Investigation of the possibility of using an augmented reality-based endotracheal aspiration simulation tool for nursing education
Abstract
Aim
We developed an augmented reality technology-based endotracheal aspiration simulation tool (the AR tool) consisting of three modes: a mode for nursing students to learn endotracheal aspiration by themselves (learning mode); a mode for repeated practice (practice mode); and a mode for confirmation testing (test mode). This study aimed to compare the learning outcomes of the AR tool with traditional training mannequins and identify potential uses and improvements of the AR tool.
Methods
We invited students, and faculty members from the three universities who agreed to cooperate in conducting this study. Fifty-four students and nine faculty members agreed to participate in this study. The students were divided into two groups. One group was to study with the AR tool and the other group was to study with the traditional half-body training mannequin for suction. The students in both groups were asked to demonstrate endotracheal aspiration on another full-body type training mannequin which could be used as a patient with a tracheostomy (Skill test). Group interviews with faculty members focused on the topic of the AR tool's potential use in nursing education and improvement needed.
Results
There was little significant difference in the skill test results of endotracheal aspiration of students in both groups. The students and faculty members both expressed an interest in the AR tool. They said it was suitable for self-study of endotracheal aspiration.
Conclusions
This AR tool is an effective teaching tool for learning the sequence of endotracheal suctioning, although there are some areas that need improvement.
1 INTRODUCTION
Endotracheal aspiration, a respiratory management skill, is a clinical skill that is routinely used in home care and medical settings in the airway management of children and the elderly. According to the Ministry of Health, Labor and Welfare guidelines, nursing students are required to learn endotracheal aspiration using a training mannequin or similar device as a skill to be mastered before graduation (Ministry of Health, Labour, and Welfare, 2020).
The complexity of endotracheal aspiration requires the skills to be adequately learned for it to be properly performed. Specifically, communication with the patient, assessment of the patients' respiratory status, knowledge of tracheostomy and respiratory management, and knowledge of aseptic procedures and suctioning maneuvers are required, and the complex procedures must be carried out in the correct sequence. Therefore, nurses should practice endotracheal aspiration repeatedly to ensure that it is safe and comfortable for the patient.
Nursing skills have traditionally been taught through lectures, demonstrations, exercises utilizing training mannequins and other equipment and hospital practicum. However, Hayden et al. (2014) conducted a longitudinal study of 666 nursing students and reported that the educational outcomes at the end of the program for new graduates who experienced up to half of their traditional clinical time in high-quality simulation were comparable to the outcomes of clinical practice, proving the importance of simulation education.
In addition, along with the recent development of computer technology, the use of so-called augmented reality (AR) is progressing in the medical and nursing care fields. Typical examples include virtual reality (VR), a technology that mimics an entire environment and replaces the user's world with a virtual world, and AR, a technology that combines the real world with computer-generated content to create an interactive world. In a recent review of the literature, AR was found to be widely used to alleviating chronic pain and psychiatric symptoms, acquiring surgical skills, teaching anatomy, and conducting medical, and nursing education. In medical education, it has also been reported to improve learning motivation and effectiveness (Barteit et al., 2021).
A previous review entitled “Effectiveness of Virtual Reality in Nursing Education: A Meta-Analysis” (Chen et al., 2020) reviewed the results of 12 VR-based nursing studies. The review included materials on non-technical skills such as nursing newborns and nursing patients with chronic obstructive pulmonary disease, as well as those dealing with technical skills such as urinary drainage and intravenous injection; however, no educational materials had been developed to enable self-learning of endotracheal aspiration procedures.
In Japan, Komizunai et al. (2020) developed a model that measures the whole-body movements and gaze of skilled nurses during tracheal suctioning, which is reflected in a humanoid model in the VR space. Colley et al. (2021) also developed a device for learning endotracheal aspiration skills (Patent No. 6980203). This device presents the endotracheal aspiration skills of skilled nurses in a 3D computer graphics video; however, it has not yet been widely used as a teaching tool.
Therefore, we developed an endotracheal aspiration simulation tool using AR technology consisting of three modes by examining the process by which nursing students learn endotracheal aspiration by themselves (hereinafter referred to as “the AR tool”).The three modes consisted of the learning mode which incorporated video explanations of endotracheal aspiration techniques into the AR teaching materials, the practice mode which did not provide video explanations but provided hints when students asked for help and allowed them to repeatedly practice, and a test mode which did not provide hints but allowed students to check their mastery of the techniques. The purpose of this study was to compare the learning outcomes of the three-mode AR tool for endotracheal aspiration with traditional training mannequins and to identify potential uses and improvements of the three-mode AR tool.
