A new easy technique to identify the correct artificial hair implantation site: A case series and preliminary results
Beniamino Palmieri, Maria Vadalà and Al Bzour Bogdan Morad contributed equally to this work as co-first Authors.
Mariastella Di Carmine and Antonio Scarano contributed equally to this work as co-last Authors.
Abstract
Background
The implantation of artificial hair is a successful standardized procedure to restore bald areas or scarred alopecic surfaces of the scalp in both sexes.
Materials and Methods
Sebometric measurements were taken, pre, 1, 3, and 6 months postimplant in two symmetric frontotemporal areas of the scalp of seven volunteers to be implanted with 50 units of artificial hair. The artificial hair used in this study are Biofibre 4.0 produced by Medicap srl, Italy.
Results
The dermaroller assisted procedure was performed only on one side, and the plain random implant contralaterally for comparison. A marked downregulation of the sebum concentration was observed in the dermaroller treated area 1, 3, and 6 months later in respect to the control side.
Conclusion
The dermaroller assisted procedure is safe and effective in reducing the foreign body reaction by the sebaceous glands and the vascular axis injured by the implanting needle; a longer standing success of the implanted hair can thus be achieved reducing the burden of inflammatory reaction.
1 INTRODUCTION
Androgenic alopecia occurs when the normal repopulation of hair is disrupted in the location of the frontotemporal, sparing the occipital scalp and was classified by Nordwood.1 Alopecia, particularly in women, causes a strong impact on the quality of life and on self-esteem, and there is a critical need for treatment. Different therapeutic strategies are used for the treatment of alopecia such as medical, phototherapy, stem cells, micropigmentation, and surgical approaches.2, 3 Today, autograft hair transplantation is the gold-standard surgical treatment for alopecia and includes transplantation of hair bulbs from the occupational zone to the frontotemporal areas.4 Additionally, autologous hair transplantation is contraindicated in alopecia areata because the organ-specific autoimmune reaction affects the transplanted hair.5 Synthetic hair fibers have been proposed for treating patients without adequate donor hair, patients with alopecia areata, scars, and possibly cicatricial alopecia. Different materials have been used to construct synthetic hair such as polyester, monacrylic, and polyacrylic. Nowadays, hair in polyamide material is claimed to be inert and safe.
The success of hair transplant surgery is largely dependent on a complete understanding of male pattern baldness and a proper patient selection. Synthetic hair implants are proposed in alopecia when the patient has a poor donor area or requests a non-invasive approach with minor surgery and immediate result.
The proper choice of the artificial hair implantation site is critical for the successful long standing and uneventful maintenance of the implanted fiber across the scalp.6-9
In routine practice, each individual artificial hair is regularly implanted along definite lines by the medical operator whose primary attention is on selecting the right distance in between each fiber and the proper penetration angle to achieve an appealing, natural cosmetic appearance of the refurbished scalp. The technique, by trained and qualified doctors, is minimally invasive and requires quite a short learning curve; the cosmetic results are very appealing, and the loss of the artificial hair does not usually exceed 10% per year. The autologous dermal reaction to the artificial hair implant, is in some cases a result of a condensation of sebaceous secretions that, melted with exfoliated epithelial cells, may produces black spot and irritation phenomena around the skin output of the implanted hairs; if neglected the subsequent inflammatory reaction can affect the long-term implants' engraftment. In some cases, they are implanted in the sebaceous glands which causes excessive production of sebum, temporary superficial infection or inflammation that usually subsided within 15 days or causes a failure of the implant.6, 10, 11 For this reason, the guidelines of the post-treatment follow-up recommend regular hygiene and cleanliness of the scalp. The hypothesis of the present clinical pilot study is that artificial hair aside from the pilosebaceous unit, identified with dermaroller pass, reduces the amount of the sebum over the scalp in the postoperative follow-up.
The aim of the present study is to avoid the artificial hair unit's insertion across the sebaceous glands by use of the dermaroller.
