Do Neighborhoods Matter for Individual Decision-Making? The Case of COVID-19 Vaccination in Sweden
ABSTRACT
Much research has highlighted the significance of neighborhood effects on individual-level choices and outcomes. But it has proven difficult to disentangle the influence of those that an individual shares a residential space with from that of other peers, such as work colleagues and family members. Neighbors, work colleagues, and family members constitute different sources of information. The decision to accept or refuse a vaccine is intensely personal and involves the processing of information about phenomena likely to be unfamiliar to most individuals. To examine the information effect of different peer groups we use microlevel data on COVID-19 vaccination in Sweden. We investigate the extent to which an individual's decision not to get vaccinated is influenced by the presence of other unvaccinated individuals in their household, workplace, or residential neighborhood. Our findings reveal that workplace peers tend to be most strongly connected to the decision not to get vaccinated. We also find that the role of neighborhood peers tends to be overestimated when we do not control for peers at home and at work.
1 Introduction
Most decisions made by individuals are not made in isolation. Human beings gather information from various sources, such as news outlets and social media, friends, family members, neighbors, and colleagues; codified knowledge, recent research, previous experiences, and belief systems are all tapped when making choices. The decision-making process thus involves multiple sources of information connecting the various communities in which individuals are embedded. Different research strands in the social sciences, of varying vintages, have examined how individual decision-making and individual-level outcomes are influenced by interactions with others.
Economists have long understood that social interactions—what Becker termed the “social environment” (Becker 1974)—can shape many aspects of economic activity, including migration, job matching, investment behavior, valuation of goods, product adoption decisions, and learning-by-doing (Simon 1983; Manski 2000; Becker and Murphy 2003). Renewed interest in the economic effects of social interactions, advances in the mathematics of networks, refinements on the social networks, and the increasing availability of data recording interactions among individuals have all combined to make the study of social interactions central to economic inquiry (Durlauf and Ioannides 2010; Ioannides and Soetevent 2007; Jackson 2008; Cabrales et al. 2011; Bailey et al. 2018, 2022).
The behaviors and choices of individuals are influenced by those of their peers, that is, members of social groups with similar interests, experiences, education, or social statuses. Members of a peer group are more likely to influence a person's beliefs, attitudes, values, and behaviors to conform to the influencing group or individual. These types of interactions have captured the attention of social scientists. Educational, labor market, and health outcomes have been shown to be affected by individuals following their peers by changing their attitudes, values, or behaviors (Coleman 1968; Calvó-Armengol et al. 2009; Mas and Moretti 2009; Van Veldhuizen et al. 2018; Epple and Romano 2011; Oakes et al. 2015; Bailey et al. 2022). Another type of social interaction that has received much attention are neighborhood effects—the effects on an individual's decisions, behaviors, and outcomes of the socioeconomical and behavioral traits of those she shares a residential space with (Kain 1968; Dietz 2002; Sampson et al. 2002; Durlauf 2004; Kling et al. 2007; Roosa and White 2014; Arcaya et al. 2016; Rotger and Galster 2019; Candipan 2019; Vandecasteele and Fasang 2021).
Neighborhood effects encompass not only outcomes but also decisions or choices made by individuals via role models, peer group influences, and imitative behavior (Piraveenan et al. 2021). Although there is now a large body of empirical research on neighborhood effects, we still know relatively little about the causal mechanisms responsible for relationships between neighborhood attributes and individual outcomes (Galster 2012). Due to spatial sorting, the causality of neighborhood effects on labor market outcomes is debated in the literature (see, e.g., Bolster et al. 2007; Ioannides and Topa 2010; Graham 2018). The existence of spatial sorting means that individuals self-select into different types of areas based on their preferences and characteristics, including their labor market outcomes as these determine what type of neighborhood individuals can (afford to) reside in (cf. van Ham and Manley 2010; Sager 2012; Clark et al. 2022). In addition to residential spaces, social interactions occur in the myriads of social environments in which individuals spend substantial portions of their waking hours outside of their homes or residential environments (Wickes et al. 2019; Cagney et al. 2020).
In summary, the behavior, and choices, and consequently, outcomes, of individuals occur in social settings, where the behavior, choices, and outcomes of others spill over to all members of the peer group(s). Peer effects can be due to social pressure to act in a certain way, and/or knowledge spillovers providing new and relevant information for improved decision-making. An individual's peer groups can, for example, be formed by coworkers in the context of the workplace, the neighbors in the context of the neighborhood, as well as family members in the context of the household. At a very abstract level, we can think of social interactions as taking place within a “social space,” defined by one's reference group—be it one's classmates, peers, neighbors, or colleagues (Topa and Zenou 2015). These social spaces are also spatial spaces and very often urban spaces (Sato and Zenou 2015). A central feature in many models of urban economics is that a dense concentration of people facilitates social interactions and thereby benefits learning and productivity (Durlauf 2004). But how to disentangle the influence of family members, peers, neighbors, and coworkers on individuals' decision-making?
Much of the prior research has focused on the influence of neighborhoods as peer groups, with fewer studies exploring the combined impact of neighborhoods alongside the influence of households and workplaces as crucial peer environments (Klaesson et al. 2023). This disparity in emphasis is likely due to limited data accessibility, as analyzing these factors necessitates microlevel data that maps the broader social landscape encompassing neighborhoods, families, and workplaces for individuals. If we recognize the significance of all three social environments but solely rely on commonly available neighborhood-level data, there is a potential risk of overestimating the role of neighborhoods as influential social arenas in decision-making. This oversight could occur due to the omission of variables associated with family and workplace characteristics. The present discussion considers the effects of different peer groups by focusing on a consequential health outcome: whether to get COVID-19 vaccinated or not. This decision is anticipated to be influenced by interconnected neighborhood effects, peer pressure, and social networks.
Our aim is to advance the analysis by incorporating both family and workplace peers into the decision-making context, alongside the neighborhood level. What is the relative importance of three very salient peer groups—family, neighbors, coworkers—in influencing the choice to get vaccinated? More specifically, our study examines the multilevel influences using the COVID-19 vaccination as an example. To what extent was an individual's choice to refrain from vaccination impacted by having other unvaccinated individuals in their household, workplace, and immediate neighborhood. Further, we aim to examine the degree to which the decision of not getting vaccinated is influenced by the vaccination status of those in close proximity, and to what extent the role of the neighborhood may be overestimated if family and workplace are not integrated into the model.
While we recognize that the COVID-19 pandemic was an unusual and unique event, the health crisis created a lot of urgency and pressure for people to make quick decisions, especially regarding vaccinations. However, we believe that the vaccination decision is still a useful example for studying peer group influence. Individuals had to make a very consequential decision in an environment that was rich with novel and often conflicting information. Even though the situation was exceptional, people likely talked with their family, neighbors, and colleagues before deciding whether to get vaccinated. This makes it a strong case to explore how social interactions influence important choices.
To be able to answer this question data is needed that makes it possible to link an individual's decisions with the specific characteristics and behaviors of those with whom she interacts and who constitute her neighborhood and social groups. Detailed Swedish microlevel data allow us to both capture the characteristics of an individual, including whether the individual received a COVID-19 vaccine, and who constitute her family, workplace, and residential neighborhood peers.
Results from prior research indicate that neighborhood social settings have played a crucial role in determining health outcomes (Oakes et al. 2015). While COVID-19 infection disproportionately affected disadvantaged neighborhoods, these neighborhoods also lagged in COVID-19 vaccinations (Sacarny and Daw 2021; Barry 2021; Corallo et al. 2021; Sun and Monnat 2022; Rich et al. 2022). Additionally, neighborhoods tend to play a more significant role as a peer group among low-skilled individuals in the decision to get vaccinated (Klaesson et al. 2023). Social network exposure to COVID-19 cases shaped individuals' beliefs and behaviors concerning the coronavirus (Bailey et al. 2022; Kuchler et al. 2020).
