Contour first—retrospective study of an algorithmic approach of auricular keloids
Huanhuan Wu and Guoxuan Dong authors contributed equally to this work.
Abstract
Background
Auricular keloids are difficult to treat, and recurrent keloids are more aggressive and more likely to develop aural deformities. Surgical excision, injections, or radiotherapy alone have high recurrence rates. An algorithmic approach of auricular keloid remains to be explored.
Aims
To investigate the sequential treatment protocol for the treatment of auricle keloids to maintain auricle morphology and reduce the postoperative recurrence rate.
Patients/Methods
A retrospective analysis of 42 patients who attended the scar minimally invasive treatment center of the Hospital of Plastic Surgery, Chinese Academy of Medical Sciences for serial treatment from January 2019 to June 2021. According to the size and involvement of the keloid, the core excision of the scar was excised under the condition of ensuring the priority of the auricular contour, and the scar flap was repaired to reconstruct the auricular appearance, and electron beam treatment was performed within 24 h after the operation, ray energy: 6–7 MeV, dose: Dt18Gy/2f; regular trimethoprim combined with 5-Fu injection treatment and the application of silicone ear clips for local compression treatment were performed 1 month after the operation.
Results
Thirty-five patients were followed up from 12 to 40 months after surgery, and three of them showed a tendency of recurrence, and early local treatment with trimethoprim and 5-Fu injection achieved favorable results.
Conclusion
A standardized and sequential treatment plan for keloids with different morphology and anatomical locations can achieve remodeling of the auricular morphology and maintain long-term results.
1 INTRODUCTION
A keloid is a particular pathological scar that typically appears on the anterior sternum, upper back, ears, and shoulders.1 Keloid scars can develop spontaneously or as a result of skin trauma. Clinically, it is distinguished by an ongoing expansion of hard, encrusted nodular, striated, or lumpy tissue that goes beyond the initial skin lesion.2 Auricular keloids are difficult to treat because of their three-dimensional and exposed shape, and they frequently result in deformities that have an impact on the patient's appearance and even social life3, 4 Surgical excision, injections, or radiotherapy alone have high recurrence rates. Recurrent keloids are more aggressive and more likely to develop aural deformities. The goal of treating auricular keloids is to minimize appearance loss, increase recurrence rate reduction, and as much as possible restore the patient's ear to its normal appearance. From 2018 to 2021, our center has applied the auricular contour priority—Algorithmic treatment concept to provide comprehensive treatment for auricular keloid with 12–40 months of postoperative follow-up, with excellent clinical results, which are reported below.
2 MATERIALS AND METHOD
2.1 Patients information
From January 2019 to June 2021, 61 auricular keloids on a total of 42 patients underwent sequential therapy at our center. Postoperative pathology revealed keloids in all cases. To date, a total of 35 patients have been followed up for 12–40 months, with a median follow-up time of 18.5 months. There were 30 females and 5 males, aged 19–50 years, with a median age of 29 years. Table 1 contains statistics on disease causes, location of onset, family history, and additional sites involved. Exclusion criteria were as follows: (1) those with severe systemic disease; (2) those who were pregnant or breastfeeding, with a requirement for childbirth within 1 year; (3) those who required a guarantee that the keloid would not recur after surgery; (4) those who did not receive postoperative drug injections or had contraindications to drug injections; and (5) those who did not receive postoperative radiotherapy or had contraindications to radiotherapy. All patients were thoroughly informed of the treatment plan and the various possible complications, signed the relevant informed consent forms, and complied with the Declaration of Helsinki.
| Classification | Number of patients | |
|---|---|---|
|
Age |
<18 years | 0 |
| 18–30 years | 21 | |
| >30 years | 14 | |
| Gender | Male | 5 |
| Female | 30 | |
|
Family history |
Yes | 7 |
| None | 28 | |
|
Etiology |
Idiopathy | 1 |
| Trauma | 5 | |
| Piercing | 29 | |
|
Site |
Left side | 16 |
| Right side | 14 | |
| Bilateral | 5 | |
|
Location |
Earlobe | 17 |
| Helix | 16 | |
| Scaphoid fossa | 2 | |
|
Additional parts involved |
None | 26 |
| Torso | 7 | |
| Extremities | 1 | |
| Perineum | 1 | |
3 METHOD
3.1 Surgical treatment
A customized surgical strategy is used to establish bilateral symmetry wherever possible, depending on the size and shape of the keloid. The incision is designed with regard to the size and proportions of the opposing auricle.