2 MATERIALS AND METHODS
Seven male patients affected by androgenetic alopecia who had undergone synthetic hair implants were treated with artificial hair. All patients signed the informed consent. The procedure fulfilled the ethical lines being a minor variation of the world widely approved artificial hair implantation standard method and conducted in compliance with the local Good Clinical Practice procedures for quality control.12 One split parietal temporal was treated by broadband light (BBL), another split-face was untreated as a control and skin sebum excretion was evaluated by using the SebumScale®, according to the manufacturer's instructions. The contralateral side showed on the contrary some asymptomatic scanty punctiform not inflamed skin ripples and bulging, presumably due to mesenchymal cell chemotactic pooling as a very early uneventful reaction to foreign material. The right mild-parietal was treated with derma roll technique, while the left mild-parietal was treated with random technique and was used as control.
The skin sebum evaluation of the patients was performed by means of SebumScale® (Delfin Technologies, Kuopio, Finland), a non-invasive instrument based on a quartz crystal sensor that absorbs and measures the amount of sebum accurately in micrograms per 1 cm2 (0–150 μg/cm2), with a time of 5 s (Figure 1). In the specific, this measures the sebum by analyzing changes in the resonance frequency of the quartz crystal. Moreover, SebumScale® has been widely used in some studies, including an analysis of skin sebum excretion performed on seven patients who received treatments with broadband light (BBL) at 2-week intervals.13 The experiment was conducted in an air-conditioned, clean room to reduce the impact of confounding variables, including an ambient temperature, humidity, and hormonal balance.14 Usually, sebum recovery takes approximately 2–3 h after washing to the casual level15; therefore, the period of 4 h was set to cover the period of sebum recovery. All measurements were made on the forehead and at two sites lying symmetrically and over the mid-frontal hair line. The value of sebum (expressed in SebumScale® units from 0 to 150, approximated to μg/cm2 in a certain range) is the arithmetic mean of 3–5 repetitive measures in the same area.

- Basic Sebometric level in both the areas to be treated (Figure 2),
- Prolonged regular disinfection.
- Preliminary local epidermic anesthesia (EMLA or lidocaine cream) administration.
- Loco-regional subdermal (1% xylocaine without adrenaline) anesthesia (31G needle 3 mL) into the symmetric frontotemporal areas to be restored with artificial hair.
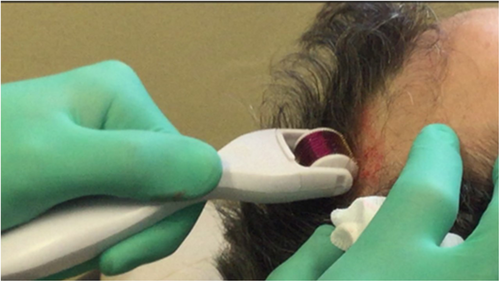
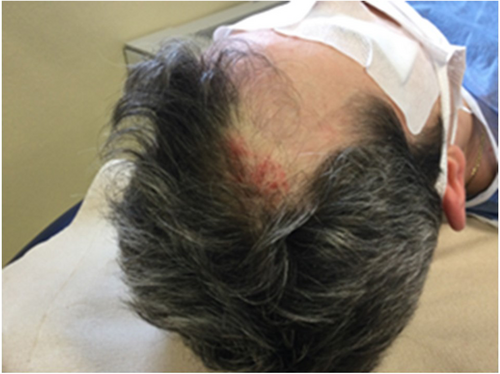
- On the right side, the surgeon passed with rotating dermaroller a device, 2.5 mm needle length, transfixing the skin surface along parallel rows 2–3 millimeters apart; rolling was done 3 times in horizontal, vertical, and oblique directions pressing over the scalp with adequate strength to introduce the tip of the needle through the epidermal layers down to the dermic papillae (Figures 3 and 4).
- The bleeding spots were stopped with an adrenaline 1 mg + epsilon aminocaproic acid mg embedded sponge pressed over for 3–5 min but were visible due to the microclots.
- 50 artificial hairs were then implanted into the avascular areas in between the clotted tips (Figure 5).