2 METHODS
2.1 Subjects and research collaborators
University students receiving basic nursing education and university faculty of fundamental nursing and adult nursing were selected as research subjects. The students were asked to conduct empirical research on the AR tool. The timing and methods of learning the endotracheal aspiration techniques differed among the three universities collaborating in the study. In one university, students performed endotracheal aspiration with a training mannequin, while in the other two universities, students simply watched a video or a demonstration by a faculty member. This study also aimed to identify the potential use of the AR tool. Therefore, it was necessary to confirm that students who had already learned and even novice students could learn endotracheal suctioning with this AR tool. Therefore, students' participation in this study was not limited by their grade level. Faculty members in the fundamental nursing and adult nursing science fields who are most likely to teach endotracheal aspiration were included in the study. The faculty members were asked to experience the AR tool and to give their opinions on its potential use in nursing education. In recruiting research collaborators, we invited students, and faculty members from the three universities who agreed to cooperate with us in conducting this study. Fifty-four students and nine faculty members agreed to participate in this study. The empirical studies were conducted from August to September 2022.
2.2 Procedures for empirical studies
The empirical study involving students was conducted according to a flowchart (Figure 1). The purpose of this study was to examine the potential use of the AR tool in education. In addition, because students did not have the same learning status in endotracheal aspiration, this empirical study was designed to assess the same level of endotracheal aspiration knowledge of methods and procedures in Step 1. Specifically, students read the handouts and watched the videos for basic knowledge and endotracheal aspiration procedures, then took 18 questions on knowledge and procedures (Data S1). They were not allowed to proceed to Step 2 until they had correctly answered all the quiz questions, repeating the self-study and quiz attempts when needed.

Students who completed Step 1 proceeded to Step 2. The students were divided into two groups: one group to study with the AR tool and the other group to study with the traditional half-body training mannequin for suction (M8511229-0 00 by Kyoto Kagaku Co., Ltd., in Japan) (the TM tool). The AR tool group received 10 min of instruction on how to use the head-mounted display (VIVE Pro by HTC Co., Ltd., in Taiwan) (hereafter, HMD) and the AR tool. Then, they put on the HMD and adjusted it. After the HMD was put on, they experienced the learning mode of the AR tool for 10 min and the practice mode for 15 min. During this time, students were allowed to view the paper materials distributed to them. Students in the TM tool group received a 5 min explanation of how to use the TM tool and then practiced by themselves for 25 min while reviewing the paper materials distributed to them. The AR tool group had 29 students and the TM tool group had 24.
In Step 3, students in both groups were asked to demonstrate endotracheal aspiration on a full-body type training mannequin (MW25 11, 404-000 by Kyoto Kagaku Co., Ltd., in Japan) which could be used as a patient with a tracheostomy. Two nursing faculty members per student checked the appropriateness of the endotracheal aspiration skill. The 32 checkpoints in Table 2 were used to determine whether the skill was properly performed or not. The total score of the skill test was calculated as follows: two points were awarded if the procedure was correct and the skill was performed accurately, one point if the procedure was correct but the skill was not sufficiently appropriate, and zero points if the skill was not performed or the skill was inappropriate. In the event of a disagreement between the two evaluators, a good evaluation was adopted in principle after a third-party faculty member confirmed the reasons for the point reduction. The time required was also measured using the same brand of stopwatches. Students in the TM tool group experienced the AR tool after Step 3.
In Step 4, students in the AR tool group rated their understanding and ease of use of the AR tool on a scale of 1–10, with higher scores indicating positive results. Students in both groups also provided free-writing comments about the AR tool. We compared the percentages and times of performance attainment on the skill test between the two groups. In addition, we examined both groups' impressions and opinions of the AR tool to identify areas that required improvement.
2.3 Group interviews with the faculty
For the faculty research collaborators, four group interviews were conducted with 2–3 participants after 15 min of experience with the AR tool. The main questions asked in the group interviews were about the demographics of the faculty members, the current state of practice education with the TM tool, and the possibility of using the AR tool. The group interviews were recorded with an integrated chip recorder and then transcribed.
2.4 Details of the AR tool
The AR tool used in this study was developed based on the devices presented in a previous study by this team (Yamabe et al., 2021). These devices have been developed to simulate an environment including a virtual patient and some instruments and superimpose computer graphics as AR. The devices measure the position of the catheter tip and indicate it for students. The apparatus AR tool consisted of the following.
2.4.1 Devices
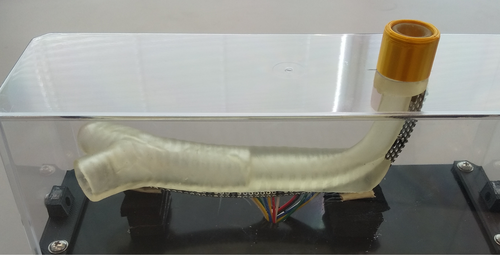
- Tracheal model (3D-printed translucent, Figure 2).