Our research findings indicate that individuals' decisions not to get vaccinated are most significantly associated with influences from their workplace peers and family peers, while neighbors play a relatively marginal (although still significant) role. These peer groups differ from each other in many ways, including their spatial setting. Additionally, we observe that the influence attributed to neighborhood peers tends to be overestimated when we do not account for the influence of peers both at home and in the workplace.
2 Methods and Data
2.1 Social and Spatial Setting
We regard an individual's stance on vaccination as an unobservable, latent variable. This variable can be seen as the individual's perceived overall gain or loss from receiving a vaccine injection. This perceived gain or loss is calculated as the sum of all psychological benefits minus the sum of all psychological costs associated with getting vaccinated—a benefit and cost at least partly influenced by the peers. Because the overall gain or loss cannot be directly observed, we label it as a latent variable. However, what we can observe is the choice an individual makes regarding vaccination, and we posit that this choice is influenced by peer groups stemming from the individual's family members, colleagues, and neighbors.
It can be argued that individuals are sorted across neighborhoods, and choosing partners and workplaces, based on fundamental beliefs and values, which may be correlated with vaccine hesitancy in general. Vaccine hesitancy has also been shown to be strongly correlated with education and income (Hudson and Montelpare 2021), which work as sorting factors. Even though these factors, and general vaccine hesitancy, are correlated also with reluctance regarding COVID-19 vaccination (Khubchandani et al. 2021), Troiano and Nardi (2021) find that the most common reasons for not accepting the COVID-19 vaccine include concerns about safety due to perceived dangers about a vaccine produced in a hurry, finding the vaccine unnecessary due to COVID-19 being a harmless disease and/or due to believing to be already immune, and doubting the efficiency of the vaccine. Similarly, an extensive survey conducted by The Public Health Agency of Sweden (2021) revealed that skepticism toward the COVID-19 vaccine was largely driven by concerns about side effects and uncertainty regarding the safety of the vaccine, especially due to the new messenger RNA technology. Other reasons included distrust of authorities, the belief that natural immunity provided sufficient protection, and the perception by some individuals that the vaccination program infringed upon personal rights and freedom of choice.
These fears, beliefs, and factors are likely to be specific for the COVID-19 vaccine, due to the novelty and quick uprise of both the virus and the vaccine production, and thus not correlated with resistance against long-term researched vaccines for well-known and long-standing diseases. Furthermore, it is important to note that Sweden may differ slightly from other countries in the context of COVID-19 vaccinations, as they were not mandatory, and vaccine passports were only required for international travel. For comparison, Sweden has a voluntary vaccination program for children, which includes vaccines such as polio, measles–mumps–rubella (MMR), human papillomavirus (HPV), rotavirus, pneumococcal infections, and Vaccine against diphtheria, tetanus, and pertussis, with a coverage rate of approximately 93%–94% (The Public Health Agency of Sweden 2024). This reflects a strong underlying acceptance of vaccinations among Swedes, particularly for well-established vaccines.1
Hence, it is unlikely that individuals have engaged in spatial sorting based on their attitudes toward COVID-19 vaccination in particular, and there is a high likelihood that such attitudes did not influence individuals' choices regarding residence, employment, or family/partner selection. Stated differently, it is highly likely that the COVID-19 vaccination status has not exerted a discernible influence on the composition of an individual's peer groups at the time when the vaccination decision was made.
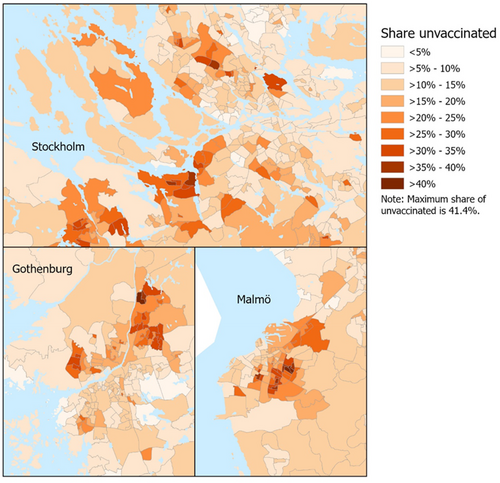
Figure 1 presents a map of neighborhoods in the country's three largest cities—Stockholm, Gothenburg, and Malmö. The map illustrates that vaccination uptake does indeed vary across space, with some neighborhoods being more likely to vaccinate than others. This may be due to neighborhood effects and/or spatial sorting based on individual characteristics, such as ethnic background, education, income, and other socioeconomic variables. These factors influence our choice of residential neighborhood (spatial sorting) at the same time as they may play a role in the decision to get vaccinated. To alleviate issues of sorting, we control for several ethnic and socioeconomic individual characteristics.
2.2 Model and Estimation Strategy
If an individual's stance regarding COVID-19 vaccination is largely uncorrelated to her sorting across households, workplaces, and neighborhoods, as we argue above, we can at least approach causal estimates of these three sources of peer effects on the decisions to vaccinate (or not). At the same time, the decision to vaccinate is likely to be influenced by individual characteristics, such as age, civil status, ethnic background, education, occupation, and income, also including housing characteristics, as well as geographical characteristics, such as the type of municipality of residence. We expect age to influence the choice of vaccination since older individuals were/are more at risk of severe infection and death from COVID-19. Ethnic background is likely to play a proxy role due to language, cultural, and social barriers that may lead to a lack of information regarding, for example, the individual and social benefits of the vaccine. There may also exist mistrust toward Swedish institutions within certain ethnic groups. We expect more educated and higher-income individuals in more advanced occupations to show less vaccine hesitancy due to the increased probability of making more informed choices and having higher trust in science and experts. We also expect that individuals in some family arrangements (married and/or having children) will be more likely to get vaccinated to avoid spreading the virus to close family members.
Several of the above-mentioned variables are connected to an individual's socioeconomic status, as are variables regarding one's housing situation. Individuals in rental apartments, which is typically the cheapest housing option since it does not require a capital investment, are thus expected to show greater vaccine hesitancy. The expected effect regarding intergenerational and crowded households is, however, ambiguous. On the one hand, we would expect a greater vaccine acceptance to not spread the virus to (older) family members. On the other hand, households with these characteristics tend to be socioeconomically disadvantaged in the Swedish context, pointing us to expect greater vaccine hesitancy.
The primary question of concern for this paper is to what extent potential peers at the family, workplace, and neighborhood levels play a significant role in this decision-making, and for this purpose, we employ a binary logit regression analysis. We thus estimate the probability of not getting vaccinated versus getting vaccinated. More specifically, we want to investigate the relative importance of neighbors, as compared with family members and coworkers. Even though we expect all three information communities to matter for the vaccine decision of individuals, we posit that the inclusion of family and peers at work downplays the neighborhood effects due to stronger (cognitive) connections within the family and within the workplace than within one's neighborhood. We thus expect the spatial aspect to play a more marginal role when it comes to an important, possibly life-changing decision that had to be taken within a relatively short time frame.
2.3 Data
To investigate the influence of peer groups—family, colleagues, and neighbors—in the decision-making in getting the COVID-19 vaccine, we use individual-level vaccination data from the Swedish National Vaccination Register covering the period December 27, 2020, to May 4, 2022. This national register, initiated in 2013, is administrated by the Public Health Agency of Sweden (Swe: “Folkhälsomyndigheten”). Figure 2 illustrates the timeline for the vaccinations and the pandemic development over time in terms of the number of deaths.
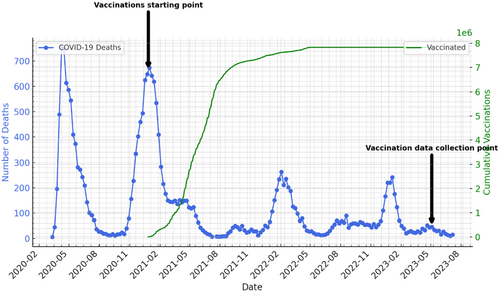
Figure 2 illustrates the two significant pandemic waves observed during the spring of 2020 and the winter of 2020/2021. Notably, during the peak of the second wave, the Swedish vaccination program commenced. In the subsequent months, vaccine supply remained relatively limited. However, by the time our data was collected on May 4, 2023, vaccination rates had plateaued. The green line in Figure 2 represents the number of individuals who had received at least one dose of the vaccine. It is evident that this number reached a plateau by the end of 2021, with very few additional individuals opting to receive the vaccine thereafter.
