICU.
- There is readily potential to bundle minor painful procedures together in order to reduce harm in this vulnerable population.
- Increased exposure to minor painful procedures is associated with decreased BSID-III motor composite score in extremely preterm infants at 12- and 24-month follow-up.
In the neonatal intensive care unit (NICU), infants undergo a large number of painful procedures as part of their routine care. A recent systematic review identified that the typical NICU patient experiences 7.5–17.3 invasive procedures per day for the first 2 weeks of admission, noting the most frequent procedures as heel lance, suctioning and venepuncture.1 These are relatively minor procedures and thus the pain elicited can be appropriately managed without the use of pharmacological intervention. In 2001, an evidence-based consensus statement was developed which recommends methods such as oral sucrose, swaddling and skin-to-skin care can be used alongside or after such procedures.2 At a similar time, the analgesic effects of breastfeeding were also reported in the context of reducing procedural pain.3 In the years since, numerous clinical trials and associated systematic reviews have demonstrated the efficacy of these interventions in reducing pain associated with minor procedures in neonates.4-7 It is concerning that, despite access to methods which reduce procedural pain in neonates, procedures such as heel lance, suctioning and venepuncture were met with pain mitigation in less than 50% of instances in some studies.8, 9
Efforts to reduce neonatal pain are driven not only by the principal of ‘first do no harm’. There is also concern that frequent exposure to pain may be associated with neurological sequelae in this vulnerable population. In a previous critical study, a greater number of invasive procedures experienced by infants at 24–32 weeks gestational age (GA) was associated with reduced MRI-defined white matter maturation and reduced IQ at 7.6-year median follow-up after controlling for clinical confounders.10 A more recent study characterised this further, showing associations between procedural pain in NICU and aberrant development of somatosensory regions of the brain.11 Overall, a large body of work supports the hypothesis that recurrent exposure to pain in the neonatal period may contribute to suboptimal neurodevelopmental outcomes in later life.12-14
While it is known that vulnerability to neurological insults correlates inversely with GA, there is a relative paucity of research addressing the experience of extremely preterm infants in this context. In line with this, we report the characteristics of extremely preterm infants at a tertiary level III NICU, their exposure to painful procedures, pain mitigation undertaken and their neurodevelopmental outcomes at 12- and 24-month follow-up.
Methods
Study cohort and data collection
The present study is based on the retrospective audit of medical records pertaining to extremely preterm infants (GA less than or equal to 28 weeks) admitted to a tertiary NICU in Canberra, Australia during 2016. Infants admitted to NICU more than 24 h after their birth were excluded. Demographics and diagnostic data were extracted from the Neonatal Intensive Care Unit Study database. Minor painful procedures (MPP) (such as venepuncture, oral/nasal or tracheal suctioning, continuous positive airway pressure (CPAP) or non-invasive neurally adjusted ventilation (NIV-NAVA) care events, invasive blood collections, etc.) and pain scoring with the Premature Infant Pain Profile – Revised, as well as pharmacological and non-pharmacological pain mitigation were collected in individual detail from the medical records. Data pertaining to neurodevelopmental follow-up at 12- and 24-months were available from departmental records. Neurodevelopmental follow-up clinics involved scoring by the Bayley Scales of Infant Development, Third Edition (BSID-III). The BSID-III cognitive, language and motor composite scores were available for use in this study.
Proximity of minor painful procedures, pain mitigation and pain scoring
Association of MPP with pain mitigation and pain scores used ‘best-case-scenario’ logic. For example, care events noted in the charts alike ‘cuddles’, although not specified as kangaroo care or swaddling, were regarded as non-pharmacological pain mitigation. The time between MPP and pain mitigation or pain scoring was measured in minutes. MPP were regarded as being associated with pain scoring or pain mitigation if they occurred within 4 h of each other.
Classifying opportunities to bundle minor painful procedures
In an ideal setting, MPP are bundled to reduce frequency of exposure to pain as well as improve their coverage with pain mitigation and the utility of pain scoring. The date and time of each MPP were used to identify opportunities to bundle MPP. An opportunity to bundle MPP was defined as any MPP that was not a CPAP or NIV-NAVA care event or a suction event. An opportunity to bundle MPP was considered missed if it was the only procedure documented at the hourly charting interval and the next closest procedure or group of procedures (including CPAP or NIV-NAVA care events and suction events) occurred within 2 h.