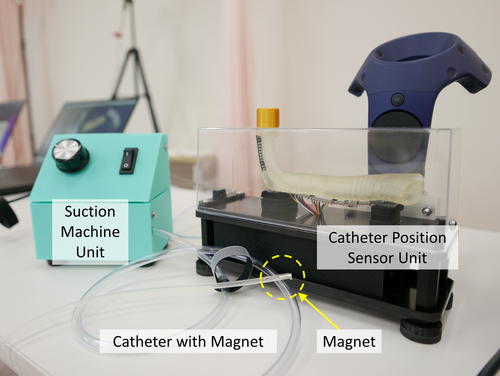
- Catheter position sensor unit with
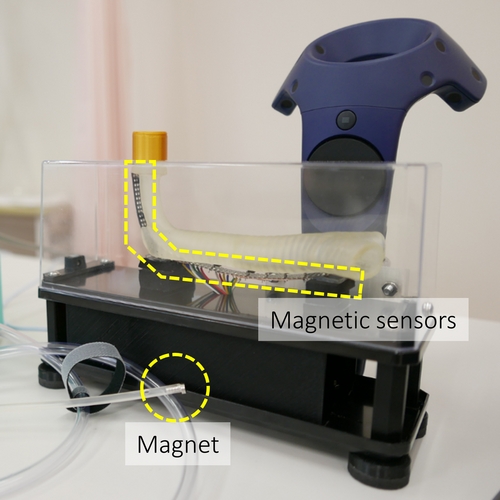
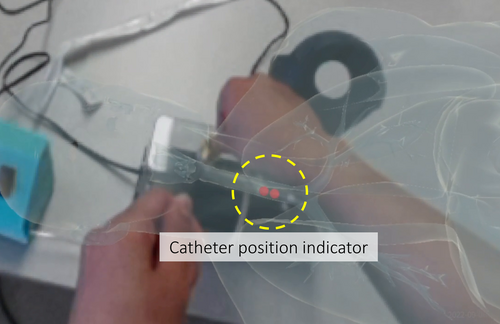
- A group of magnetic sensors attached to the tracheal model (Figure 3, right).
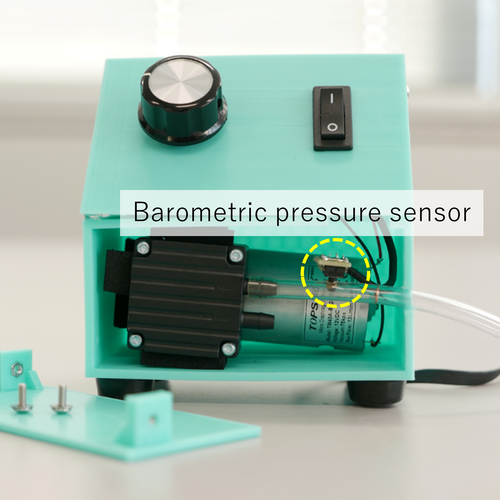
- Suction machine unit (Figure 3, left) which detects catheter bending while simulating a suction machine.
- Catheter with a magnet (Figure 3, center).
2.4.2 Systems

Figure 5 is a configuration of all the systems and the devices which assist to learn nursing skills regarding endotracheal aspiration.
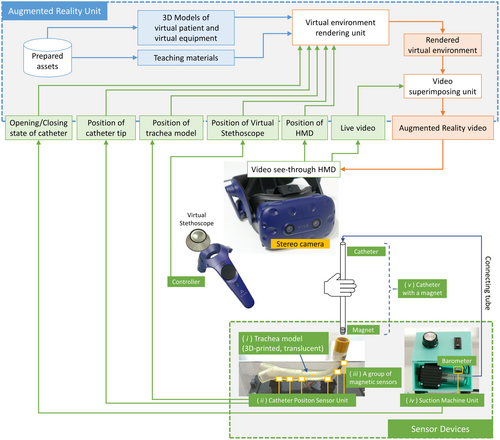
By wearing the HMD, the students could learn, through AR images, to synthesize the surrounding environment and computer graphics teaching materials. HTC VIVE Pro, which is commercially available for consumer use, was used as the head-mounted display. The instruments and buttons synthesized in computer graphics are operated using a controller for HTC VIVE Pro. In particular, the virtual stethoscope can be held virtually in the hand, and students can also listen to lung sounds by holding it close to the virtual patient through the HMD's headphones. Differences in lung sounds can be heard and compared before and after endotracheal aspiration. Before suctioning, breath sounds and adventitious sounds are heard. After suctioning, only breath sounds are heard. The aforementioned devices (i) ~ (v) are prepared to perform the tracheal suctioning procedure as physical devices.