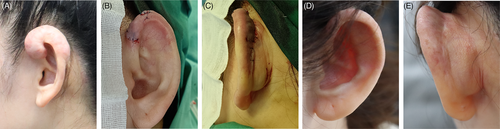
3.1.1 Earlobes
If a single keloid is present on either the front or rear of the earlobe, or present on both the front and back of the earlobe, and it has clear borders and does not significantly impact the size of the earlobe contour, it can be excised using a pike excision with complete excision of the keloid tissue via the front and back, using tension-free sutures to trim the wound margins. If the keloid on the earlobe is substantial, it can be removed by making a curving incision at its base, removing its core, leaving the keloid flap to cover the wound, and then tightly suturing it.(Figure 1A–C).

If there is a large number of keloids in front of and behind the earlobe, and the earlobe is severely distorted, direct excision and suturing will result in a malformed earlobe. To keep the patient's earlobe substantially symmetrical with the contralateral earlobe, the length and width of the contralateral earlobe must be measured before surgery. The defects were closed with Z-plasty or local flap transfer.(Figure 1D–F).
A recurrent earlobe keloid has a widespread growth of the entire earlobe and no discernible boundary separating it from normal skin. Before surgery, the earlobe on the opposite side is measured for length and width. A curved earlobe flap is then built behind the earlobe, the keloid is removed from the core, and the earlobe flap is folded posteriorly and superiorly to remove the extra skin and create a new earlobe.
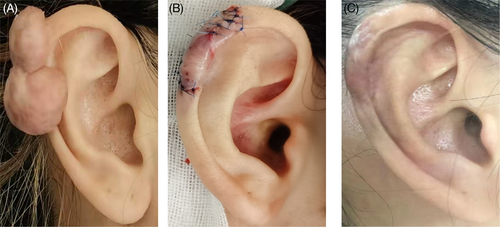
3.1.2 Helix
The helix is a significant aesthetic feature of the ear; thus, it is crucial to handle keloids at the helix. The contour line of the auricular rim and the visual appeal of the ear will be altered if the keloid is directly removed and sutured. A curved incision at the base of the postauricular keloid can be utilized to totally remove the core of a single keloid at the helix while perfectly retaining the thin keloid flap. The keloid is first entirely removed from the auricular cartilage; then, the membrane covering the auricular cartilage is used to cover the wound and apply the keloid flap to restructure the auricle.
Recurrent keloids at the auricular rim frequently appear with significant auricular deformity, a history of multiple auricular keloid excisions, a lack of clear demarcation between the keloid tissue and the auricular cartilage, and complete coverage of the auricular rim in keloid tissue. A keloid core excision is employed for this specific type of keloid, and an auricular mold made in accordance with the shape of the contralateral auricle is created prior to surgery. The ear canal and ear wheel are exclusively covered, and oiled gauze rolls have been used to fill and crush the canal (Figure 2).

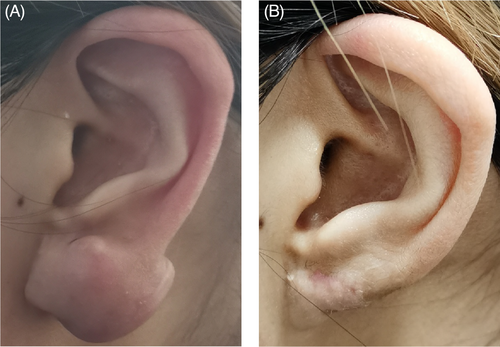
Scaphoid Fossa and postauricle area.
If the keloid develops simultaneously on the scaphoid fossa and postauricle region, it should be excised using a curved incision along the keloid's base that is divided from the front to the center and connected anteriorly and posteriorly. If the keloid is excised in the navicular area and sutured directly to the ear, it is easy to develop an adhesive band around the ear wheel and navicular, which affects the shape of the ear. As a result, the keloid should be excised from the core of the keloid and the scar flap utilized to patch the incision, totally maintaining the skin of the ear canal and avoiding the appearance of an adhesive pull on the ear canal, which could impair the three-dimensional structure of the ear canal. (Figure 3).