Modelling predictors of adverse neurodevelopmental outcome
Linear mixed effects regression models using maximum likelihood estimation were used as a first-look approach to examine if frequent exposure to MPP is predictive of BSID-III cognitive, language and motor composite scores at 12- and 24-months follow-up. Models assessed whether the patient experiencing more than or equal to the third quartile of MPP in the first 14 days of NICU admission predicted variation in composite score. Each model was then compared to a base model fitted without predictors. Models were considered eligible for reporting if they showed significant improvement over the base model according to ANOVA. All models controlled for GA and birthweight (BW). Patients were modelled as random effects, whilst candidate predictors and controls were modelled as fixed effects.
Statistical analysis
Categorical data are reported as frequency. Continuous data are reported as mean ± standard deviation unless the underlying distribution was non-normal, in which case median (interquartile range) was reported. This study utilised an alpha threshold for statistical significance at P < 0.05. Study data were prepared and analysed using R for Statistical Computing version 4.0.0 (www.r-project.org) and the lme4 package for mixed-effects models (http://www.cran.r-project.org/web/packages/lme4). The present study was approved by the Human Research and Ethics Committees at The Canberra Hospital (2020/ETH00344) and the Australian National University (2020/632)
Results
Cohort characteristics
Twenty-five extremely preterm infants were admitted to NICU within 1 day of birth in 2016. Table 1 summarises the demographic and clinical characteristics of the patients under study. GA ranged from 24 to 28 weeks with a mean of 26.44 ± 1.36 weeks. BW ranged from 540 to 1370 g with a mean of 981.40 ± 201.57 g. 52% (13/25) of infants underwent endotracheal intubation in the delivery room and 48% (12/25) infants were diagnosed with bronchopulmonary dysplasia. A total of 4% (1/25) of patients were diagnosed with severe intraventricular haemorrhage and no patients were diagnosed with necrotising enterocolitis. The average NICU length of stay was 87.28 ± 38.46 days and all patients were admitted for more than 14 days. A total of 350 patient-days were included in the present analysis.
| Summary | Statistic |
|---|---|
| Patients, n | 25 |
| Male sex, n (%) | 18 (72) |
| Gestational age (weeks), mean (SD) | 26.44 (1.36) |
| Birthweight (g), mean (SD) | 981.40 (201.57) |
| APGAR score, median (IQR) | |
| At 1 min | 3 (2.75–5) |
| At 5 min | 6 (5.75–7.25) |
| At 10 min | 8 (7–8.5) |
| Endotracheal intubation in delivery room, n (%) | 13 (52) |
| Diagnoses (during NICU admission), n (%) | |
| BPD | 12 (48) |
| NEC | 0 (0) |
| Gastrointestinal perforation | 0 (0) |
| IVH highest grade, n (%) | |
| No IVH | 17 (68) |
| Grade 1 | 5 (20) |
| Grade 2 | 2 (8) |
| Grade 3 | 0 (0) |
| Grade 4 | 1 (4) |
| NICU admission length of stay (days) | 87.28 (38.46) |
- BPD, bronchopulmonary dysplasia; IQR, interquartile range; IVH, intraventricular haemorrhage; NEC, necrotising enterocolitis; SD, standard deviation.
Frequency of minor painful procedures
In the first 14 days of NICU admission, extremely preterm infants underwent 157.32 ± 29.10 MPP. Table 2 indicates the types of MPP infants underwent on average per day of admission during this period. Specifically, infants underwent on average 11.24 ± 4.12 MPP per day in the first 14 days of admission. The most common MPP were endotracheal and oropharyngeal suction events, CPAP and NIV-NAVA care events, and invasive blood collections (Table 2). The average number of MPP undertaken is broadly consistent in each of the first 14 days from NICU admission (Fig. S1, Supporting Information). Exception to this was the first day of admission, during which infants underwent the most MPP (averaging 13.72 ± 3.81 MPP). The average number of MPP varied greatly across the time of day (Fig. S2, Supporting Information). Specifically, MPP tended to occur 2-10fold more frequently per patient during or near 00:00, 06:00, 12:00 and 1800 hours, coinciding with planned nursing cares.