The 3D printed tracheal model (device [i]) was made of translucent resin so that the insertion position of the catheter could be easily seen from the surroundings. The 3D position of the tracheal model was tracked in real-time by one of the controllers mounted on the back of the model, and a computer graphics virtual patient was superimposed in the students' field of view (Figure 6). The tracheal model was equipped with multiple magnetic sensors that respond to a magnet attached to the tip of a catheter. They tracked the catheter tip's position in real-time (Figure 7). The tracked catheter tip's position was fed back to the students by an AR indicator (Figure 8). The suction machine unit provides the sound and vibration of the suction machine to the students and detected the bending of the catheter with a barometric sensor (Figure 9).

The AR tool consists of three modes: the learning mode to learn endotracheal aspiration by themselves; the practice mode for practice repetition; and the test mode for learning confirmation. The learning mode was designed to allow the student to learn the procedure by presenting texts and videos showing the endotracheal suction procedure on the AR screen. The practice mode is the one in which the texts and videos of the procedure are removed from the learning mode. If a mistake was made during the procedure, or an incorrect answer such as oxygen saturation or cuff pressure was given, or if it took more than a certain amount of time before the next operation, the option to “see a hint” was presented and the user could ask for a hint. If the answer was still incorrect after viewing the hint, the correct procedure could be viewed. The test mode was set up so that the videos and hints were not presented, and if a mistake was made during the procedure or a certain amount of time elapsed before the next action, the incorrect answer was given and the correct procedure that should have been performed next was presented. The test mode was automatically graded by the system to ensure that the correct procedure was performed at the 15 checkpoints. Students were shown the number of correct and incorrect answers at the end of the exam.
2.5 Analysis methods
For the students' endotracheal aspiration skill test in Step 4, the percentage of students who correctly performed each procedure was compared between the two groups using the Chi-square test. The total score and amount of time required were calculated by comparing the mean scores of the two groups (independent-samples t-test), the interaction between the two groups and the grade level, and the percentage of students who properly performed each skill. Students' free-text statements were categorized based on semantic content.
For the group interviews of faculty members, meaningful sentences about the AR tool were extracted as codes from the transcribed texts, and codes with the same content were aggregated. The meanings of the codes were classified and categorized.
2.6 Ethical considerations
This empirical study was conducted with the approval of the ethics committee of Kawasaki City College of Nursing (approval number: R1111). In addition, during the technology test in Step 3 for the students, the evaluation was conducted by a research team member from a university other than the student's home institution. In group interviews with the faculty members, the research team members, who were different from the cooperating faculty members, served as facilitators.
3 RESULTS
3.1 Results of the empirical study with students
3.1.1 Distribution of students' grades
The number of students in each grade is presented in Table 1. The first grade had the largest number of students (61.1%), and the percentages of grades did not differ significantly between the two groups.
| Group | Grade of students | Number of students | Percentage of gradesa | Mean score of performanceb | SD |
|---|---|---|---|---|---|
| AR tool | 1 | 17 | 58.6% | 47.4 | 8.0 |
| 2 | 1 | 3.4% | 52.0 | − | |
| 3 | 6 | 20.7% | 56.5 | 2.4 | |
| 4 | 5 | 17.2% | 59.8 | 1.3 | |
| Total | 29 | 100.0% | 51.6 | 8.1 | |
| TM tool | 1 | 16 | 64.0% | 48.4 | 6.1 |
| 2 | 3 | 12.0% | 52.3 | 5.5 | |
| 3 | 3 | 12.0% | 52.7 | 6.0 | |
| 4 | 3 | 12.0% | 58.3 | 4.5 | |
| Total | 25 | 100% | 50.6 | 6.5 |
- Note: Intergroup (AR tool, TM tool): F = 0.159 P = .692. Intergrade of students: F = 7.667 P < .001. Interaction of group and grade: F = 0.355, P = .786.
- Abbreviations: AR tool, augmented reality model of endotracheal aspiration; TM tool, traditional simulation mannequin.
- a Fisher–Freeman–Halton's exact test P = .551.
- b Total score of skill test in endotracheal aspiration (perfect score was 64).
3.1.2 Understanding and interest in the AR tool and results of skill tests
Table 2 shows the percentage of students who rated their performance as adequate (two points) at 32 observation points in the skill test. The percentage of students who were deemed appropriate at each observation point ranged from 24% to 100%. Although the AR tool group was significantly lower at confirmatory point 32, “recording the nature and results of the procedure in the medical record,” there was no significant difference in the percentages between the two groups for the other items. The confirmation points were scored to check for interactions between groups and grades (Table 1). No interaction effects were found. Although there was no significant difference in scores between the two groups, there was a significant difference between grades, with third-graders and fourth-graders scoring higher than first-graders. The results of the 15 checkpoints set within the test mode of the AR tool are also presented in Table 2. All results were high range in 90%–100%.