3.2 Postoperative sequential therapy
3.2.1 Electron beam radiation therapy
Patients are treated with 6–7 MeV electron beam radiation therapy within 24 h of surgery, using the Elekta Versa HDTM electron linear accelerator. Patients are first instructed to adjust to a suitable position so that the irradiated area is kept in the same plane as the patient as far as possible, and the irradiated surface is covered with a 0.5 cm equivalent film. The radiotherapy treatment should be centered on the surgical incision and spread outwards by 1 cm, with a radiation dose of Dt18Gy/2f and Biologically Effective Doses (BED) values up to 30-40Gy, in two sessions with an interval of about 1 week. It is critical to change the dressing on time after each radiotherapy treatment to avoid infection.
3.2.2 Local compression therapy
Seven days following the procedure, the stitches are removed. A magnetic ear stud or a silicone nasal clip can be used for compression 7 days after the stitches are removed. Compress for 6–8 h each day, take a break for 30 min after 2 h of continuous compression, then continue compressing for another 6 months.
3.2.3 Drug injection therapy
Low concentration of 5-FU injections (0.5% lidocaine:5-FU = 1 ml:0.1 ml) are given 1 month after surgery, subject to the skin color at the injection site becoming lighter and whiter, once every 4 weeks, for a total of 3 injections after surgery. If the area becomes hard in texture, treatment is given by triamcinolone acetonide: 0.5% lidocaine:5-FU injection (1ml: 2 ml: 0.1 ml).
4 RESULTS
The three grades classification method5 is used to evaluate the treatment's effectiveness. The following indications indicate that the condition has been cured: satisfactory auricular appearance, eradication of the itching and pain symptoms, flattening and softening of the keloid, normal skin tone, and no recurrence for more than a year during follow-up. Significant effect: The appearance of the auricle was basically satisfactory, the self-conscious symptoms disappeared, the scar softened by 60% ~ 70% and became flat, and no recurrence was observed during the follow-up of more than 12 months. Ineffective: patients who felt pain and itching symptoms, keloid appearance and texture did not see significant improvement, or recurred within 12 months after treatment. On a scale of 1–10, patients' subjective assessments of their subjective satisfaction with the overall treatment outcome and the treatment process were tallied.
A total of 35 of the 42 patients were followed up postoperatively, with a missing rate of 16%, of which 31 were cured, one was effective and three were ineffective, with recurrence occurring at 7, 14, and 15 months postoperatively, respectively. The overall efficiency of treatment reached 91.4%, with a mean patient satisfaction score of 9.71.
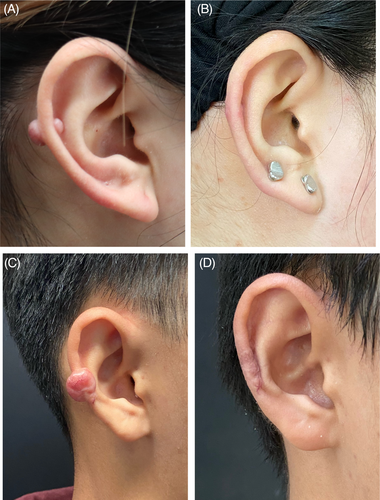
4.1 Typical cases 1
A 27-year-old female has had a keloid in her right ear for more than 2 years after having her ear pierced. The keloid grew significantly during her pregnancy a year ago, and she was treated with an external excision before coming to our clinic 6 months later. The keloid was excised from the core of the scar, leaving intact the ear cartilage and a small amount of softened keloid flap to facilitate shaping and suturing, with appropriate trimming of the keloid flap and tension-free suturing. Postoperative radiotherapy and injections were completed routinely, and there was no tendency for recurrence at 1 year follow-up (Figure 4).
4.2 Typical cases 2
A 31-year-old female patient suffered from left earlobe keloid for more than 5 years. The keloid core was excised, and the earlobe was reshaped by a keloid flap with good morphology. After 6 months of follow-up, there was no recurrence tendency (Figure 5).
4.3 Typical cases 3
A 23-year-old female patient suffered from right keloid located at helix and a recurrence keloid located at postauricle area (Figure 6).