- On the LEFT side, 50 artificial hairs were implanted without using the dermaroller.
- The patients were medicated and discharged after careful instructions about the hygienic management of the scalp.


2.1 Technical characteristics of dermaroller
The dermaroller is an easy and cheap disposable instrument currently used by dermatologists and aesthetic doctors for wrinkles, face rejuvenations, acne and also alopecia. First described by Orentreich in 1995 for the use of wrinkles and atrophic scars.16
The standard dermaroller a drum-shaped roller studded with 192 fine microneedles in eight rows, 0.5–1.5 or more, mm in length and 0.1 mm in diameter. The microneedles are synthesized by reactive ion etching techniques on silicon or medical-grade stainless steel. The instrument is presterilized by gamma irradiation. Medical dermarollers are for single use only.
The procedure involves the use of a micro-needling device to create controlled skin injury. There are various skin needling devices including Dermaroller® (Dermaroller GmbH); Dermapen™ (Equipmed, Australia) Derma-Stamps™ (Dermaroller, USA) and radial disks incorporating fine microneedles of various diameters and lengths, fabricated from a wide range of materials such as silicon, glass, metals, and polymers. As each fine-needle punctures the skin, it creates a channel or micro-wound. The controlled injury triggers the body to fill these micro-wounds by producing new collagen and elastin in the papillary dermis.
Immediately after the micro-needling, some moderately bleeding holes appear on the skin surface whenever the roller needles randomly intercept dermal capillaries; easy hemostasis is thus achieved with cold wet adrenaline embedded sponge compression in 1 min. Subsequently, the hair is implanted skipping the bleeding holes 2–3 mm far around them.
The artificial hair is then implanted aside to the coagulated microvessels, previously identified by the dermaroller pass: So, the implant inserted into an avascular plain achieves a better biocompatibility reducing the chance of chemotactic risk by neutrophils and lympho-monocytes from the injured micro vessels and triggering a slight encapsulating activity by the fibroblasts with or without minimal involvement of cell mediated inflammation. Postimplant treatment requires the use of minocycline (100 Mg) for 7 days and local disinfectant (bacitracin, fusidic acid) and also an antiseptic shampoo each other day for a week.
2.2 Statistical methods
The study data were elaborated through the statistical software package GraphPad 8 (Prism, San Diego CA USA). The descriptive statistics was performed calculating the means, standard deviation, standard error, and 95% of confidence intervals of the sebum content measured at the baseline (T0), at 1 month from the treatment (T1), at 3 months (T2), and 6 months follow-up (T3). Due to the reduced sample size, the analytic procedure considered the using of non-categorical approach using the Friedman followed by Dunn post hoc test for repeated measurements to evaluate longitudinally the study findings. The Kruskal–Wallis followed by Dunn post hoc test was applied to compare the different anatomical sites effectiveness at all study timepoints.
3 RESULTS
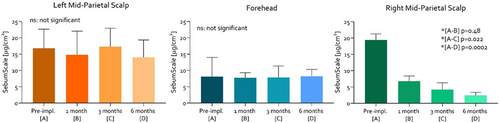
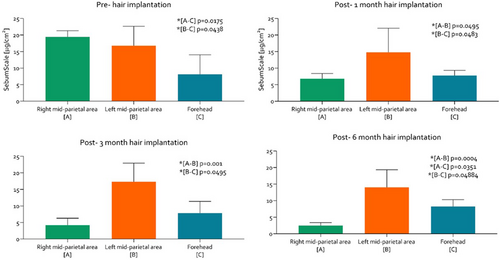
The operative step with a dermaroller was easy, quick, and uneventful. Infectious or inflammatory complications after hair implantation were 14.29% (1 patient) and involved only the left control area. This complication was mild and treated with local and systemic therapy which did not require the extraction of fiber. The measured skin sebum levels evidenced a significant reduction on the right skin area after 3 and 6 months by hair implantation. The sebum content revealed a significant reduction at the level of the right mid-parietal area of the scalp (Table 1) comparing the T0 and T1 (p = 0.48), while the levels were maintained at similar levels comparing T1, T2, and T3 (p > 0.05) (Figure 6). The sebum assessment revealed no significant difference in the left mid-parietal area of the scalp (Table 2) comparing the T0, T1, T2, and T3 (p > 0.05) (Figure 6). Similar findings were detected evaluating the forehead region that seems to produce no significant difference in sebum contents comparing the timepoints evaluated (p > 0.05) (Table 3; Figure 6).