| Order | Procedure | AR tool | TM tool | P value | Test mode |
|---|---|---|---|---|---|
| n = 29 | n = 25 | n = 29 | |||
| 1 | Verify the patient's identity. Use multiple methods of patient identification according to the facility's standards. | 58.6% | 52.0% | .296 | – |
| 2 | Explain the purpose of performing tracheal suctioning and obtain the patient's consent. | 72.4% | 68.0% | .764 | – |
| 3 | Check the required items. | 48.3% | 45.8% | .622 | – |
| 4 | Perform hand hygiene with alcohol cleanser, and wear a plastic apron, mask, and eye guard. | 65.5% | 44.0% | .254 | – |
| 5 | Auscultate and identify the area where sputum is present. | 75.9% | 72.0% | .552 | – |
| 6* | Confirm that the cuff pressure is appropriate with a cuff manometer (2.0–2.9 Kpa or 20–30 cmH₂O, 5–22 mm Hg). | 62.1% | 52.0% | .122 | 100.0% |
| 7* | Attach the pulse oximeter to the patient. | 96.6% | 96.0% | .915 | 93.3% |
| 8* | Confirm that transcutaneous arterial blood oxygen saturation values measured with a pulse oximeter are in the normal range. | 96.6% | 96.0% | .915 | 93.3% |
| 9* | Wear disposable gloves on the nondominant hand. | 86.2% | 84.0% | .974 | 100.0% |
| 10* | Open the rubbing alcohol cotton and sterile distilled water. | 58.6% | 56.0% | .810 | 100.0% |
| 11* | Activate the aspirator. | 96.6% | 100.0% | .349 | 93.3% |
| 12* | Open only the connector portion of the catheter and connect it to the connecting tube. Check the suction pressure while the connection between the catheter and the connecting tube is closed. | 82.8% | 84.0% | .977 | 96.7% |
| 13 | Check suction pressure. Adjust suction pressure to 13–16 kPa (equivalent to 100–120 mm Hg). | 89.7% | 88.0% | .217 | – |
| 14* | Wear sterile gloves on the dominant hand. | 86.2% | 84.0% | .255 | 93.3% |
| 15 | Remove the catheter and hold it with the dominant hand (the one that is clean). | 86.2% | 88.0% | .456 | – |
| 16 | Flex the connector portion of the tubing with an ungloved hand to avoid negative pressure. | 93.1% | 68.0% | .055 | – |
| 17* | With gloved hands, insert the catheter into the endotracheal tube. | 93.1% | 100.0% | .409 | 100.0% |
| 18* | Unbend the connector area and apply negative pressure. | 93.1% | 80.0% | .352 | 86.7% |
| 19* | Unbend the connector area and apply negative pressure. | 86.2% | 84.0% | .974 | 96.7% |
| 20* | Aspirate while pulling out the catheter. | 100.0% | 96.0% | .277 | 90.0% |
| 21* | The catheter insertion time is handled within 10–15 sec. | 75.9% | 72.0% | .552 | 90.0% |
| 22 | Wipe off secretions on the outer wall of the catheter with alcoholized cotton | 86.2% | 68.0% | .081 | – |
| 23 | Aspirate sterile distilled water to flush the catheter lumen. | 86.2% | 68.0% | .109 | – |
| 24 | Suction the upper cuff and perform oral and nasal suctioning as needed. | 58.6% | 72.0% | .253 | – |
| 25* | Stop the aspirator. Disconnect the connecting tube from the catheter. | 100.0% | 100.0% | 1.000 | 100.0% |
| 26 | Hold the catheter in one's palm, remove the glove by wrapping it, and discard the gloves and the catheter. | 69.0% | 84.0% | .279 | – |
| 27 | Remove the eye guards and the aprons. | 69.0% | 68.0% | .929 | – |
| 28 | Auscultate to determine if sputum has been removed. | 72.4% | 64.0% | .795 | – |
| 29* | Observe the general condition, respiratory status, and vital signs | 51.7% | 56.0% | .091 | 96.7% |
| 30 | After hand hygiene, measure the cuff pressure and confirm that it is within 2.0–2.9 Kpa (20–30 cmH₂O, 15–22 mm Hg). | 51.7% | 48.0% | .300 | – |
| 31 | Perform hand hygiene and leave the room. Clean up used items appropriately. | 34.5% | 24.0% | .665 | – |
| 32 | Recording the nature and results of the procedure in the medical record. | 31.0% | 68.0% | .013 | – |
- Note: χ2-test. The 15 points set to check achievement in the test mode are marked with an asterisk (*).
- Abbreviations: AR tool, augmented reality model of endotracheal aspiration; TM tool, traditional simulation mannequin; Test mode, the results of the students in AR tool group.