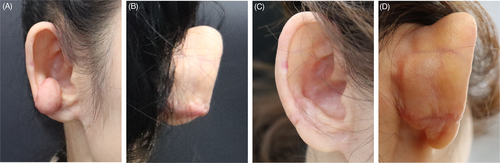
4.4 Typical cases 4
Showed auricular keloid located at auricular rim (Figure 7).
5 DISCUSSION
Keloidectomy is the primary therapeutic choice for auricular keloids,6 but the auricle structure is complicated, and incorrect healing of auricular keloids after excision has been clinically shown to result in auricular deformity; thus, core excision is recommended for auricular cartilage keloids. The recurrence rate of single excision can be 45–100 percent. Adjuvant therapies such as steroid injections, radiotherapy, and laser combined with core resection have yielded promising results in the recurrence rate and auricular contour. We summarize the clinical manifestations of primary and recurrent keloids in different locations of the auricle, and propose corresponding surgical options to preserve the appearance of the auricle.
A rounded and full earlobe is considered to be more fortunate in Chinese aesthetics. In the case of auricular keloids with first surgery, when obvious boundaries between the keloid and normal skin or a narrow keloid base was observed, a transverse shuttle incision can be designed to completely remove the keloid tissue, and longitudinal excision with longitudinal sutures should be avoided. It is advised to utilize a horizontal pike incision to excise and suture the earlobe without compromising its width because after longitudinal excision and suturing, the width of the earlobe grows narrower and the length becomes longer, giving the appearance of a long and thin earlobe that is not in accordance with the traditional earlobe aesthetic. Direct pulling together of the sutures will result in a distorted earlobe in cases of significantly deformed earlobes with keloids, leaving a huge through defect in the earlobe. In this scenario, a local flap reshaping needs to be designed to restore continuity and fullness to the edge of the earlobe. In initial or recurrent auricular keloids that are greatly enlarged and have a wide base, complete excision of the keloid makes trauma repair difficult, and direct pull-together sutures can easily lead to a deformed earlobe; the use of a nearby tipped flap or free flap to repair the trauma decreases the damage to the donor area. The keloid epidermal flap is commonly utilized in clinical practice due to its simplicity, ease, and sufficient amount of donor skin. It effectively eliminates incisional suture tension, reduces the possibility of postoperative recurrence, and also prevents the creation of new incisions, making it especially appropriate for larger ear keloids. When weighing auricle morphology restoration vs. the possibility of total excision of pathological tissue, we prefer those that preserve the appearance of the ear morphology, retain some of the scar core flap as an ear support structure, and retain the scar epidermal flap for tension-free wound recovery. A relative balance between “scar removal” and “auricular form restoration” can be achieved by using subsequent treatment to eliminate some of the remaining diseased tissue. In this study, only three patients who underwent primary auricular keloid surgery suffered postoperative recurrence, while none of the patients with partial scar skin retention had recurrence after surgery by core excision of the keloid. Similar findings have been made by domestic and foreign authors,7 According to Ogawa et al., the epidermis and dermal papillae were the only parts of the scar skin that thinned following “core excision,” which did not increase the recurrence rate by leaving behind some of the scar skin and resulted in a recurrence rate8, 9 that was statistically identical to that of “complete excision.” The recurrence rate is statistically identical to that of “complete excision.” Therefore, for keloids of various morphologies and anatomical locations, we employ a standardized and individualized sequence of treatments. The keloid is specifically chosen for “complete excision” or “core excision,” and the wound is then repaired with tension-free sutures.