| Sebum content [right mid-parietal area] | ||||
|---|---|---|---|---|
| Pre-impl. [T0] | 1 month [T1] | 3 months [T2] | 6 months [T3] | |
| Mean | 19.46 | 6.800 | 4.229 | 2.471 |
| SD | 1.837 | 1.592 | 2.078 | 0.8958 |
| SE | 0.6945 | 0.6016 | 0.7855 | 0.3386 |
| Lower 95% CI | 17.76 | 5.328 | 2.307 | 1.643 |
| Upper 95% CI | 21.16 | 8.272 | 6.151 | 3.300 |
| Sebum content [left mid-parietal area] | ||||
|---|---|---|---|---|
| Pre-impl. [T0] | 1 month [T1] | 3 months [T2] | 6 months [T3] | |
| Mean | 16.79 | 14.79 | 17.30 | 14.03 |
| SD | 5.867 | 7.277 | 5.644 | 5.311 |
| SE | 2.217 | 2.750 | 2.133 | 2.007 |
| Lower 95% CI | 11.36 | 8.056 | 12.08 | 9.117 |
| Upper 95% CI | 22.21 | 21.52 | 22.52 | 18.94 |
| Sebum content [forehead region] | ||||
|---|---|---|---|---|
| Pre-impl. [T0] | 1 month [T1] | 3 months [T2] | 6 months [T3] | |
| Mean | 8.129 | 7.786 | 7.871 | 8.243 |
| SD | 5.879 | 1.533 | 3.523 | 2.085 |
| SE | 2.222 | 0.5796 | 1.332 | 0.7880 |
| Lower 95% CI | 2.691 | 6.368 | 4.613 | 6.315 |
| Upper 95% CI | 13.57 | 9.204 | 11.13 | 10.17 |
At the T0, lower sebum content was detected in the forehead region with a mean of 8.129 ± 5.879 μg/cm2 compared to the right mid-parietal (p = 0.0175) and left mid-parietal region of the scalp (p = 0.0438), that were, respectively, 19.46 ± 1.837 μg/cm2 and 16.79 ± 5.867 μg/cm2. After 1 month from the treatment (T1), the sebum content measurement at the level of the right mid-parietal, left mid-parietal region of the scalp and forehead region were, respectively, 6.800 ± 1.592 μg/cm2, 14.79 ± 7.277 μg/cm2, and 7.786 ± 1.533 μg/cm2. A significant difference was detected comparing the left mid-parietal region with the right mid-parietal (p = 0.0495) and forehead (p = 0.0483). No difference was detected between forehead and right mid-parietal region. At 3 months from the hair implantation (T2), similar findings were detected comparing the left mid-parietal region with the right mid-parietal (p = 0.0001) and forehead (p = 0.0495) that were, respectively, 17.30 ± 5.644 μg/cm2, 4.229 ± 2.078 μg/cm2, and 7.871 ± 3.523 μg/cm2. After 6 months follow-up (T3), a significantly lower sebum content was detected comparing the right mid-parietal area with the left mid-parietal region (p = 0.0004) and the forehead (p = 0.04884). In addition, the left mid-parietal region showed a significant difference compared to the forehead area (p = 0.0351). The mean sebum contents of the right, the left mid-parietal region, and the forehead were, respectively, 2.471 ± 0.8958 μg/cm2, 14.03 ± 5.311 μg/cm2, and 8.243 ± 2.085 μg/cm2 (Figure 7). In the specific, a reduced sebum was observed in the right mid-parietal areas of the scalp from 20% to 60% (respectively, pre-hair implantation and after 6 months from treatment).
