Nurse-led telephone follow-up for early palliative care patients with advanced cancer
Funding information
This work was partly supported thanks to the contribution of Ricerca Corrente by the Italian Ministry of Health within the research line “Appropriateness, outcomes, drug value and organizational models for the continuity of diagnostic-therapeutic pathways in oncology” (L1P2358)
Abstract
Aim and objectives
To present our experience of a nursing telephone consultation service, describing patient and caregiver requests, and outlining ensuing nursing or medical interventions.
Background
Recently, there has been an increase in the use of telephone consultation for cancer patients. However, there is still limited data on the characteristics of this type of service and on the nature of the interventions carried out.
Design and methods
In this observational retrospective study, we evaluated the phone calls made over a 6-month period by patients or caregivers to the early palliative care team of a cancer institute. Information regarding telephone calls (frequency, reason and management) was systematically collected by a nursing case manager. The study complies with the STROBE checklist File S1.
Results
171 patients used the service, for a total of 323 phone calls. The majority (80.8%) were from patients followed at the outpatient clinic and the most common requests were for pain management (38.4%) and for updates on the clinical situation (23.8%). Other frequent requests were for medication management (18.9%) and scheduling (18.3%). 210 of the 323 phone calls were handled by the nurse, while 22 were managed in collaboration with a physician. An 87.6% effectiveness in telephone management was observed.
Conclusion
The overall use of the phone service was higher for early palliative care patients. The majority of phone calls were effectively handled by the nursing case manager.
Relevance to clinical practice
An effective and feasible nurse-led telephone follow-up of early palliative care patients with advanced cancer could improve their care experience. Specifically, it could impact on patients and families improving quality of life and symptom control securing access to timely care without travel or additional cost.It can also improve continuity of care, adherence to oncological treatments and minimise acute care visits.
What does this paper contribute to the wider global clinical community?
- Nurse-led telephone service is a feasible and effective method to offer early PC follow-up.
- Nurse-led telephone follow-up for EPC patients should include symptom management, prescription management and logistical issues concerning territorial health care resources.
1 INTRODUCTION
Cancer patients, during the different stages of their illness, may experience severe physical and psychosocial symptoms that significantly impact their quality of life (QoL) and that of their families (Kirkova et al., 2010; Kutner et al., 2006). Early palliative care in oncology has been shown to have a positive impact on clinical outcome, quality of care and costs. Many studies have confirmed that the early integration of palliative care (PC) in patients with advanced cancer improves QoL, including physical and psychosocial symptoms, and also promotes a more appropriate use of healthcare services (Bakitas et al., 2009; Bauman & Temel, 2014; Davis et al., 2015; Ferrell et al., 2017; Maltoni et al., 2016; Maltoni et al., 2017; Temel et al., 2017; Zimmermann et al., 2014).
The management of patients in early PC is not straightforward as it coincides with active medical treatments involving a multiprofessional team, including palliative physicians and nurses, case managers, psychologists, social workers, dieticians and many more in various care settings. However, patients may experience worsening symptoms, deteriorating health conditions and/or logistic problems that make adherence to oncology treatments and outpatient supportive care visits more problematic. Hence, ongoing symptoms and patient management for patients receiving PC is vital (Yennurajalingam et al., 2012), often requiring an on-going and intensive follow-up. Advanced cancer patients are often in poor clinical conditions and experience worsening symptoms and deteriorating health; in addition, they could have logistical problems that may make adherence to an outpatient supportive care visit difficult. For all these reasons, there is a need for alternatives to traditional follow-up in PC outpatient clinic, involving nurses as well as physicians (Hui & Bruera, 2020). Whether to fulfil a need to intensify support or the geographic distance between patients and the clinic it is too far, telephonic follow-up could be a helpful solution to integrate with face-to-face consultation, both for patients and families but also for professionals, improving access to timely care for participants living in rural communities or for those who are not able to travel (Rogante et al., 2016).
Studies states that a nurse-led telephone follow-up for patients with cancer is acceptable, appropriate and/or effective, but there is still limited literature describing methods and evaluating effects (Cox et al., 2008; Cox & Wilson, 2003; Hintistan et al., 2017; Suh & Lee, 2017; Tan et al., 2021).