We utilize a sequential therapy strategy of radiation combined with local compression and drug injections after excision, which contains first electron beam irradiation within 24 h after surgery, second irradiation around 1 week after surgery, local compression using magnetic sheet ear staples after removal of the stitches, and low concentration drug injections to lower the recurrence rate of keloids. A variety of factors influence radiation regimens and outcomes, including the date of treatment beginning, dose, and treatment method.10 Early radiotherapy after keloid surgery has been demonstrated in studies to suppress fibroblast proliferation, induce apoptosis, and considerably lower recurrence rates. In light of this, radiation administered within 24 h of surgery has recently gained widespread acceptance. The radiotherapy break encourages the transformation of radiation-tolerant fibroblasts into radiation-sensitive fibroblasts while allowing normal skin cells to recover.11, 12 Two radiation treatment techniques are suggested13, 14 based on our clinical practice experience and pertinent literature: (1) the use of multiple fractionation and (2) less fractionated mode. The total dosage is controlled at 17.5–20 Gy and completed in 4 ~ 5 sessions. 18 Gy was accomplished in two periods, each lasting 1 week. Taking into account the aforementioned considerations, we decided to time the first radiotherapy to begin within 24 h of surgery and the second radiotherapy to begin 1 week later, using a radiotherapy dose of 16–18 Gy/2f and a BED of 30–40 Gy, which is consistent with the current guidelines. Triamcinolone is a long-acting glucocorticoid that suppresses inflammation, diminishes the production of collagen and glycosaminoglycan,15 and prevents the proliferation of fibroblasts.16 Injections of intra-lesional steroid hormones have been demonstrated to be 50%–100% effective in preventing the recurrence of hyperplastic keloids and keloids17, 18 The timing of postoperative injections, however, is currently in dispute. Some experts19 contend that hormonal injections should be administered as soon as the keloid has been removed or in the early postoperative period, whereas Song20 contends that treatment administered during the static stage of pathological scarring will significantly improve the outcome. Injections given in the early postoperative phase, when the wound is inflamed, will likely raise the risk of bleeding, infection, and even flap necrosis, but injections given 4 weeks after surgery, when the wound is in the proliferative phase, will likely encourage a dynamic balance of collagen creation and degradation and produce superior therapeutic results. Triamcinolone should not be injected more than 40 mg/site during the first injection, since doing so could result in localized skin atrophy, hyperpigmentation, poor wound healing, or local capillary dilation.21, 22 5-FU, an anti-pyrimidine antimetabolite, atrophying keloid scars by inhibiting cell division and proliferation as well as local vascular proliferation.23 Low concentration 5-FU injection combined with glucocorticoid injection has been designated as the first-line injectable therapy for keloid prevention of postoperative keloid recurrence in the current Recommended Guidelines for the Clinical Treatment of Keloid Scars in China. Through our treatment with tretinoin combined with 5-FU injection, patients with a propensity to recurrence, such as hardness of the surgical area during follow-up, were effectively controlled. Additionally, we selected a self-adhesive soft polysilicone dressing to match as closely as possible to the complex contour of the auricular profile in order to maximize the efficacy of the silicone gel in suppressing scar creation. A magnet sheet ear stud or silicone nasal clip was added for compression on the outside of the self-adhesive soft polysilicone dressing, which not only better utilizes the scar-inhibiting function of the silicone gel but also prevents scar growth through pressure.
The innovations of this article include the following: (1) Emphasis contour priority with core excision and subsequent elimination of residual lesions with adjuvant treatments. Pointing out different surgical approaches for different anatomical sites of the auricle; (2) Establishing a standardized systematic treatment system that combines surgical treatment with three adjuvant treatments and observing postoperative treatment efficacy, as previous studies have mostly combined surgical treatment with one or two treatments; (3) Attach importance to the patients' education and satisfaction, reminding and supervising patients to regular follow-up and timely treatment.
In summary, for keloids of different morphology and anatomical locations, we have combined two surgical excisional options, “complete excision” and “core excision,” with postoperative treatments such as tretinoin +5-FU injection, electron beam radiation therapy and silicone gel sheet + magnet sheet compression. These sequential treatments not only preserve the shape of the auricular tissue and eliminate residual lesions, but also effectively prevent the recurrence of keloids and achieve favorable results. This study, however, has the drawback of being a single-center retrospective analysis with the source of patients being relatively uniform. Additional large-scale randomized controlled trials and the inclusion of additional cases are required to prove the superiority of this strategy compared to other conventional treatments.
AUTHOR CONTRIBUTIONS
Huanhuan Wu performs operations and provides method guidance. Guoxuan Dong involved in data collection, follow-up investigation, and original draft writing. Jintian Hu and Meng Wang perform radiotherapy and conceptualization. Yue Liu and Chunan Qu perform injection treatment and supervision. Qian Jin and Lianzhao Wang involved in supervision, and writing review and editing.
ACKNOWLEDGMENT
None.
ETHICAL APPROVAL
The Medical Ethical Committee of Peking Union Medical College, Plastic Surgery Hospital (No.H202008012js). The authors confirm that the ethical policies of the journal, as noted on the journal's author guidelines page, have been adhered to and the appropriate ethical review committee approval has been received.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.