Cost Effectiveness of Colorectal Cancer Screening Strategies in Middle- and High-Income Countries: A Systematic Review
Funding: The authors received no specific funding for this work.
ABSTRACT
Background and Aim
Colorectal cancer (CRC) is a significant global health burden, and screening can greatly reduce CRC incidence and mortality. Previous studies investigated the economic effects of CRC screening. We performed a systematic review to provide the cost-effectiveness of CRC screening strategies across countries with different income levels.
Methods
We searched relevant scientific databases (PubMed, Embase, Ovid, Web of Science, Scopus) from January 1, 2010, to December 31, 2023. We selected English-language studies related to model-based economic evaluations of CRC screening strategies. Information such as the characters of screening tests, model characteristics, and key cost-effectiveness findings were collected. The net monetary benefit approach was used to compare the outcomes of various strategies.
Results
A total of 56 studies were identified, including 46 from high-income countries (HICs), 6 from upper-middle-income countries (UMICs), and 4 from lower-middle-income countries (LMICs). Most annual fecal occult blood tests and fecal immunochemical tests were cost-saving, and colonoscopy every 10 years was cost-saving. Other strategies involving multitarget fecal FIT-DNA detection, computed tomography colonography, and flexible sigmoidoscopy were cost-effective compared with no screening. Newer strategies such as magnetic resonance colonography every 5 years, annual urine metabolomic tests, and fecal bacterial biomarkers were cost-effective compared with no screening.
Conclusion
In our updated review, we found that common CRC screening strategies and magnetic resonance colonography continued to be cost-effective compared with no screening. Areas for further development include accurately modeling the natural history of colorectal cancer and obtaining more evidence from UMICs and LMICs.
Graphical Abstract
1 Introduction
Colorectal cancer (CRC) is the third most common cancer and the second leading cause of cancer death worldwide, with over 1.9 million new cases and 935 000 deaths expected in 2020 [1]. The highest incidence and mortality rates are observed in high-income countries (HICs) such as Europe, Oceania, and North America [2]. However, countries undergoing economic development and experiencing changes in diet and lifestyle are witnessing rapid increases in incidence [3]. In countries with lower economic status, current screening programs and medical treatments are inadequate in reducing the increasing rates of CRC [4]. Implementing optimal screening strategies for CRC presents an opportunity for improving public health [5].
Various screening modalities have been evaluated for reduction of CRC incidence and mortality in average-risk individuals [6, 7]. These include stool-based tests, a semi-invasive approach using computed tomography (CT) imaging, and direct visualization of the distal or entire colon with sigmoidoscopy or colonoscopy [8]. However, current screening modalities each fall short in different aspects with respect to access, cost, cultural acceptance, risk of complications, test characters, and patient and provider knowledge gaps [8]. To address these limitations, novel screening tests have been developed based on advancements in CRC molecular biology, genetics, and epigenetic [8]. However, there is no consensus that the new strategy is necessarily superior to current screening strategies, and the broad adoption of all potentially advantageous screening strategies may be unfeasible for numerous nations, particularly in lower-middle-income countries (LMICs) [9, 10].
Economic evaluations for various screening strategies can provide evidence-based support for advocacy, policy-making, and patient-care decisions for health care policymakers [11]. Since 1984, several model-based cost-effectiveness analyses of CRC screening have been conducted in countries at different income levels [12-14]. Therefore, the aims of this study were threefold: firstly, to provide an overview of the evidence base and similarities and differences in screening strategies in different income countries; secondly, to summarize the cost-effectiveness results of screening strategies in different income countries; and thirdly, to identify key issues to inform future analyses in LMICs and upper-middle-income countries (UMICs).
2 Methods
We searched PubMed, Embase, Ovid, Web of Science, and Scopus for studies published between January 1, 2010, and December 31, 2023. We used different queries matching the keywords in each database to identify the relevant cost-effectiveness analyses (the complete search strategy is shown in Text S1). To identify studies not captured by our database searches, we manually checked the reference lists of retrieved articles.
We included original peer-reviewed articles or reports written in English that provided information on the cost effectiveness of CRC screenings and that have comparable screening recommendations. Text S2 describes the detailed selection criteria. Two researchers (Y.X.L and W.W.S) independently screened the article titles, abstracts, and full texts. The 28-question checklist informed by Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) [15] was used for quality assessment of the studies (Table S1). The final list then was checked independently (Y.Y.).
We focused on the characters of six screening tests (fecal occult blood test [FOBT], fecal immunochemical test [FIT], multi-target fecal FIT-DNA detection [MT-sDNA], computed tomography colonography [CTC], flexible sigmoidoscopy [FS], and colonoscopy), based on recent recommendations [16-18] and the popularity of the strategies [19]. Different from the 2019 review [20], we added MT-sDNA and CTC in our analysis, considering their growing popularity and recommendations from various agencies [16-18]. Following this, we manually checked the reference lists of retrieved articles from research containing new screening tests. After finding the original study, we structured the pertinent screening characteristics, and consolidated data on sensitivity, specificity, cost, and screening compliance for both common and new screening tests. These findings were then stratified according to the countries' income levels, which are currently categorized into four groups: low, lower-middle, upper-middle, and high. The classification is based on the Gross National Income (GNI) per capita in US dollars, converted from the local currency using the Atlas method (https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups).