The trend shown in Figure 2 suggests that by May 2023, those who had not yet been vaccinated had made a deliberate decision to abstain, rather than being influenced by vaccine shortages or major infection peaks. In fact, the opposite appears to be true. On May 5, 2023, the day following our data collection, the World Health Organization declared an end to the Public Health Emergency of International Concern for COVID-19. The small peaks observed in infection rates since then resemble typical winter influenza patterns. Consequently, it seems likely that the remaining unvaccinated individuals had consciously chosen not to receive the vaccine, independent of any external constraints or pandemic dynamics.
It is mandated by law that all healthcare providers are legally obliged to report every vaccination administered to this register to record the effectiveness of the national vaccination program. This encompasses the documentation of individual-level data for each COVID-19 vaccination administered during this specified period. Additionally, the register encompasses the reporting of various other vaccinations, including those against diphtheria, tetanus, whooping cough, polio, Haemophilus influenzae type b, pneumococcus, MMR, HPV, and rotavirus. It is important to note that due to the legal framework, which came into effect in 2013, we lack information pertaining to potential vaccinations individuals in the data set may have received earlier in life.
We merge the data from the National Vaccine Register with microlevel register data from Statistics Sweden for the year 2020, that is, before the vaccination program was rolled out. This register data includes all individuals in Sweden aged 16 years and above, providing comprehensive information on various demographic and socioeconomic attributes, such as age, educational attainment, income, occupation, marital status, housing arrangements, workplace identification, as well as geo-coded residential location. On the basis of this information, we can trace who an individual lives together with, who he or she works with, as well as who lives in the same residential location. For all three levels, we measure the share in the individual's peer groups who are not vaccinated against COVID-19.
“Family,” in the context of the present paper, refers to individuals aged 16 and above who reside in the same household, as determined by the Household ID available in the database we utilize. We also rerun the analysis for individuals in the household aged 25 years or older. This is because parents are likely to exert a more substantial influence on the decision to get vaccinated compared with their children (Bell et al. 2020; Konstantinou et al. 2021). “Workplace” is defined based on the establishment, that is, the physical site where an individual conducts her or his employment activities, rather than the company for which the individual works (which may consist of several establishments). This approach enables us to precisely identify the individuals whom a person interacts with in the professional milieu. This means that every individual in the registry data sharing the same workplace ID is employed by the same firm and occupies the same physical workspace, thus letting us identify with whom an individual interacts at work.
In this investigation, we employ a spatial neighborhood unit referred to as “Regional Statistical Area” (RegSO). This geographical definition has been developed by Statistics Sweden to facilitate the analysis of socioeconomic structures. Notably, the RegSO definition of neighborhoods considers socioeconomic factors, like, household income, housing type, demographic homogeneity, and location-specific demographic conditions. The RegSO neighborhoods are demarcated by spatial boundaries, encompassing features, such as streets, waterways, and railways. In essence, they should represent genuine residential communities rather than being mere administrative constructs. The RegSO populations range from 663 to 22,622 individuals.
We merge the vaccination data from the National Vaccination Register with microlevel register data made available by Statistics Sweden. To be able to disentangle the relative importance of each peer group, we select individuals that live in a family setting (at least two persons in the household), have a job in a certain workplace, and a known place of residence. This data set encompasses 4,125,561 observations. We also run robustness checks for individuals with only a family and a place of residence, but not necessarily a registered workplace. This can be, for example, due to unemployment, studies, or retirement. When doing so, the data set encompasses 6,234,175 individuals. Approximately 12.5% of the individuals included in Statistics Sweden's records do not appear in the National Vaccination Register, meaning that they have not received the COVID-19 vaccination. It is plausible that some in this group may have been vaccinated in another country, a circumstance that would not be documented in the National Vaccination Register. However, considering the restrictions put on international travel during the timeframe of our study, we argue that most of the cohort of 12.5% that are not in the vaccination register cohort made a deliberate choice not to get vaccinated.
3 Results
We start with a correlation analysis to gain an initial understanding of how our main variables of interest (individual vaccination status, share of unvaccinated household, workplace, and neighborhood members) are related to one another. Table 1 illustrates these relationships.
| Individual vaccination status | Unvaccinated HH | Unvaccinated WP | |
|---|---|---|---|
| Unvaccinated HH | 0.515*** | — | — |
| Unvaccinated WP | 0.476*** | 0.329*** | — |
| Unvaccinated NH | 0.196*** | 0.237*** | 0.241*** |
- Abbreviations: HH = household, NH = neighborhood, WP = workplace.
- *** Indicates significance at the 1% level.
The strongest relationships are observed between the individual vaccination status on the one hand and the unvaccinated share at home and in the workplace, with correlations of 0.515 and 0.476, respectively, significant at the 1% level. The correlation between individual vaccination status and the unvaccinated share in the neighborhood is also significant at the 1% level, but the magnitude is smaller, 0.196.
The dependent variable P(Unvaccinated = 1) represents the probability that the individual i is not vaccinated. The coefficients β1, β2, and β3 correspond to the key independent variables, which measure the share of unvaccinated individuals in the household (HH), workplace (WP), and residential neighborhood (NH), respectively. The δ coefficients are associated with various individual control variables: age, gender, ethnic background civil status, occupation, disposable income, education, and housing. We also add a dummy for the municipality in which the individual lives. Finally, εi represents the error term, which captures unobserved factors. The model is estimated using robust standard errors to account for potential heteroscedasticity. All variables are from the year 2020, except for the vaccination variables, which were collected in May 2023 and cover the period from December 2020 to May 2023. Descriptive statistics for all included variables are presented in Tables A1–A3 in the appendix.
We estimate different versions of the regression model to enable the examination of the relative importance of the three peer groups—the family, the workplace, and the neighborhood—on the likelihood to not vaccinate against COVID-19 (Table 2). The findings are reported as average marginal effects (AMEs).