| MPP per patient per day, over first 14 days of NICU admission | Mean (SD) (n = 25) |
|---|---|
| Overall | 11.24 (4.12) |
| Suction events | 7.03 (3.47) |
| CPAP and NIV-NAVA care events | 3.15 (1.00) |
| Invasive blood collections (i.e. those excluding presence of arterial lines) | 2.10 (1.58) |
| Painful drug administration (injection and per rectum) | 1.40 (0.49) |
| Line insertion and removal (excluding umbilical lines) | 1.18 (0.47) |
| Others† | 2.10 (1.00) |
- † Others include intubation and extubation, as well as nasopharyngeal and oropharyngeal tube placement and more.
- CPAP, continuous positive airway pressure; NIV-NAVA, non-invasive neurally adjusted ventilatory assist.
Opportunities to bundle minor painful procedures
A total of 537 opportunities to bundle MPP were identified. Of these, 76.0% (408/537) opportunities to bundle were considered missed (as they had not occurred within 2 h of another MPP). Indeed extremely preterm infants experienced 4.3 ± 2.32 h between MPP or groups thereof. Figure 1 shows missed versus not missed opportunities to bundle by the MPP procedure type. Invasive blood collection events presented the most missed opportunities to bundle for any of the eligible MPP procedure types (Fig. 1). Each infant in the present study experienced more missed opportunities to bundle MPP than those which were not missed (Fig. S3, Supporting Information). Almost each hour of the day experienced on average more missed opportunities to bundle MPP than those which were not missed (Fig. S4, Supporting Information).
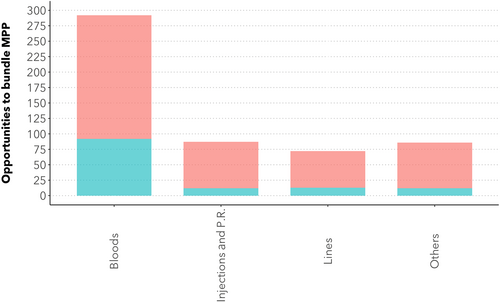
 ), Missed; (
), Missed; ( ), not missed.
), not missed.Frequency of pain mitigation for minor painful procedures
In the 350 patient-days studied, four patients received one to two administrations of morphine each, one patient received 20 administrations of paracetamol and another patient received a single administration of paracetamol. A total of 3.6% (144/3933) total MPP occurred within 4 h of pharmacological pain mitigation in the patient-days studied. No evidence of sucrose administration was observed in the patient records. Non-pharmacological pain mitigation events were documented in the form of kangaroo care (26 instances) or swaddle (one instance). Furthermore, some care events were documented generically as cuddling (94 instances). Including kangaroo care, swaddle and cuddle events, extremely preterm infants were documented as undergoing on average 5.04 ± 3.16 non-pharmacological pain mitigation events in their first 14 days of NICU admission. A total of 8.7% (342/3933) total MPP occurred within 4 h of documented non-pharmacological pain mitigation. Overall, 12.2% (481/3933) of MPP occurred within 4 h of pharmacological pain mitigation, non-pharmacological pain mitigation or cuddling. Pain scores were documented 111 times in 48% (12/25) patients, although rarely were documented over consecutive timespans. A total of 9.9% (385/3933) total MPP occurred within 4 h of documented pain score.