The AR tool group's understanding and interest in the AR tool were confirmed, with high scores as shown in Table 3.
| Questionnaire | Mean | SD |
|---|---|---|
| Are you interested in the learning mode? | 9.5 | 1.1 |
| Did you understand the learning mode? | 9.6 | 0.8 |
| Were you interested in the practice mode? | 9.8 | 0.5 |
| Did the practice mode tips help? | 9.7 | 0.8 |
| Was it easy to understand how to use the AR tool? | 9.6 | 1.0 |
| If you have access to the AR tool, would you be willing to learn on your own? | 9.4 | 1.0 |
| Was the AR tool practice time adequate? | 9.2 | 1.5 |
| Was the classroom environment comfortable? | 9.8 | 0.6 |
| AR: augmented reality model of endotracheal aspiration | ||
| The questionnaire was developed by the authors |
- Note: Students were asked to answer on a 10-point scale ranging from not at all true (1) to exactly true (10).
3.1.3 Amount of time required for endotracheal aspiration in the skill test
The mean time required for the AR group was 384.4 s (SD ±17.7) and 366.0 s (±15.9) for the TM group; there was no significant difference in this parameter between the two groups, although the AR group tended to take slightly longer. There were also no significant differences by grade level.
3.1.4 Students' comments on the AR tool
After the completion of all experiences, the two groups of students were asked for their impressions of the AR tool in a free-text format. There were comments indicating the potential of the AR tool as a learning tool, such as “This tool can be used for self-practice”, “Suitable for entry-level students because of the explanations”, and “It is an interesting and fun learning tool” (Table 4).
| Content of students’ free statements | AR tool | TM tool |
|---|---|---|
| n = 29 | n = 25 | |
| Potential for use as a teaching tool | ||
| This tool can be used for self-practice. | 6 | 5 |
| Suitable for entry-level students because of the explanations. | 6 | 4 |
| It is an interesting and fun learning tool. | 5 | 7 |
| This tool helps students remember a series of steps. | 4 | 2 |
| This tool helps students practice efficiently. | 3 | 0 |
| The use of AR materials in on-campus exercises would be effective. | 2 | 3 |
| Learning is more effective with both AR tool and model dolls. | 2 | 1 |
| It could also be used to educate new nurses in hospitals. | 1 | 0 |
| Students can learn without undue tension. | 0 | 1 |
| AR materials can help save space in simulators. | 0 | 1 |
| Strengths of AR tool as specific educational materials | ||
| The position where the catheter is inserted is indicated by a red point. | 4 | 2 |
| The noise from lung sounds is audible on auscultation. | 2 | 4 |
| Suctioning can be performed considering anatomy and physical assessment. | 3 | 2 |
| Students can actually insert the catheter. | 2 | 0 |
| Suction sounds are played, so it feels like actual suction. | 1 | 0 |
| The process is easy to understand because video explanations are provided in the learning mode. | 1 | 1 |
| AR images are practical. | 2 | 1 |
| The correct/incorrect feedback function is effective for learning. | 1 | 0 |
| Difficult to use and needs improvement | ||
| Difficult to see the actual thing or the hand. | 3 | 5 |
| It is difficult to insert the catheter because of misalignment in the image. | 3 | 0 |
| The HMD is misaligned. | 1 | 0 |
| Lots of left and right viewpoint movements. | 0 | 1 |
| Improvements in configuration, including aseptic manipulation and patient care. | ||
| The aseptic manipulation tends to be neglected in AR tool. | 3 | 1 |
| Students may be distracted by a series of procedures and neglect patient care. | 3 | 2 |
| It is better to have a configuration where students actually wear the gloves. | 2 | 1 |
| The lung sounds should be different in the auscultation position. | 0 | 1 |
| It would be good if students could think from the preparation and arrangement of supplies. | 0 | 1 |
| Fatigue during use | ||
| One's eyes get tired. | 2 | 0 |
| The user may experience VR sickness. | 0 | 2 |
| The goggle is heavy. | 0 | 1 |
- Abbreviations: AR tool, augmented reality model of endotracheal aspiration; HMD, head-mounted display; TM tool, traditional simulation mannequin.
Students also specifically mentioned the following strengths of the AR tool as a teaching tool: “The position where the catheter is inserted is indicated by a red point”, “The noise from lung sounds is audible on auscultation”, and “Suctioning can be performed considering anatomy and physical assessment.”
The opinions on areas for improvement were “Difficult to see the actual thing or the hand”, “Aseptic manipulation tends to be neglected in the AR tool”, “Students may be distracted by a series of procedures and neglect patient care”, and “It is better to have a configuration whereby students actually wear the gloves.” There were also four comments about feeling eye fatigue and VR sickness.
3.2 Results of group interviews with participating faculty members
The specialties of the nine faculty participants included five in fundamental nursing science and four in adult nursing science. The number of years of teaching experience ranged 5–10. Their work experience ranged 4–13 years. The duration of the four group interviews ranged from 35 to 65 min.