| Peers | (1) | (2) | (3) Reduced sample | (4) | (4a) Only 25 years and older |
|---|---|---|---|---|---|
| Unvaccinated HH | — | 0.159*** (0.0002) | — | 0.159*** (0.0002) | 0.145*** (0.0002) |
| Unvaccinated WP | — | 0.318*** (0.0007) | — | 0.317*** (0.0007) | 0.290*** (0.0007) |
| Unvaccinated NH | 0.237*** (0.0019) | — | 0.271*** (0.0026) | 0.048*** (0.0023) | 0.029*** (0.0024) |
| Age (base: 20–29) | |||||
| 30–39 | 0.014*** (0.0004) | −0.012*** (0.0004) | −0.004*** (0.0005) | −0.012*** (0.0004) | −0.004*** (0.0005) |
| 40–49 | −0.025*** (0.0004) | −0.034*** (0.0004) | −0.038*** (0.0005) | −0.034*** (0.0004) | −0.034*** (0.0005) |
| 50–59 | −0.054*** (0.0004) | −0.051*** (0.0004) | −0.063*** (0.0005) | −0.051*** (0.0004) | −0.052*** (0.0005) |
| 60–69 | −0.084*** (0.0004) | −0.067*** (0.0004) | −0.085*** (0.0005) | −0.067*** (0.0004) | −0.067*** (0.0005) |
| 70–79 | −0.117*** (0.0004) | −0.081*** (0.0007) | −0.104*** (0.0007) | −0.081*** (0.0007) | −0.081*** (0.0008) |
| 80–89 | −0.119*** (0.0004) | −0.078*** (0.0031) | −0.110*** (0.0021) | −0.078*** (0.0031) | −0.078*** (0.0029) |
| 90 + | −0.099*** (0.0007) | −0.020 (0.0248) | −0.066*** (0.0195) | −0.020 (0.0248) | −0.025 (0.0228) |
| Female | −0.012*** (0.0002) | −0.002*** (0.0002) | −0.008*** (0.0003) | −0.002*** (0.0002) | 0.0003 (0.0003) |
| Civil status (base: Single) | |||||
| Single with child | −0.005*** (0.0005) | 0.001 (0.0007) | 0.001 (0.0008) | 0.001 (0.0007) | −0.001 (0.0009) |
| Married | −0.029*** (0.0003) | 0.002*** (0.0003) | −0.017*** (0.0004) | 0.002*** (0.0003) | 0.0003 (0.0004) |
| Married with child | −0.035*** (0.0003) | −0.008*** (0.0003) | −0.025*** (0.0004) | −0.008*** (0.0003) | −0.011*** (0.0003) |
| Income | −0.025*** (0.0001) | −0.010*** (0.0002) | −0.025*** (0.0002) | −0.010*** (0.0002) | −0.008*** (0.0002) |
| Education level (base: less than High School) | |||||
| High School | −0.012*** (0.0003) | −0.003*** (0.0004) | −0.013*** (0.0005) | −0.003*** (0.0004) | −0.004*** (0.0004) |
| Shorter Higher Edu | −0.034*** (0.0004) | −0.011*** (0.0005) | −0.033*** (0.0005) | −0.011*** (0.0005) | −0.010*** (0.0005) |
| Longer Higher Edu | −0.043*** (0.0004) | 0.016*** (0.0005) | −0.047*** (0.0006) | 0.016*** (0.0005) | −0.016*** (0.0005) |
| Occupation (base: Managers) | |||||
| Occupations requiring an advanced level of higher education | 0.006*** (0.0006) | 0.022*** (0.0006) | 0.004*** (0.0007) | 0.022*** (0.0006) | 0.019*** (0.0006) |
| Occupations requiring higher education qualifications or equivalent | 0.018*** (0.0006) | 0.022*** (0.0006) | 0.016*** (0.0007) | 0.022*** (0.0006) | 0.019*** (0.0006) |
| Administration and customer service clerks | 0.034*** (0.0006) | 0.024*** (0.0007) | 0.029*** (0.0008) | 0.024*** (0.0007) | 0.022*** (0.0006) |
| Service, care, and shop sales workers | 0.036*** (0.0006) | 0.021*** (0.0006) | 0.029*** (0.0007) | 0.021*** (0.0006) | 0.021*** (0.0006) |
| Agricultural, horticultural, forestry, and fishery workers | 0.048*** (0.0011) | 0.008*** (0.0010) | 0.045*** (0.0014) | 0.008*** (0.0010) | 0.007*** (0.0010) |
| Building and manufacturing workers | 0.056*** (0.0007) | 0.025*** (0007) | 0.052*** (0.0008) | 0.025*** (0007) | 0.022*** (0.0006) |
| Mechanical manufacturing, transport workers, and so forth | 0.056*** (0.0007) | 0.031*** (0.0007) | 0.052*** (0.0009) | 0.031*** (0.0007) | 0.029*** (0.0007) |
| Elementary occupations | 0.049*** (0.0007) | 0.014*** (0.0007) | 0.039*** (0.0008) | 0.014*** (0.0007) | 0.014*** (0.0007) |
| Ethnic background (base: Native Swedes) | |||||
| Nordic | 0.043*** (0.0008) | 0.016*** (0.0010) | 0.031*** (0.0013) | 0.016*** (0.0010) | 0.014*** (0.0010) |
| EU15 | 0.088*** (0.0009) | 0.035*** (0.0010) | 0.081*** (0.0014) | 0.035*** (0.0010) | 0.032*** (0.0010) |
| West Balkan | 0.129*** (0.0010) | 0.031*** (0.0008) | 0.127*** (0.0013) | 0.031*** (0.0008) | 0.030*** (0.0008) |
| East Europe | 0.215*** (0.0009) | 0.040*** (0.0007) | 0.219*** (0.0012) | 0.040*** (0.0007) | 0.036*** (0.0007) |
| Middle East | 0.058*** (0.0005) | 0.005*** (0.0005) | 0.061*** (0.0007) | 0.005*** (0.0005) | 0.004*** (0.0005) |
| East Africa | 0.034*** (0.0007) | 0.005*** (0.0008) | 0.032*** (0.0010) | 0.005*** (0.0008) | 0.001 (0.0009) |
| North–South–West Africa | 0.068*** (0.0011) | 0.018*** (0.0011) | 0.065*** (0.0016) | 0.018*** (0.0011) | 0.017*** (0.0012) |
| South-Central Asia | −0.013*** (0.0005) | −0.016*** (0.0006) | −0.013*** (0.0007) | −0.016*** (0.0006) | −0.013*** (0.0006) |
| Southeast–East Asia | −0.014*** (0.0006) | −0.019*** (0.0007) | −0.026*** (0.0007) | −0.019*** (0.0007) | −0.018*** (0.0007) |
| South-Central America | 0.032*** (0.0010) | 0.005*** (0.0010) | 0.023*** (0.0013) | 0.005*** (0.0010) | 0.005*** (0.0009) |
| North America–Oceania | 0.080*** (0.0021) | 0.039*** (0.0022) | 0.063*** (0.0029) | 0.039*** (0.0022) | 0.037*** (0.0022) |
| Elderly home | −0.030*** (0.0010) | −0.001 (0.0045) | −0.0021 (0.0050) | −0.001 (0.0045) | 0.0004*** (0.0048) |
| House type (base: Rental apartment) | |||||
| Tenant-owned (apartment) | −0.020*** (0.0003) | −0.003*** (0.0004) | −0.016*** (0.0004) | −0.003*** (0.0004) | −0.002*** (0.0004) |
| Owner-occupied (house) | −0.013*** (0.0003) | −0.001*** (0.0003) | −0.010*** (0.0004) | −0.001*** (0.0003) | 0.001*** (0.0004) |
| Intergenerational household | 0.050*** (0.0013) | 0.015*** (0.0012) | 0.028*** (0.0016) | 0.015*** (0.0012) | 0.014*** (0.0019) |
| Crowded household | 0.029*** (0.0004) | 0.009*** (0.0003) | 0.023*** (0.0005) | 0.009*** (0.0003) | 0.007*** (0.0004) |
| Municipality control | Yes | Yes | Yes | Yes | Yes |
| N | 8,314,025 | 4,125,561 | 4,125,561 | 4,125,561 | 3,575,963 |
| Pseudo-R2 | 0.1741 | 0.4253 | 0.1550 | 0.4255 | 0.4492 |
- Abbreviations: HH = household, NH = neighborhood, WP = workplace.
- *** Denotes significance at 1% level, **denotes significance at 5% level, and *denotes significance at 10% level. Dependent variable = 1 if not getting the COVID-19 vaccine, zero otherwise.
Starting with specification 1, where we let the share of unvaccinated individuals in the neighborhood explain the likelihood of an individual not getting vaccinated, controlling for individual and geographic characteristics. The magnitude of the neighborhood coefficient is 0.237 and highly statistically significant. The neighborhood vaccination rate thus seems to be one significant indicator for explaining the likelihood of getting vaccinated.
Next, we exclude the neighborhood variable and, instead, explain the likelihood of not getting the vaccine using the shares of unvaccinated individuals in the household (family) and workplace (specification 2). It is important to note that this reduces the number of observations by approximately half (from 8,314,025 to 4,125,561) because many individuals live in single households and, therefore, do not have any other individuals residing in the same household. The household variable yields a coefficient of 0.159, and the workplace variable yields a coefficient of 0.318, both of which are highly statistically significant. These results suggest that the association between the likelihood of not receiving the COVID-19 vaccine is approximately twice as strong with the share of unvaccinated individuals in the workplace as compared with that in the household. This can be interpreted as if the workplace peers most likely would have a more pronounced impact on the probability of not getting vaccinated. However, we are more likely to have larger variations in the share of unvaccinated at the family level than the workplace level. Due to fewer family members than coworkers, the effect of an additional unvaccinated person is likely to be larger at the household level than the workplace level.