At IRCCS Istituto Romagnolo per lo Studio dei Tumori, PC and symptom control is offered in all care settings. Although some experience it as inpatients, we integrate specialised PC in oncology to better address supportive care needs, especially in an outpatient setting. Patients are referred for pain management, fatigue, nausea, vomiting, loss of appetite, lack of sleep, emotional distress, to assist their transition from curative treatment to PC, and to orient them towards the most suitable personalised care pathway. Recently, we adopted a different approach to manage patients' through a telephone follow-up program, going from a medical-centred method to a nurse-led one. By then, it was the PC physician to take care of patients and families' phone calls, with this change to a nurse-led telephone service we were hoping to reduce clinician work intensity, to improve patient satisfaction and continuity of care. This article describes our new method, evaluating the feasibility of a nurse-led telephone follow-up and patient and caregiver (CG) needs.
2 BACKGROUND
The World Health Organisation and current research are now focusing on integrating telemedicine into healthcare systems, especially at the present time of the COVID-19 emergency where patient access to medical facilities is sometimes more limited (Bokolo, 2020; Doraiswamy et al., 2020; Rogante et al., 2016).
Telephone services have been used in healthcare practice to offer follow-up contact with patients and their families and to offer assistance with various concerns: from symptom management, to prescription management, emotional support but also logistical concerns such as accessing territorial health resources. Telephone follow-up could be an efficient way for healthcare professional to guide patients and families to the most appropriate healthcare resources in case of need, potentially reducing the risk of recurrent hospitalizations (Cox & Wilson, 2003). Previous findings support the potential of telephone follow-up in reducing clinician work and access to emergency units, and increasing patient satisfaction (Bunn et al., 2004; Leibowitz et al., 2003; Purc-Stephenson & Thrasher, 2010) but also that a nurse-led telephone program improves access to care and early symptom management, especially in an advanced cancer setting (Bunn et al., 2005; Pimentel et al., 2015; Suh & Lee, 2017). However, there is still limited information in the literature on the characteristics of telephone programs specific for PC patients and on the nature of the interventions carried out (Mistiaen & Poot, 2006; Pimentel et al., 2015; Zhou et al., 2012).
The aim of this retrospective study was to present our experience of a telephone consultation program, to describe patient and caregiver requests, and to outline the ensuing nursing or medical actions undertaken. We also evaluated the potential benefits and critical issues of nurse-led telephonic case management to identify aspects of the initiative requiring improvement.
3 METHODS
3.1 Design and Data Collection
In this observational, retrospective study, we examined all consecutive phone calls made by patients to our PC team from 1 March 2020 to 31 August 2020. The first day of data collection coincided with a change in responsibility for the management of the telephone service from physicians to a PC nursing case manager, a recent addition to the multiprofessional team. Information about the telephone calls was systematically collected in a specifically created database and subsequently completed with data from the electronic medical records of patients.
3.2 Process of the telephone-call service
At each consultation, PC patients and their families were informed of the possibility of reaching us by phone or email on weekdays during working hours (8:30 am– 4:00 pm.). They were encouraged to call for issues regarding PC needs, for example, to discuss physical and psychosocial symptoms or medication management, plan appointments or express concerns about the personalised care trajectory. The service was provided by a case manager, a PC nurse with experience in supportive care and trained in the management of medications and counselling. Each day the nurse called back patients or CG who had contacted the PC team by email or left a message for the team with the reception. It was explained to patients that the service was not an emergency service and that they would be contacted within 48 h. Once the case manager understood the reason for the call, appropriate advice was provided if the problem was a nursing one, if the call was for clinical intervention the case manager would refer the call to the physician.
3.3 Data
The following data were collected: number of calls made by each patient undergoing PC or CG, reason for calling, recommendations made and type of intervention (medical or nursing). The database was completed by inserting information on age, gender, CG, type of tumour, metastasis, Eastern Cooperative Oncology Group performance status (ECOG PS) and ongoing pain medications.Telephone calls received were grouped into 2 main categories, i.e. interventional or logistic, as reported by Pimentel et al. (2015). Interventional needs included the management of cancer-related symptoms and medication education. Logistic needs addressed over the telephone included medication refills, scheduling, homecare organisation, hospice information and interdisciplinary issues/coordinating care. The study also evaluated the nature of each patient's call and the necessary nursing interventions made during the telephone interaction. The outcome of a call was used to evaluate the validity of the telephone service, i.e. a call was considered effective if the patient did not call again for the same reason, did not access the Emergency Room or did not die within the following 7 days. The 7-days criteria we chose to evaluate efficacy is based on PC patients fragility and frequent disease progression in short time: if evaluation time is too late, cancer progression may alter the efficacy of PC outpatient clinic. (Yennurajalingam et al., 2012). Therefore, we set an efficacy evaluation at the seventh day of each phone call, as also stated by Follwell et al. (2009), suggesting the ideal timing of an active telephone follow up is weekly.