3.2.1 Faculty members' comments on group interviews
There were some comments about the advantages of this AR tool, which included the following: “The position where the catheter is inserted is indicated by a red point”, “It is useful for learning a series of procedures”, and “The AR tool can be tied to anatomy and physical assessment” (Table 5).
| Category | Codes | Numbers of codes |
|---|---|---|
| Advantages of this AR tool | ||
| The position where the catheter is inserted is indicated by a red point. | 12 | |
| It is useful for learning a series of procedures. | 11 | |
| AR tool can be tied to anatomy and physical assessment. | 10 | |
| AR tool makes learning fun and game-like. | 5 | |
| The feedback for incorrect answers motivates students to learn. | 8 | |
| It allows for labor-saving preparation and cleanup. | 4 | |
| AR tool saves space and can be used for separate class exercises. | 4 | |
| Actions can be recorded and used for reflection. | 3 | |
| About the three modes | ||
| The three modes are helpful when practicing independently. | 10 | |
| There is less information in the practice mode, so there is more tension. | 7 | |
| Tips are presented in the practice mode. | 5 | |
| The test mode could actually be utilized. | 5 | |
| The practice mode made me aware of the time spent on the procedure. | 3 | |
| Three different modes can be used depending on the learning objectives. | 3 | |
| It would be useful if the practice mode could record the student's learning history. | 1 | |
| About sound effects | ||
| The sound effects make me feel like I'm actually suctioning. | 7 | |
| Auscultatory sounds are more realistic if they vary by lung area. | 6 | |
| The lung sounds are audible on auscultation. | 4 | |
| The disappearance of lung murmurs after aspiration is commendable. | 1 | |
| About the visibility on the screen | ||
| It is hard to see the actual thing. | 5 | |
| The screen appears vivid. | 4 | |
| There are many left and right viewpoint shifts of the learner on the screen. | 3 | |
| The tracheostomy site is somewhat difficult to see. | 3 | |
| The desks in AR space should actually have desks there. | 2 | |
| It should give the feeling of a bed in an AR space. | 1 | |
| About the comfort of wearing a HMD | ||
| Changing the material of the HMD sheet makes it less likely to shift. | 5 | |
| There is some concern that some students may get VR sickness. | 3 | |
| HMD is heavier than expected. | 2 | |
| Putting on the HMD takes lots of time. | 2 | |
| Feels hot and humid when wearing HMD. | 2 | |
| Difficulty in adjusting the HMD. | 1 | |
| Specifics requiring improvement | ||
| Wearing gloves is more appropriate for the actual procedure of endotracheal aspiration. | 12 | |
| Eye-tracking technology can be used in the AR tool. | 10 | |
| It would be helpful to have feedback on unclean behavior. | 8 | |
| In the learning mode, providing explanations about mistakes would be helpful. | 7 | |
| There can be transparent and non-transparent patterns on the screen. | 7 | |
| The patient's reaction and facial expression should change. | 5 | |
| It is more effective to let students think through the part of preparing and arranging items. | 4 | |
| The step that requires holding the controller all the time needs improvement. | 4 | |
| Change the SPO2 value setting to a lower value. | 3 | |
| It is more effective to increase the situations in which students can think. | 3 | |
| The background should also be an image of a hospital room. | 2 | |
| It is effective if students can practice lots of times in areas where they made mistakes. | 2 | |
| The glove removal and attachment steps should be learned separately and combined with the AR portion. | 2 | |
| It is better to put trash cans on the floor. | 2 | |
| Students need training to use AR tool. | 2 | |
| Talking to the patients should be included in the checklist of AR tool. | 2 | |
| The time to auscultate should be added to the checklist (more than one breath). | 1 | |
- Abbreviations: AR tool, augmented reality model of endotracheal aspiration; HMD, head-mounted display.
About the three modes, faculty members said, “Three modes are helpful when practicing independently”, and “There is less information in the practice mode; so, there is more tension”. Faculty members made the following comments about sound effects: “The sound effects make me feel like I am actually suctioning” and “Auscultatory sounds are more realistic if they vary by lung area”. Some commented “It was hard to see the actual thing” due to the visibility of the screen, while others said “The screen appears vivid”. Regarding the comfort of wearing an HMD, there were comments such as “Changing the material of the HMD sheet makes it less likely to shift” and “There is some concern that some students may get VR sickness”.
Regarding areas for improvement, many participants expressed opinions such as “Wearing gloves is more appropriate for the actual procedure of endotracheal aspiration”, “Eye-tracking technology can be used in the AR tool”, “It would be helpful to have feedback on unclean behavior”, “In the learning mode, providing explanations about mistakes would be helpful”, and “There can be transparent and non-transparent patterns on the screen”.
4 DISCUSSION
We developed an AR-based endotracheal aspiration simulation model consisting of the learning mode, the practice mode, and the test mode, and evaluated its potential for use in nursing education for students and faculty members.