We subsequently conducted regression 3 with the same individuals as in regression 2 (N = 4,125,561) but replaced the family and workplace variables with the share of the neighborhood that did not get vaccinated (as in specification 1). We do this to examine whether the neighborhood coefficient is influenced by the changed group of individuals. The coefficient is now 0.271, indicating an even stronger relationship between the share of the neighborhood that did not get vaccinated and the likelihood of an individual making the same decision. These results seem to indicate that neighborhood effects are both significant and quite substantial, in line with some previous research (cf. Kain 1968; Dietz 2002; Sampson et al. 2002; Durlauf 2004; Kling et al. 2007; Roosa and White 2014; Arcaya et al. 2016; Rotger and Galster 2019).
However, in the next step (specification 4), we include all three variables—the share of unvaccinated individuals in the household, the workplace, and the neighborhood—to explain the likelihood of an individual not receiving the COVID-19 vaccine. The results align with what we discovered in regression 2 for the household and workplace variables, with coefficients of 0.159 and 0.317, respectively. However, the neighborhood variable exhibits a significantly smaller effect compared with what we observed in the initial specification. The coefficient is now 0.048, compared with the previous 0.237 or 0.271. This suggests that for individuals with both family and workplace connections, the influence of the neighborhood is more limited than we might have initially assumed and expected based on the large literature on neighborhood effects. Also, using the results from specification 4 in Table 2 we tested if indeed the coefficients for household, workplace, and neighborhood are statistically different from each other. By applying pairwise z tests we concluded that all three coefficients are different from one another at the 1% level. Hence, many studies of neighborhood effects are not only plagued by issues of spatial sorting making causal inference unfeasible if not controlled for (cf. Bolster et al. 2007; Ioannides and Topa 2010; van Ham and Manley 2010; Galster 2012; Graham 2018), but also of omitted variable bias resulting from a neglect of individuals' social spaces beyond the neighborhood of residence.
Since we assume that children in the household can be strongly influenced by their parents in their decision to get vaccinated, we have excluded everyone below the age of 25 to avoid that the results are affected by this. We then rerun specification 4 but now only for individuals above the age of 25 (3,575,963). Again, we find the strongest relations between the likelihood of not getting vaccinated and the peers in the workplace, with a marginal effect of 0.290. The share in the household is approximately half the size (0.145), while the neighborhood coefficient is only 0.029, that is, one-tenth of the workplace coefficient.
Taken together, our results suggest that peers in the workplace may play a more pronounced role than those with whom an individual resides, both at home and in the neighborhood. Having said this, the neighborhood still appears to be statistically significant, although the magnitude of the effect and thus the societal relevance is limited.
The results for the control variables are mainly in line with expectations. Individuals who are older, in some sort of family constellation, who have a higher education, a higher income, and/or a more “advanced” occupation are less likely to not vaccinate against COVID-19. Regarding housing conditions, individuals in rental apartments are, as expected, most likely to not get vaccinated. Similarly, individuals residing in intergenerational and/or crowded households are more likely to not vaccinate against COVID-19, perhaps implying that these household features may pick up socioeconomically weak families. Regarding ethnic background, nonnative Swedes are generally more likely to not get vaccinated. Interestingly, the exception is individuals from Asia, which may be due to greater awareness of the potential dangers of COVID-19 in the Asian societies to which these individuals may still be connected to.
3.1 Robustness Tests
To ensure that the results are not driven by vaccine-hesitant individuals moving to certain neighborhoods and/or changing workplaces due to the pandemic, we select individuals who have either (1) lived in the same neighborhood for at least for 10 years, or (2) worked in the same workplace for at least 10 years, or (3) both lived and worked in the same place for at least 10 years. We rerun the same regressions but now only look at these populations. Table 3 illustrates the results.
| Peers | (1) | (2) | (3) Reduced sample | (4) | (4a) Only 25 years and older |
|---|---|---|---|---|---|
| Same NH | |||||
| Unvaccinated HH | — | 0.133*** (0.0003) | — | 0.132*** (0.0008) | 0.115*** (0.0003) |
| Unvaccinated WP | — | 0.264*** (0.0009) | — | 0.262*** (0.0009) | 0.235*** (0.0009) |
| Unvaccinated NH | 0.221*** (0.0025) | — | 0.261*** (0.0035) | 0.063*** (0.0031) | 0.034*** (0.0032) |
| Individual and municipality controls | Yes | Yes | Yes | Yes | Yes |
| N | 4,224,092 | 1,966,985 | 1,966,985 | 1,966,985 | 1,716,491 |
| Pseudo-R2 | 0.1519 | 0.4400 | 0.1351 | 0.4405 | 0.46562 |
| Same WP | |||||
| Unvaccinated HH | — | 0.102*** (0.0004) | — | 0.102*** (0.0004) | 0.099*** (0.0004) |
| Unvaccinated WP | — | 0.204*** (0.0013) | — | 0.204*** (0.0012) | 0.120*** (0.0013) |
| Unvaccinated NH | 0.139*** (0.0019) | — | 0.129*** (0.0026) | 0.004*** (0.0044) | 0.007*** (0.0045) |
| Individual and municipality controls | Yes | Yes | Yes | Yes | Yes |
| N | 1,103,735 | 888,192 | 888,192 | 888,192 | 864,775 |
| Pseudo-R2 | 0.0967 | 0.4627 | 0.1018 | 0.4627 | 0.4700 |
| Both the same NH and WP | |||||
| Unvaccinated HH | — | 0.094*** (0.0005) | — | 0.094*** (0.0005) | 0.090*** (0.0004) |
| Unvaccinated WP | — | 0.088*** (0.0014) | — | 0.188*** (0.0014) | 0.184*** (0.0014) |
| Unvaccinated NH | 0.127*** (0.0057) | — | 0.116*** (0.0060) | 0.0006 (0.0051) | 0.004 (0.0051) |
| Individual and municipality controls | Yes | Yes | Yes | Yes | Yes |
| N | 771,869 | 634,398 | 634,398 | 634,398 | 619,156 |
| Pseudo-R2 | 0.0932 | 0.4724 | 0.0960 | 0.4724 | 0.4780 |
- Abbreviations: HH = household, NH = neighborhood, WP = workplace.
- *** Denotes significance at 1% level, **denotes significance at 5% level, and *denotes significance at 10% level. Dependent variable = 1 if not getting the COVID-19 vaccine, zero otherwise.
In cases where individuals have lived and/or worked longer with their peers, the results remain largely consistent with those presented in Table 1. Even though the coefficients decrease in size, they remain significant, and the most significant peer group continues to be those individuals who meet at work, followed by those in the household. Additionally, the neighborhood variable weakens significantly as we control for the home and work peer groups. Interestingly, the difference in coefficient values between the household and workplace peer groups decreases for individuals over the age of 25 who have worked in the same workplace for at least 10 years, with the coefficients for home and work being 0.099 and 0.120, respectively. This suggests a convergence in the influence of peer groups at home and at work overtime when individuals have been in the same workplace for an extended period.