3.4 Statistical analysis
- A second phone call received from the same patient for the same reason within 7 days of the first call suggested that that any previous interventions had not been effective; monthly verification of medical records to see whether the solutions offered to the patient or caregiver had resolved the problem and were appropriate;
- Evaluation of the member of PC staff taking care of each phone-call, whether it was a nursing problem or a medical problem. With this parameter, we could determine if the PC telephone service could be effectively managed by a nurse, for the most part.
3.5 Ethical statement
The study was approved by a Medical Scientific Committee and by an Ethics Committee; was also conducted in accordance with the principles laid down in the 1964 Declaration of Helsinki and Good Clinical Practice guidelines. As this was a non-interventional study based on the secondary use of data collected for other purposes (retrospective observational study), individual informed consent was not required.
The study complies with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies (von Elm et al., 2007). STROBE checklist is available as File S1.
4 RESULTS
We analysed 323 phone calls for a total of 171 patients. The majority (79.3%) were from outpatients, in particular 67.4% from those followed by the early PC outpatient clinic and 11.9% from individuals followed by the palliative radiotherapy one. The remaining 20.7% were composed of patients in transition to the territory, some already on the territory or patients from IRCCS Istituto Romagnolo per lo Studio dei Tumori cancer ward for whom CG called, generally for logistical needs concerning discharge and some waiting for a PC first visit. The majority of patients had an ECOG PS stated by a PC physician of 0–1 (53.9%) or 2 (39.2%). On average, each patient contacted us 2.7 times.
Patient characteristics are reported in Table 1. The majority of calls were made by male patients (61%), and for 40.6%, the ones who were calling were CG. The most prevalent cancer diagnoses were thoracic cancer (19.5%) and gastrointestinal cancer (24.2%). 70.8% of patients were plurimetastatic and 56.6% of patients were undergoing chemotherapy.
| Variable | No. | % |
|---|---|---|
| Median age, years (interquartile range) | ||
| <35 | 6 | 1.8 |
| 35–54 | 48 | 14.9 |
| 55–74 | 177 | 54.8 |
| >74 | 92 | 28.5 |
| Gender | ||
| Male | 197 | 61.0 |
| Female | 126 | 39.0 |
| Caller | ||
| Patient | 192 | 59.4 |
| Caregiver | 131 | 40.6 |
| ECOG PS | ||
| 0–1 | 172 | 53.9 |
| 2 | 125 | 39.2 |
| 3–4 | 22 | 6.9 |
| Missing | 4 | - |
| Cancer type | ||
| Thoracic | 63 | 19.5 |
| Upper gastrointestinal | 61 | 18.9 |
| Lower gastrointestinal | 17 | 5.3 |
| Prostatic | 47 | 14.5 |
| Breast | 44 | 13.6 |
| Genitourinary | 30 | 9.3 |
| Haematological | 20 | 6.2 |
| Rare tumour | 18 | 5.6 |
| Head and neck | 6 | 1.9 |
| Melanoma | 7 | 2.2 |
| Other | 10 | 3.0 |
| Metastasis | ||
| Single | 78 | 29.2 |
| Multiple | 189 | 70.8 |
| Missing | 56 | - |
| Ongoing treatment | ||
| Chemotherapy | 181 | 56.6 |
| Chemotherapy + radiotherapy | 8 | 2.5 |
| Chemotherapy + palliative radiotherapy | 11 | 3.5 |
| Radiotherapy | 6 | 1.9 |
| Palliative radiotherapy | 11 | 3.5 |
| BSC | 19 | 6.0 |
| FU | 19 | 6.0 |
| Diagnostic evaluation or re-evaluation | 61 | 19.1 |
| Other treatment (brachytherapy, hyperthermia, bone embolization) | 3 | 0.9 |
| Missing | 4 | - |
| Ongoing pain therapy | ||
| Adjuvant | 7 | 2.3 |
| Weak opioid +/−adjuvant | 19 | 6.1 |
| Strong opioid +/− adjuvant | 268 | 85.9 |
| Non opioid +/− adjuvant | 18 | 5.7 |
| Setting | ||
| Out-Patient | 256 | 79.3 |
| In-Patient | 6 | 1.8 |
| Territory | 11 | 3.4 |
| Waiting for territory charge | 40 | 12.4 |
| Waiting for first PC appointment | 10 | 3.1 |
| Timing from the last PC visit | ||
| <24 h | 5 | 1.6 |
| 24–72 h | 32 | 10.4 |
| 3–7 days | 48 | 15.7 |
| 7–15 days | 51 | 16.7 |
| 15–30 days | 55 | 18.0 |
| >30 days | 115 | 37.6 |
- Abbreviation: ECOG PS, Eastern Cooperative Oncology Group Performance Status.