In the follow-up at 3 and 6 months of the implant procedure, the dermaroller implanted site showed, at dermatoscopic magnification (20×), a perfectly smooth skin surface, without any reaction into or around the newly formed artificial follicles; the contralateral side showed, on the contrary, some asymptomatic scanty punctiform not inflamed skin ripples and bulging, presumably due to mesenchymal cell chemotactic pooling as very early uneventful reaction to foreign material.
4 DISCUSSION
The results of the present study showed the reduction of sebum in the right mid-parietal areas of the scalp from 20% to 60%, pre-hair implantation and after 6 months from treatment, respectively. Reduction of sebum is essential for avoiding infection and loss or fiber extraction. Usually, poor quality fibers, multiple fibers in one hole, implanted too close or too shallow and non-flexible increase the percentage of adverse reactions.17 For successful artificial hair implantation, it is important to implant in the sebaceous glands which causes excessive production of sebum, temporary superficial infection or inflammation that usually subside within 15 days or cause a failure of implant.6, 10, 11
In the present study, our main concern has been that, in the bald areas to be restored, the vascular axis of the dropped hair follicles and the alleged sebaceous gland did not undergo atrophy; therefore, if the artificial hair is randomly implanted across these sebo-vascular spots, the body reaction will be increased, accelerating the drop out of the subdermal root anchoring the artificial hair.
Our technique has thus been planned, in order to insert the artificial hair into sub-epidermal specific spots bare of vessels, nerves, and sebaceous glands; these selected spots are quite far from the capillaries which have not to be injured by the implanting needle causing extravasation of erythrocytes, leucocytes, platelets, and inflammatory cytokine pooling in the dermis.
Our endeavor to reduce the amount of sebum, caused us to design a specific operative strategy aiming at avoiding the artificial hair unit's insertion across the sebaceous glands, and the vascular axis of the previously existing hair bulbs. Distinguishing the bleeding points helps the operator to implant the artificial hair preferably into the dermic avascular spots in between, identified by a previous pass of a dermaroller. This avoids inserting hairs into the vessels, which would trigger a foreign body reaction. The dermaroller is a multi-needle rolling cylinder used to scarify the skin causing oozing from the dermal capillaries transfixed by the needles. The dermaroller unmasks the dermal capillaries intimately enveloped by the sebaceous glands, and the operator is able to safely implant the artificial hair units in the avascular spaces aside to them.
The advantage of such a method is to prevent early or delayed phlogistic reactions involving the implants and the engorgement of the epidermal artificial holes, by sebaceous material, reducing the complication rate and eventually the implant drop out.
The dermaroller has been proven as a reliable instrument to show the topography of the dermal vessels, nourishing the pilosebaceous apparatus, and still viable after the bulb cells apoptosis. The dermaroller stings the vessels, and accordingly to its anti-aging/bio-revitalizing function, makes them bleed and clot rendering them visible to the operator.
Micro-needling (MN) is a minimally invasive procedure involving the induction of percutaneous channels-shaped micro-wounds achieved with 0.25–5.00 mm medical-grade needles; it is well tolerated by the patients and very rarely induces short term erythema which does not require any treatment and spontaneously subsides; the procedure releases platelet-derived growth factor and vascular endothelial growth factor to promote wound-healing responses, improve angiogenesis, and attenuate or partially reverse fibrosis resulting from acute injury and skin aging.16-18
This technique has already been used in the scalp area to counteract the baldness.
English and co-workers19 synthesized 22 clinical studies enclosing 1127 subjects with different kinds of alopecia submitted to micro-needling as an adjunct therapy; androgenic alopecia and alopecia aerate achieved good improvement of hair loss parameters and were variously matched with standard minoxidil, prp, CO2 laser, and other topical administrations the authors state that.
Notwithstanding the evidence that micro-needling might improve the hair loss, the clinical data reported are of quite low quality, due to wide heterogeneity among procedures, interventions, and comparators. With better study designs and efforts to standardize best practices, micro-needling could become an FDA-approved hair loss treatment.