Looking at the spatial heterogeneity of vaccination rates across the entire country (as shown for the three metropolitan regions in Figure 1), we observe that the greatest variations in vaccination rates are found within densely populated areas, and neighborhoods with relatively high rates of unvaccinated are more or less exclusively found in urban parts of municipalities. To test whether this is specifically an urban phenomenon, we split the sample and rerun the estimations for individuals residing in urban versus rural neighborhoods. The results are presented in Table 4.
| Peers | (1) | (2) | (3) Reduced samplea | (4) | (4a) Only 25 years and older |
|---|---|---|---|---|---|
| Urban | |||||
| Unvaccinated HH | — | 0.161*** (0.0003) | — | 0.160*** (0.0003) | 0.146*** (0.0003) |
| Unvaccinated WP | — | 0.317*** (0.0008) | — | 0.316*** (0.0004) | 0.288*** (0.0008) |
| Unvaccinated NH | 0.226*** (0.0020) | — | 0.309*** (0.0027) | 0.047*** (0.0024) | 0.028*** (0.0025) |
| Individual and municipality controls | Yes | Yes | Yes | Yes | Yes |
| N | 7,239,683 | 3,517,256 | 3,517,256 | 3,517,256 | 3,024,508 |
| Pseudo-R2 | 0.1807 | 0.4153 | 0.1622 | 0.4153 | 0.4382 |
| Rural | |||||
| Unvaccinated HH | — | 0.146*** (0.0005) | — | 0.145*** (0.0005) | 0.135*** (0.0005) |
| Unvaccinated WP | — | 0.307*** (0.0017) | — | 0.307*** (0.0017) | 0.286*** (0.0017) |
| Unvaccinated NH | 0.433*** (0.0019) | — | 0.587*** (0.0116) | 0.095*** (0.0145) | 0.089*** (0.0147) |
| Individual and municipality controls | Yes | Yes | Yes | Yes | Yes |
| N | 1,074,342 | 608,305 | 608,305 | 608,305 | 551,455 |
| Pseudo-R2 | 0.1336 | 0.4972 | 0.1023 | 0.4973 | 0.5210 |
- Abbreviations: HH = household, NH = neighborhood, WP = workplace.
- a Regression 3 did not converge when we included all 290 Municipal control variables. In this case, we instead used six municipal control variables that capture the degree of urbanity/rurality.
- *** Indicates significance at the 1% level.
Once again, we find that the results are robust. The neighborhood coefficient tends to be overestimated in both urban settings and, to a greater extent, in rural areas. The size of the neighborhood coefficient decreases significantly once we control for the unvaccinated share within the household and workplace. Furthermore, the relative size of the marginal effects from the estimations for unvaccinated share in the household, workplace, and neighborhood remain consistent throughout the analyses. Finally, we rerun the estimations holding one or several of the social contexts (household, workplace, neighborhood) constant. Although these analyses do not allow us to discuss the relative importance of the various contexts, which is central to this paper, it allows us to test the robustness of household, workplace, and neighborhood effects. Table 5 illustrates the results on the main variables.
| Peers | (1) Constant NH | (2) Constant WP | (3) Constant HH and NH |
|---|---|---|---|
| Unvaccinated HH | 0.407*** (0.0008) | 0.448*** (0.0009) | — |
| Unvaccinated WP | 0.671*** (0.0012) | — | 0.454*** (0.0023) |
| Unvaccinated NH | — | 0.166*** (0.0041) | — |
| Individual and municipality controls | Yes | Yes | Yes |
| N | 4,125,561 | 3,829,717 | 2,811,212 |
| R2 | 0.3936 | 0.3765 | 0.7704 |
| Within R2 | 0.3645 | 0.2383 | 0.0914 |
- Note: Note that the linear probability model (LPM) produces larger average marginal effects (AMEs) than the logit also when the model is estimated with all three social contexts included. The corresponding LPM estimates of specification 4 in Table 2 is 0.405*** for Unvaccinated HH, 0.672*** for Unvaccinated WP, and 0.098*** for Unvaccinated NH.
- Abbreviations: HH = household, NH = neighborhood, WP = workplace.
- *** Denotes significance at 1% level, **denotes significance at 5% level, and *denotes significance at 10% level. The AMEs are retrieved from linear probability models allowing for many levels of fixed effects (Correia 2017). Within R2 relates to the explanatory power of the regressors, with the fixed effects (at NH, WP, and/or HH) already accounted for.
As shown in Table 5, the main results on peer effects are robust when isolating the effects for individuals in (1) the same neighborhood, (2) the same workplace, and (3) the same household (which also places them in the same neighborhood). All peer effects remain significant, with the AME of unvaccinated in the neighborhood being smaller than the AME of unvaccinated at the household level for individuals at the same workplace, and workplace AMEs being larger than household AMEs for individuals residing in the same neighborhood.
To further ensure that our variable, “unvaccinated share in the neighborhood,” does not unintentionally capture other neighborhood characteristics, we include a set of additional neighborhood control variables in our analysis.
One potential concern is that the unvaccinated share in the neighborhood may not be directly related to COVID-19 vaccination but rather reflects a broader pattern of vaccine hesitancy. Since the COVID-19 vaccine was recently introduced at the time of our study, no earlier data on its uptake are available. Still, to address this, we control for the share of 18- and 19-year olds in the neighborhood who received the HPV vaccine.
In Sweden, the HPV vaccination program was introduced in 2010 as part of the national childhood immunization schedule. The vaccine provides protection against the HPV, which can lead to cervical cancer, other anogenital cancers, and genital warts. Initially, the program targeted girls aged 10–12 through school-based vaccinations, with a catch-up program available for older girls up to 18 years of age. Later, the program was expanded to include boys, as HPV also causes cancers in men, such as oropharyngeal and anal cancer. The correlation between the neighborhood share of COVID-19-vaccinated individuals and the neighborhood share of HPV-vaccinated individuals in the 18–19 age group is relatively low at 0.344, significant at the 1% level.
Also, given that COVID-19 affected neighborhoods differently, we control for the share of the neighborhood population that died from COVID-19 during the pandemic year of 2020. It is possible that in areas where a larger proportion of the population died with COVID-19 as the cause of death, this experience may have influenced individuals' willingness to receive the vaccine at a later stage.
Finally, we account for other neighborhood characteristics by controlling for population density and ethnic diversity within the neighborhood. These factors may influence both social interactions and health-related behaviors, including vaccination uptake. Table 6 illustrates the results.
| Peers | (1) | (2) | (3) Reduced sample | (4) | (4a) Only 25 years and older |
|---|---|---|---|---|---|
| Unvaccinated HH | — | 0.159*** (0.0002) | — | 0.159*** (0.0002) | 0.145*** (0.0002) |
| Unvaccinated WP | — | 0.317*** (0.0007) | — | 0.316*** (0.0007) | 0.290*** (0.0007) |
| Unvaccinated NH | 0.394*** (0.0035) | — | 0.411*** (0.0045) | 0.087*** (0.0040) | 0.065*** (0.0041) |
| Neighborhood control variables | |||||
| HPV Vaccinated NH | −0.001 (0.0012) | −0.006*** (0.0014) | −0.005*** (0.0016) | −0.002 (0.0014) | −0.003 (0.0014) |
| COVID-19 deaths NH | −0.097 (0.0959) | −0.086 (0.1093) | −0.072 (0.1293) | 0.131 (0.1095) | 0.080 (0.1130) |
| Population density (K) NH | −0.0001*** (0.00003) | −0.0001*** (0.00003) | −0.0001*** (0.00004) | −0.0005*** (0.00004) | −0.00004*** (0.000004) |
| Ethnic diversity NH | −0.031*** (0.0006) | −0.0036*** (0.00004) | −0.028*** (0.0008) | −0.008*** (0.0006) | −0.0076*** (0.00007) |
| Individual and municipality controls | Yes | Yes | Yes | Yes | Yes |
| N | 8,314,025 | 4,125,561 | 4,125,561 | 4,125,561 | 3,575,963 |
| Pseudo-R2 | 0.1749 | 0.4254 | 0.1560 | 0.4256 | 0.4494 |
- Abbreviations: HH = household, NH = neighborhood, WP = workplace.
- *** Denotes significance at 1% level, **denotes significance at 5% level, and *denotes significance at 10% level. Dependent variable = 1 if not getting the COVID-19 vaccine, zero otherwise.
As shown in Table 6, the coefficient for the unvaccinated share in the neighborhood remains robust even after the inclusion of additional neighborhood control variables. Furthermore, while the pairwise correlation between the COVID-19 unvaccinated share in the neighborhood and the HPV unvaccinated share among 18- and 19-year olds in the same neighborhood is 0.344, the latter has a significantly weaker explanatory power regarding an individual's decision not to receive the COVID-19 vaccine.