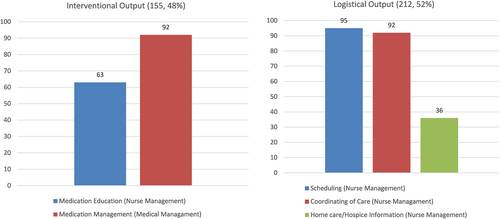
For the two main categories we grouped calls into (46.1%) or (38.7%). 15.2% of calls included both logistic and interventional requests. We created several sub-categories taking into account a total of 400 problems and 367 recommendations to better analyse the reasons for use of the service. 78.3% of calls were made to address one problem, 19.5% for two problems and 2.2% for three problems. The most frequent reasons for calls were uncontrolled pain (38.4%) and updates of the clinical situation (23.8%). 18.9% of calls were made for problems of medication management and 18.3% for scheduling.
A total of 367 recommendations were made, the most frequent for scheduling (29.4%) and medication management (25.5%) (Figure 1). We also analysed the management of phone-calls: 65% were handled by the case manager, 28.1% by a physician and 6.8% by the case manager and physician together. There was an 87.6% effectiveness of telephone management on the basis of the aforementioned 7-day criteria. 85.9% of the phone calls received in relation to pain medication were made for patients undergoing treatment with strong opioids.
5 DISCUSSION
In the present study, we described our experience of a nurse-led telephone program for early PC patients, part of an interdisciplinary care approach at IRCCS Istituto Romagnolo per lo Studio dei Tumori aimed at improving the QoL of patients and CGs. Our main aims were to assess the feasibility and impact of the service and to identify areas of the program requiring improvement. Some interesting studies on the use of nurse-led telephone care programs have been published over the past few years and during the COVID-19 emergency, all demonstrating the feasibility, effectiveness and appropriateness of such a service (Cox & Wilson, 2003; Suh & Lee, 2017; Torres-Vigil et al., 2021). The results from our preliminary observational study are in line with those of the literature, further confirming the efficacy of the initiative.
Case management is a means of ensuring continuity of care for patients with complex care needs. It is a heterogeneous term for care that consists of assessment, planning, implementation, coordination, monitoring of the options and services required to meet patient needs (Case Management Society of America, 2010). There are numerous models and variations in ways of delivering such care. We analysed nurse-led telephone case management, a less expensive and more accessible alternative to outpatient appointments for seriously ill patients.
Wang et al. (2015) concluded that PC case management may help reduce hospitalisation and increase referral to hospice in patients nearing death. However, further research is warranted to more clearly define its usefulness (Strupp et al., 2018). We hypothesized that the majority of phone calls from our patients could be managed by a trained nurse to resolve specific healthcare, organisational and administrative issues, thus reducing the need for access to the outpatient clinic. Furthermore, although nurses cannot substitute a physician from a clinical point of view, their empathetic skills, typical of this caring profession, contribute substantially to making patients feel ‘cared for’ (Strupp et al., 2018).
Over a period of 6 months, we registered 323 phone calls from 171 patients, the majority of whom were attending our early PC outpatient clinic and had an ECOG PS of 0–1 or 2. This attests our approach of promoting the early integration of palliative care for patients with advanced cancer. 40.6% of phone calls were from caregivers, indicating their importance in PC and highlighting the need for their presence during visits. This is in line with results from other studies reporting a positive impact of early PC on CGs and confirming that their active presence throughout the clinical trajectory positively impacts on patients (Case Management Society of America, 2010; Suh & Lee, 2017). Further research is warranted to explore the satisfaction level given by CGs with regard to such a telephone service and the extent to which it can affect their QoL.