Neurodevelopmental outcomes
Data from neurodevelopmental assessment were available for all 25 patients at 12 months corrected age and for 21 patients at 24 months corrected age. Table 3 shows BSID-III cognitive, language and motor composite scores at 12- and 24-months. Figure 2 indicates BSID-III composite score outcomes at 12- and 24-month follow-up relative to the number of MPP experienced. MPP was predictive of BSID-III motor composite score. Motor composite score was associated with an 11.75 (95% confidence interval 1.99, 21.27) decrease in patients experiencing more than or equal to the third quartile of MPP in the 14 days post-NICU admission (P = 0.0329, n = 42). MPP quartile was not predictive of BSID-III cognitive and language composite scores.
| Neurodevelopmental outcome | Mean (SD) |
|---|---|
| BSID-III cognitive composite score | |
| At 12 months corrected age | 98.48 (14.42) |
| At 24 months corrected age (n = 21) | 95.48 (13.87) |
| BSID-III language composite score | |
| At 12 months corrected age (n = 22) | 98.77 (11.92) |
| At 24 months corrected age (n = 20) | 89.00 (14.38) |
| BSID-III motor composite score | |
| At 12 months corrected age | 91.17 (12.60) |
| At 24 months corrected age | 90.16 (11.62) |
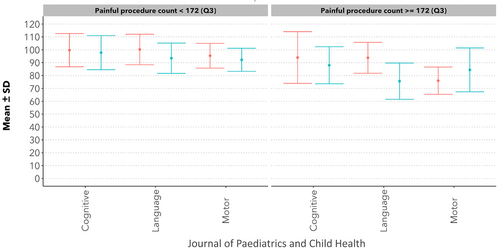
 ), 12-month follow-up; (
), 12-month follow-up; ( ), 24-month follow-up.
), 24-month follow-up.Discussion
MPP were frequent in extremely preterm infants admitted to NICU in 2016. Infants underwent an average of 11.24 ± 4.12 MPP per day in the first 14 days of admission, consistent with the findings of other NICUs in past years.1
Despite their frequency, MPP undertaken in extremely preterm infants were usually not associated with documented pain mitigation. Pharmacological pain mitigation was associated with 3.6% of MPP, which is understandable given non-pharmacological pain mitigation is preferred for MPP. Nonetheless, rescheduling of some MPP to co-occur with pharmacological pain mitigation indicated for other reasons may comprise a poriton of quality improvement initiatives in this space. Non-pharmacological pain mitigation was associated with 8.7% of MPP. While overlap between MPP and any pain mitigation is lower than reported in previous studies,8, 9 it is possible that non-pharmacological pain mitigation occurred more often than was documented. In particular, the use of sucrose for pain mitigation was not documented in these patients despite our anecdotal understanding that it was in use during this time. Although the low overlap between MPP and pain mitigation is despite the highly lenient matching criteria of 4 h in either direction, the suspected limitation of incomplete documentation confounds this component of the study results.
A unique analysis in this study is around opportunities to bundle MPP, an initiative which remains beneficial even in the ideal setting in which all MPP are accompanied by pain mitigation. Opportunities to bundle MPP were missed 75.98% of the time during the first 14 days of NICU admission in extremely preterm infants. Results of this study characterising missed opportunities to bundle MPP highlight this as an exciting opportunity for quality improvement initiatives: opportunities to bundle MPP were missed more often than not missed in all patients, across all eligible procedures, and in almost all hours of the day. MPP also tended to occur across all patients at or near 00:00, 06:00, 12:00 and 18:00 hours, corresponding with planed care times across the NICU, suggesting that rescheduling MPP which were planned outside of these times may naturally lead to improved bundling.
Analysis was also undertaken to identify possible link between increased exposure to MPP and neurodevelopmental outcomes in extremely preterm infants. In this study, increased exposure to MPP was associated with an 11.75 point decrease in BSID-III motor composite score after controlling for GA and BW. This is despite that the study was not planned or powered to find clinically relevant effect size whilst controlling for relevant confounders. For this reason, a definitive association cannot be claimed, and this analysis can be seen as a first-look at possible neurodevelopmental implications of MPP extremely preterm infants.
Conclusions
Overall, we have characterised MPP and their relation to pain mitigation and pain scoring in extremely preterm infants. There exists strong need to improve documentation and use of non-pharmacological pain mitigation in these patients. There is also readily potential for quality improvement initiatives to improve bundling of MPP and thereby reduce harm in this highly vulnerable population. It is possible that reducing exposure to MPP will have beneficial impact on neurodevelopmental outcomes, and such studies should monitor this closely.
Acknowledgement
Open access publishing facilitated by Australian National University, as part of the Wiley - Australian National University agreement via the Council of Australian University Librarians.