The relative strength of our three key variables—the unvaccinated share in the household, workplace, and neighborhood—remains consistent even after the inclusion of these neighborhood control variables.
4 Conclusions
Individuals' behaviors and decisions can be significantly shaped by their peers, referring to those within social circles sharing similar interests, backgrounds, education, or societal positions. Peer groups have a substantial influence over an individual's beliefs, values, attitudes, and behaviors, often leading to conformity within these influential groups. Several studies (Coleman 1968; Calvó-Armengol et al. 2009; Mas and Moretti 2009; Van Veldhuizen et al. 2018; Epple and Romano 2011; Correia 2017; Battisti 2017; Oakes et al. 2015; Bailey et al. 2022) showcase how individuals' attitudes, values, and behaviors change as they interact with their peers.
Neighborhood effects have been an extensive area of study, examining how an individual's decisions, behaviors, and outcomes are influenced by the socioeconomic and behavioral characteristics of those sharing the same residential space (Kain 1968; Dietz 2002; Sampson et al. 2002; Durlauf 2004; Kling et al. 2007; Roosa and White 2014; Arcaya et al. 2016). However, social interactions occur not only within residential areas but also in various other environments individuals frequent during their waking hours (Cagney et al. 2020). Peer groups can also be expected to be formed within workplaces, neighborhoods, and households, impacting decision-making through social pressure and knowledge sharing.
Here we explored three possible peer groups influencing the decision-making process regarding the COVID-19 vaccine: family, colleagues in the workplace, and neighbors. While existing research has predominantly emphasized the significance of neighborhood influence on this decision, fewer studies have encompassed the roles of family and the workplace. Our study aimed to achieve two primary objectives: first, to disentangle the predominant factors in a decision where individuals possessed limited prior knowledge and needed to make an informed choice; second, to examine whether the perceived impact of neighborhood peers might have been over-estimated when considering the influence of both home and workplace environments as well.
We find that the AME of an increase in the share of unvaccinated colleagues at an individual's workplace is larger than the corresponding AMEs of an increased share of unvaccinated among one's family or neighborhood peers. We also find that the influence of neighborhoods as a peer group in the decision-making process regarding COVID-19 vaccination may have been overestimated. While neighborhoods undeniably play a significant role, their impact is likely considerably over-estimated when solely focusing on neighborhoods without considering other influential peer groups at work and at home.
We acknowledge that sorting into neighborhoods does occur, and our data supports this. However, if sorting played a substantial role in driving decisions like this, we might expect to observe a stronger coefficient for the neighborhood variable. Interestingly, our analysis shows that while the coefficient for neighborhoods is relatively large when we do not account for households and workplaces, its size decreases significantly once these factors are controlled for. This reduction in the neighborhood effect, even in the presence of sorting, suggests that households and workplaces are far more influential in shaping vaccination decisions than neighborhoods are. In other words, despite sorting, neighborhoods seem to matter less for this specific decision-making process than might have been anticipated.
The results presented here suggest that neighborhoods do have some influence, and it is possible that they contribute in smaller ways to many important life outcomes. These small effects may accumulate across various domains—such as education, jobs, and income—leading to a more significant overall impact. Our analysis illustrates the importance of not overestimating the role of neighborhoods in decision-making processes, while still recognizing their contribution in a broader context.
It is hard to say exactly how unique Sweden was in this situation, especially given the presumed relatively high level of trust in the government and healthcare. In Sweden, the level of what is commonly referred to as generalized trust among the population is remarkably high, reflecting a strong sense of social cohesion, institutional confidence, and interpersonal reliability (Berggren and Jordahl 2006; Charron and Rothstein 2016).
High trust in government encourages citizens to follow public health recommendations, such as vaccination programs. This confidence makes people more likely to accept information from authorities, believing that policies are designed with their best interests in mind, which in turn reduces the impact of misinformation and skepticism. Consequently, higher trust can lead to increased vaccine uptake and a more effective public health response during a crisis like the COVID-19 pandemic. Multiple studies and international surveys have shown that Swedish citizens consistently exhibit high confidence in their government and public institutions (European Commission 2019; OECD 2022; Statistics Sweden SCB 2020; Transparency International 2022). While Sweden's COVID-19 vaccination rates were high, they were comparable to those in other Nordic and high-income countries with similar levels of institutional trust and healthcare infrastructure.
The country did, in fact, have a relatively high vaccination rate compared with many other countries (Johns Hopkins 2024), but a smaller share of the population received at least one dose (77.4%) compared with, for example, the United States (81.8%), the United Kingdom (79.3%), and the other Nordic countries (ranging from 80.2% to 82.2%). The issue of COVID-19 vaccinations was also very polarizing in Sweden (Önnerfors 2024). There were strong opinions both in favor of and against vaccination, and it became a big topic in public debates as the vaccines were being rolled out. This means that while Sweden's specific social and cultural setting may have a certain influence on the findings, we still expect that discussions within peer groups were important in shaping people's decisions during this time.
The findings are interesting given that numerous vaccination information campaigns have primarily targeted neighborhoods to reach unvaccinated individuals under the assumption that this would be the most efficient way to affect the decision-making and to increase vaccination rates. But, if an individual's decision is primarily influenced by their workplace's social interactions, it may be more important for policy makers to stress workplaceh-related factors, such as workplace culture, workplace information influence, social pressure in workplaces, attitudes among leadership, and other socioeconomic workplace factors, to affect the individual's decision and thereby increase vaccination rates. By investing more resources into increasing vaccinations in certain neighborhoods, even though these areas have a relatively small impact on individuals' propensity to get vaccinated, it may lead to an inefficient resource allocation, and where a reallocation of resources may lead to a bigger impact. Focusing on neighborhoods to increase vaccination rates, risks neglecting other fundamental factors shaping individual choices. This oversight might disregard other crucial areas where interventions could yield greater benefits. Further, more comprehensive strategies can incorporate multiple determinants influencing individual decisions. Broadening the scope to include more influential factors could enhance the efficacy of endeavors in the decision-making process, here aimed at boosting vaccination rates.
While our study relies on high-quality fine-grained data, it is essential to acknowledge the limitations. A significant constraint is the absence of information about individuals' online connections and interactions on social media platforms. These digital spaces likely have a significant influence on individuals' decision-making processes, also potentially affecting their attitudes toward vaccinations. We encourage further research specifically focusing on the role of online connections and social media interactions in individuals' decision-making, also with a focus on vaccinations, contributing to a more comprehensive understanding of the complex phenomenon of decision-making.
Endnotes
Appendix
| Variable | Description | |
|---|---|---|
| Dependent variable | ||
| Unvaccinated individual | Binary variable equal to 1 if individual i did not get any vaccine shot against COVID-19, zero otherwise. Dependent variable. | |
| Independent variables | ||
| Unvaccinated HH | The share in the household aged 16 or above (or aged 25 or above) that did not get vaccinated against COVID-19. | |
| Unvaccinated WP | The share in the workplace that did not get vaccinated against COVID-19. | |
| Unvaccinated NH | The share in the neighborhood that did not get vaccinated against COVID-19. | |
| Age | Categorical variable of age groups: | |
|
|
|
| Female | Binary variable equal to 1 if female. | |
| Civil status | Categorical variable:
|
|
| Income | The natural logarithm of disposable income, inferred from the whole family's disposable income (disposable income per consumption weight). | |
| Education | Categorical variable showing highest formal schooling attainment:
|
|
| Occupation | Categorical variable showing the type of occupation:
|
|
| Ethnic background | Categorical variable showing the region of origin: | |
|
|
|
| Elderly home | Binary variable equal to 1 if residing in an elderly home. | |
| Intergenerational household | Binary variable equal to 1 if residing in an intergenerational household. | |
| Crowded household | Binary variable equal to 1 if residing in a crowded household. | |
| House type | Categorical variable showing housing type:
|
|
| HPV vaccinated NH | Share of 18- and 19-year olds who were vaccinated against HPV in the neighborhood in 2020 | |
| COVID-19 deaths NH | Number of individuals who died with COVID-19 in 2020 as a share of total neighborhood population aged 16 and above. | |
| Population density NH | Neighborhood population per square kilometer. | |
| Ethnic diversity NH | Entropy measure: , where denotes the share of neighborhood population with ethnic background g. | |
- Abbreviations: HH = household, HPV = human papillomavirus, NH = neighborhood, WP = workplace.