In this study, the students' acquisition of endotracheal aspiration skills did not differ significantly between the AR tool and the TM tool in total skill test scores and time required. In a systematic review evaluating AR-based teaching materials in medical education, an analysis of 27 studies reported that AR materials were at least equivalent to traditional methods of medical education and were beneficial in terms of motivating students to learn (Barteit et al., 2021). In addition, in a comparison between VR materials and conventional education using mannequins and other materials in nursing education, the results of a meta-analysis of skill tests performed in five studies reported that there were no significant differences between the two groups (Chen et al., 2020).
The results of the present study are similar to those of the abovementioned studies, and it can be said that students were able to learn endotracheal aspiration skills with the AR tool to the same extent as with traditional mannequin-based learning.
The development of AR educational materials is progressing rapidly, and attempts are also being made to use automated VR simulation artificial intelligence (King et al., 2022). While there are many educational materials that utilize AR technology, none of them has been reported to use the three modes to support the learning process. Students' appreciation of the AR tool's learning and practice modes in terms of understanding and interest was high. The ability of students to obtain feedback on the correctness or incorrectness of the skills, which is a strength of the AR tool, differentiates it from traditional materials. In the students' free descriptions, they also commented that the tool is useful for self-study and can be used even by first-time students. In summary, the AR tool is an effective teaching tool that helps students to learn the sequence of endotracheal aspiration, from the initial patient interaction to the final cleaning up of the items used in the process. This AR tool incorporates the test mode for skill testing. The results of the test mode showed better results compared to the results of the skill test using a full model mannequin. The difference in values can be considered from two aspects: the nervousness on the part of the student because there were two observers in the skill test, and the accuracy of the observation, where the observers were judging not only whether the student was able to perform the procedure, but also whether they had correctly performed the skill. One issue to be addressed in the future will be to improve the accuracy of the test mode decisions.
A large-scale survey of general teachers conducted in Russia revealed that teachers have a moderately positive perception of the use of VR materials; however, only 10% of them daily use VR materials. This survey also revealed that teachers who are more familiar with VR technology try to use it more often (Khukalenko et al., 2022). In another study, nursing graduates were asked about their impressions of VR materials in learning to make clinical decisions in emergency situations (Mäkinen et al., 2023). However, only a few studies have investigated the potential use of AR educational materials with nursing faculty members, who are the people who introduced AR educational materials. In this study, faculty members also appreciated the fact that the AR tool allowed students to learn about endotracheal aspiration while utilizing their knowledge of tracheal anatomy and physical assessment. Furthermore, they mentioned the possibility of introducing the AR tool to the classroom, such as saving manpower in preparation and post-processing, and being used for reflection with students, and so forth. In order to activate the use of VR educational materials, it must be necessary to provide teachers with an experience and a perception of their usefulness.
However, there are several improvements that could be made to the AR tool to ensure it is even more effective for nursing education. Specific improvements that need to be considered include addressing the difficulty in seeing the hand, adding a device to make students aware of the aseptic manipulation involved in the procedure, and adding patient handling through voice recognition technology. Table 2 also shows that some modifications to the expression of the AR tool are needed for procedures, with a low percentage of students being able to perform them, and more accurate observations of the test mode are required.
The main limitation of this study was that the students who participated in it were not of the same grade. Therefore, grade interaction was observed in the results of Step 3, the skill test performances. However, since there was no difference in the percentage of grade composition between the AR and TM tool groups, we did not consider the non-uniformity of the grades of our study participants a major limitation. In the future, by increasing the number of participating students and examining differences in learning by grade, it may be possible to suggest more specific ways of using the AR tool in exercises.
5 CONCLUSIONS
For our AR-based endotracheal suctioning simulation model, which consists of a learning mode, a practice mode and a test mode, the students' skill acquisition was as effective as that of a conventional tracheal suction manikin, and students rated it as suitable as self-learning material. The faculty members also evaluated that this could be used for basic nursing education. However, it would be easier to facilitate its use by making the improvements pointed out by both the faculty members and students.
AUTHOR CONTRIBUTIONS
All authors meet the criteria for authorship and are listed as authors. Mikako Arakida organized the study and oversaw the research. Tokiichiro Takahashi was the technical leader in the development of the AR-based endotracheal aspiration simulation tool. Yuko Matsuda, Chizuko Miyamoto, Emiko Aoki, Sawako Takahashi, Mizuho Ando, Ruriko Yamashita and Takahiro Igarashi provided input from a nursing perspective in the development of the AR-based endotracheal aspiration simulation tool. They also recruited participants for the demonstration, ran the demonstration and collected data. Yuta Yamabe, Tomoaki Moriya, Shuhei Kodama, Keito Tanizaki and Kenta Uchida made a technical contribution in the development of an AR-based endotracheal suction simulation tool. They also managed the demonstration case and collected data.
ACKNOWLEDGMENTS
This work was supported by JSPS KAKENHI Grant Number 17H04436.
CONFLICT OF INTEREST STATEMENT
The authors have no potential conflict of internet to declare.