The most frequent reasons for use of the telephone service were pain and medication management, in agreement with the results of the study by Pimentel et al. (2015). The problem of pain requires close follow-up, especially for patients where opioids, the most widely used drugs, often require dose changes. The usefulness of the telephone program is clear in that it represents a rapid and simple way of checking on patients and on pain medications, as also Zimmerman et al. suggested (Zimmermann et al., 2019). It is also easier for patients and caregivers to contact the PC team by phone rather than to wait for the next appointment, and at the same time, strengthens the sense of continuity of care. However, the present study has several limitations. The first one was its non-interventional retrospective nature, in that we did not use any instruments to evaluate symptoms or questionnaires to evaluate patient and CG satisfaction. Furthermore, patients undergoing PC are often unable to wait until the next outpatient appointment because of high symptom burden or may need logistics counselling to facilitate the management of their disease in a different setting. In fact, many of the needs assessed during phone calls were related to care coordination, such as appointment management or territorial case management. Our results highlighted the logistics nature of many of the needs expressed by patients and families, further confirming that a nursing case manager is the most suitable member of the PC team to undertake these tasks, enabling physicians to dedicate more time to clinical activities.
Furthermore, we did not provide written details about the availability of the telephone service, choosing to inform patients verbally of the initiative and to simply insert our contact details at the bottom of the referral. Another important bias concerns the fact that the study was activated during the COVID-19 pandemic, which may have increased telephone consultations and reduced physical access to IRCCS Istituto Romagnolo per lo Studio dei Tumori. Further research is needed to determine the real impact of the PC telephone service in a normal clinical setting.
6 CONLUSION
The results from our study confirmed that a PC telephone service run by a nursing case manager is a valid means of following patients and of supporting continuity of care in accordance with PC principles. The majority of problems were resolved over the phone, thus avoiding the need for patients to access the institute. In particular, our findings showed that the service can be managed solely by a PC nurse, freeing up more time for physicians to devote to clinical practice. Our program could be improved by creating a better awareness campaign about PC for patients and families. It would also be interesting to analyse patient and CG's satisfaction of the service, as well as its economic impact, measuring the effectiveness of the service. We are currently designing a non-pharmacological two-arm randomised control trial for patients followed by the early PC team at IRCCS Istituto Romagnolo per lo Studio dei Tumori. Validated tools will be included in both groups to assess patient and caregiver QoL and satisfaction, and they will receive flyers to advertise the service. The research arm will be able to take advantage of a proactive telephone service with follow-up every 7 days after the first early PC outpatient visit. Our aim is to obtain specific and measurable data on the differences between the two groups in terms of patient QoL, symptoms management, families' satisfaction and benefits in terms of cost (follow-up visits carried out telematically rather than in outpatient clinic) and time (reduction in waiting times for appointments and in time needed to resolve patient and CG problems).
7 RELEVANCE TO CLINICAL PRACTICE
An effective and feasible nurse-led telephone follow-up of early PC patients with advanced cancer can possibly dramatically improve their care experience, QoL and symptom control without travel or additional cost, securing access to timely care. The model can also improve continuity of care, adherence to oncological treatments and minimise acute care visits in a cost-effective way.
AUTHOR CONTRIBUTIONS
All of the authors conceived the idea for the paper and analysed and interpreted the data. The first draft of the article was written by VV, with revisions by RR and MM. All authors read and approved the final version of the manuscript for submission.
ACKNOWLEDGEMENTS
The authors are grateful to all patients for their participation in this study. We would also like to thank the editorial office for the support.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
Ethical statement
The study was approved by the Medical Scientific Committee and the Ethics Committee of our institute (IRCCS Istituto Romagnolo per lo Studio dei Tumori (IRST) “Dino Amadori”) (Approval no. 2837 of 06.11.2020) and conducted in accordance with the principles laid down in the 1964 Declaration of Helsinki and Good Clinical Practice guidelines. As this was a non-interventional study based on the secondary use of data collected for other purposes (retrospective observational study), individual informed consent was not required. The study complies with the STROBE checklist.
Open Research
DATA AVAILABILITY STATEMENT
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.