- a North America and Oceania are grouped together due to the relatively low number of foreign-born individuals with origin in these regions, as well as the sharing of similar cultural backgrounds
| Variable | Population | Mean | Std. Dev. | Minimum | Maximum |
|---|---|---|---|---|---|
| Unvaccinated HH | All | 0.1145 | 0.2913 | 0 | 1 |
| Vaccinated | 0.0631 | 0.2135 | 0 | 1 | |
| Unvaccinated | 0.5683 | 0.4504 | 0 | 1 | |
| Unvaccinated WP | All | 0.1056 | 0.1468 | 0 | 1 |
| Vaccinated | 0.0817 | 0.0944 | 0 | 0.9556 | |
| Unvaccinated | 0.3166 | 0.2897 | 0.0042 | 1 | |
| Unvaccinated NH | All | 0.1104 | 0.0590 | 0 | 0.4139 |
| Vaccinated | 0.1062 | 0.0546 | 0 | 0.4139 | |
| Unvaccinated | 0.1468 | 0.0804 | 0.0204 | 0.4139 | |
| Female | All | 0.4803 | 0.4996 | 0 | 1 |
| Vaccinated | 0.4873 | 0.4998 | 0 | 1 | |
| Unvaccinated | 0.4188 | 0.4934 | 0 | 1 | |
| Income (ln) | All | 8.000 | 0.6157 | 0 | 15.02 |
| Vaccinated | 7.847 | 0.8264 | 0 | 16.25 | |
| Unvaccinated | 6.918 | 2.176 | 0 | 14.46 | |
| Elderly home | All | 0.0005 | 0.0221 | 0 | 1 |
| Vaccinated | 0.0004 | 0.0211 | 0 | 1 | |
| Unvaccinated | 0.0009 | 0.0292 | 0 | 1 | |
| Intergenerational HH | All | 0.0082 | 0.0899 | 0 | 1 |
| Vaccinated | 0.0077 | 0.0873 | 0 | 1 | |
| Unvaccinated | 0.0122 | 0.1099 | 0 | 1 | |
| Crowded HH | All | 0.1239 | 0.3295 | 0 | 1 |
| Vaccinated | 0.1106 | 0.3136 | 0 | 1 | |
| Unvaccinated | 0.2426 | 0.4286 | 0 | 1 | |
| HPV vaccinated NH | All | 0.8039 | 0.1072 | 0.0769 | 1 |
| Vaccinated | 0.8063 | 0.1066 | 0.0769 | 1 | |
| Unvaccinated | 0.7822 | 0.1104 | 0.0769 | 1 | |
| COVID-19 deaths NH | All | 0.0012 | 0.0012 | 0 | 0.0122 |
| Vaccinated | 0.0011 | 0.0012 | 0 | 0.0122 | |
| Unvaccinated | 0.0013 | 0.0013 | 0 | 0.0122 | |
| Population density NH | All | 2822 | 4740 | 0.0735 | 33,531 |
| Vaccinated | 2769 | 4749 | 0.0735 | 33,531 | |
| Unvaccinated | 3290 | 4630 | 0.0735 | 33,531 | |
| Ethnic diversity NH | All | 0.8882 | 0.4328 | 0.1883 | 2.285 |
| Vaccinated | 0.8644 | 0.4140 | 0.1883 | 2.285 | |
| Unvaccinated | 1.098 | 0.5282 | 0.1883 | 2.285 |
- Note: The number of observations is 4,125,561 for all, split between 3,705,894 vaccinated and 419,667 unvaccinated.
- Abbreviations: HH = household, HPV = human papillomavirus, NH = neighborhood, WP = workplace.
| Share | |||
|---|---|---|---|
| Variable/category | All | Vaccinated | Unvaccinated |
| Age | |||
| 20–29 | 0.2015 | 0.1879 | 0.3218 |
| 30–39 | 0.2193 | 0.2107 | 0.2960 |
| 40–49 | 0.2185 | 0.2209 | 0.1974 |
| 50–59 | 0.2129 | 0.2222 | 0.1312 |
| 60–69 | 0.1199 | 0.1282 | 0.0468 |
| 70–79 | 0.0264 | 0.0287 | 0.0064 |
| 80–89 | 0.0013 | 0.0015 | 0.0003 |
| 90 + | 0.00004 | 0.00004 | 0.00002 |
| Civil status | |||
| Single | 0.2624 | 0.2507 | 0.3650 |
| Single with child | 0.0280 | 0.0258 | 0.0472 |
| Married | 0.3038 | 0.3165 | 0.1915 |
| Married with child | 0.4058 | 0.4069 | 0.3962 |
| Education level | |||
| Less than high school | 0.1021 | 0.0104 | 0.1688 |
| High school | 0.4451 | 0.4775 | 0.5232 |
| Shorter higher education | 0.1572 | 0.1742 | 0.1373 |
| Longer higher education | 0.2956 | 0.3379 | 0.1708 |
| Occupations | |||
| Managers | 0.0731 | 0.0776 | 0.0299 |
| Requiring advanced level of higher education | 0.2654 | 0.2795 | 0.1321 |
| Requiring higher education qualifications or equivalent | 0.1350 | 0.1391 | 0.0956 |
| Administration and customer service clerks | 0.0804 | 0.0793 | 0.0905 |
| Service, care, and shop sales workers | 0.2108 | 0.2050 | 0.2656 |
| Agricultural, horticultural, forestry, and fishery workers | 0.0208 | 0.0210 | 0.0192 |
| Building and manufacturing workers | 0.0905 | 0.0847 | 0.1457 |
| Mechanical manufacturing, transport workers, and so forth | 0.0684 | 0.0644 | 0.1066 |
| Elementary occupations | 0.0557 | 0.0494 | 0.1148 |
| Ethnic background | |||
| Native Swedes | 0.7896 | 0.8350 | 0.5510 |
| Nordic | 0.0171 | 0.0178 | 0.0147 |
| EU15 | 0.0172 | 0.0163 | 0.0279 |
| West Balkan | 0.0197 | 0.0163 | 0.0534 |
| East Europe | 0.0335 | 0.0002 | 0.1331 |
| Middle East | 0.0434 | 0.0371 | 0.1070 |
| East Africa | 0.0130 | 0.0111 | 0.0315 |
| North–South–West Africa | 0.0079 | 0.0067 | 0.0206 |
| South-Central Asia | 0.0254 | 0.0258 | 0.0274 |
| Southeast–East Asia | 0.0180 | 0.0189 | 0.0136 |
| South-Central America | 0.0114 | 0.0112 | 0.0151 |
| North America–Oceania | 0.0037 | 0.0036 | 0.0048 |
| House type | |||
| Rental apartment | 0.2326 | 0.2126 | 0.4123 |
| Tenant-owned apartment | 0.1924 | 0.1935 | 0.1829 |
| Owner-occupied house | 0.5750 | 0.5940 | 0.4047 |
- Note: The number of observations is 4,125,561 for all, split between 3,705,894 vaccinated and 419,667 unvaccinated.
Open Research
Data Availability Statement
The data that support the findings of this study are available from Statistics Sweden. Restrictions apply to the availability of these data, which were used under license for this study. Data are available from https://www.scb.se/en/services/ordering-data-and-statistics/microdata/mona--statistics-swedens-platform-for-access-to-microdata/ with the permission of Statistics Sweden.