Our study emphasizes the safe and effective strategy of micro-needling in the trichological field, and, based on this report, our original extended use of dermaroller in the artificial hair implantation procedure might give putative potential benefits also to the regrowth of natural hairs; our limited application, however, is exclusively intended to correctly insert the hair units aside to the pilosebaceous vascular structures, identified by the micro-needling, avoiding injury to the sebaceous glands; striking different sebum concentrations have been recorded comparing the dermaroller pre-treated area, and the contralateral one where the implants have been randomly anchored without previous micro-needling which is more prone to cause reaction across the injured glands. This very simple trick is minimally time consuming, but advantageous in terms of reducing the sebum overproduction, risk of inflammatory response, and eventually the drop out of the implants.
In fact, the literature investigations17 describe approximately 95%–98% satisfaction rate among patients,7, 8, 18, 20 but 9.7% reported mild and moderate inflammatory, or infectious complications, mainly caused by lack of proper after care from the patients, requiring antibiotic and steroid therapy to be solved. Fiber removal was necessary in 2% of the cases.7, 8, 18, 21 Infections are mainly caused by Staphylococci aureus and epidermidis, Streptococcus pyogenes, and corynebacterium. Inflammatory complications are described as mild reddening and itching.22 Histologically at 12–18 months showed fiber surrounded by fibrosis and collagen.23 No pigment was seen although the modifications vary depending on the anatomical structures in the path of the fiber, the inflammatory phenomena were extremely limited and did not produce clinically evident signs of inflammation.17 Respect of correct patient selection, correct implant procedure, and proper after care is fundamental to avoid prospective problems.22, 24, 25 The present artificial hair implant results26 are very far from the old technique of 80′-90′ which reported, in some cases, foreign body reactions also causing severe adverse events, including recurrent folliculitis, scalp crusting, scarring, the matting and breakage of fibers, and granulomatous reactions. The onset ranged between 1 and 8 weeks of a hyperplastic proliferation of epidermal cells, foreign body granuloma, and persistent acute inflammation due to bacterial infections.27 We have been acquainted with the role of the sebum in inducing inflammatory reaction around the skin outcrop of the artificial hair shaft; for this reason, we took the challenge to analyze whether the implant technique might be somehow modified, reducing the chance to damage the sebaceous glands and to elicit foreign body reaction.
The use of a dermaroller preliminary to the seeding procedure of the hair units is easy, cheap, and very little time consuming, and should be endorsed as a routine step; prospectively the micro-needling might also be used in routine postimplant check-up sessions to revitalize and better balance the scalp metabolism and natural hair regrowth. In conclusion, our clinical study fulfills the proof of the concept that implanting the artificial hair aside from the pilosebaceous unit, identified with dermaroller pass, downregulates the amount of the sebum over the scalp in the postoperative follow-up. Currently, the implantation of real hair is considered a gold standard, and the use of artificial hair remains a viable alternative.
AUTHOR CONTRIBUTION
BP, AS, and MV: Conceptualization, methodology, software, validation, resources, project administration, and funding acquisition. BP, AB, MD, and MV: Formal analysis. BP, MV, AB, and AS: Investigation. AS: Data curation, and writing—original draft preparation. BP, AS, MV, and AB, Writing—review and editing. AS, MD, MV, and AB: Visualization. AB, MV, and AB: Supervision.
ACKNOWLEDGMENTS
The authors declare no conflict of interest for the present research. Open Access Funding provided by University of Chieti-Pescara, Italy, within the CRUI-CARE Agreement.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest for the present research.
ETHICS STATEMENT
The authors confirm that the ethical policies of the journal, as noted on the journal's author guidelines page, have been adhered to. The study was based in the Department of Innovative Technology in Medicine and Dentistry of the University “G. d'Annunzio” of Chieti-Pescara in Italy, in full accordance with ethical principles, including the World Medical Association Declaration of Helsinki (https://www.wma.net/ wp content/uploads/2018/07/DoHOct2008.pdf) and the additional requirements of Italian law. All patients signed informed consent on the adopted procedure.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.