We extracted the model structure, basic parameters, and life-year (LY) and/or quality-adjusted life-year (QALY) information from the base-case scenario of the study. Subsequently, we extracted or calculated (if necessary) the incremental costs per LY saved or QALY gained. Costs were adjusted to 2023 US dollars by using the Consumer Price Index for medical care (https://eppi.ioe.ac.uk/costconversion/default.aspx), a widely utilized method in numerous reviews [21-23]. In cases where a study did not explicitly specify the base year for cost estimates, we presumed that the costs were denoted in the currency of 1 year before publication. If a strategy was less expensive (with a negative incremental cost) but equally or more effective compared with the baseline strategy (e.g., no screening), we categorized it as cost-saving (CS).
For each study, we recorded the incremental cost per LY or QALY gained values (compared with no screening) for common strategies and newer strategies. We also compared each strategy using a net monetary benefit (NMB) approach to determine the optimal strategy at different willingness-to-pay (WTP) levels [24]. First, at each WTP level, we calculated the NMB of each strategy by subtracting the cost from the product of the LYG (or QALY) and the WTP. Then, we identified the optimal strategy at each WTP level as that with the highest positive or lowest negative NMB value. We verified the results using the incremental cost-effective approach, which additionally gave us meaningful WTP reference thresholds.
3 Results
3.1 Study Characteristics
Our search identified 7325 citations, including 2787 duplications. Following removal of duplicates, title and abstract screening, and full-text reviews, we finalized the selection with 56 studies (Table S2). A diagram of the search process is depicted in Figure 1.
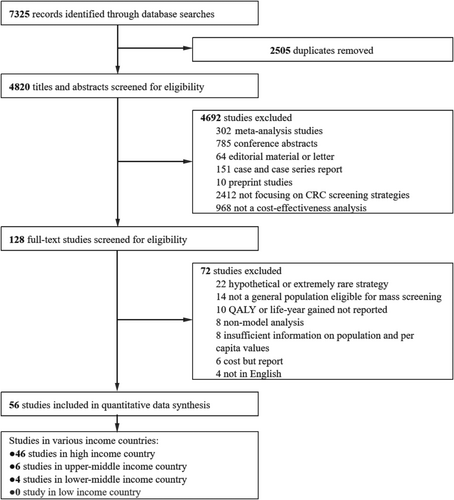
Forty-six studies were in HICs, whereas six were in UMICs and four were in LMICs. In the 46 studies of HICs (Table S3), 17 studies analyzed strategies in the United States. Additionally, 14 studies examined strategies in Europe, 7 studies analyzed strategies in Asia, 3 studies analyzed strategies in Canada, and another 3 studies focused on strategies in Australia. Additionally, there was one study each conducted in New Zealand and Alaska analyzing their respective strategies. The most common starting age for screening was 50 years, except for three studies using age 55 years, one study using 60 years, three studies using 65 years, one study using 45 years, and four studies using 40 years. For the ending age of screening, 74 or 75 years was most common, along with 80 years (11 studies), 70 years (4 studies), 64 or 65 years (2 studies), 85 years (1 study), and 100 years (1 study). The majority of the studies took a healthcare system's perspective, except for 11 studies taking a societal perspective, 12 studies taking a third-party payer's perspective, and 5 studies with no available information. A time horizon of 30 years or longer was used in most studies, except for five studies with no available information, four studies (24 or 25 years), one study (14 years), and one study (12 years). All but one study reported discounted values, with 3% being the most common discount rate, except for 1% (one study), 1.5% (one study), 3.5% (two studies), 4% (two studies), 5% (five studies), and 3% for costs; 1.5% for health outcomes (two studies). In terms of effectiveness measurements, 19 of the 46 studies used LY, 26 used QALY, and 1 used both.
In the six studies of UMICs (Table S3), all were conducted in China. The starting age for screening was 50 years, except for one study that used 40 years. For the ending age of screening, 74 or 75 years were the most common (five studies), and one study used 80 years. The time horizon varied, consisting of 25 years, 34 years, and lifetime. Regarding the discount rate, five studies used 3%, whereas one study used 5%. In terms of effectiveness measurements, four studies used LY, and two study used QALY. Meanwhile, the four studies in LMICs consisted of one study each in Iran, Vietnam, Ukraine, and Thailand (Table S3). The screening age for all target populations is 50–75 years old. Two studies had a lifetime time horizon, whereas the other two had a time horizon of 25 years. Among these studies, two used a discount rate of 3%, one used a rate of 5%, and one did not report the discount rate. All four studies utilized QALY as the measure of effectiveness. With the exception of two studies in China that employed the MISCAN-Colon model, all studies utilized the Markov model.
In order to compare the specific differences between different income countries, we summarized the detailed information on the included studies (Table S4) and found that there is a large difference in GDP per capita in HICs, ranging from $23.01–85.37 thousand, but not much difference between UMICs and LMICs. Additionally, the analyses of uncertainty employed by countries with disparate income levels exhibit a notable degree of consistency and the majority of studies received financial support.
3.2 Characters of Common Strategies and Newer Strategies
The characters of common screening tests, divided by country income, has been reported across six outcome types: sensitivity for low risk adenomas [25] (one or two small (< 10 mm) tubular adenomas with no high-grade dysplasia); sensitivity for high risk adenomas [25] (i.e., numerous [≥ 3], large [≥ 10 mm], and/or of high-risk histology [tubulovillous or high-grade dysplastic changes]); sensitivity for CRC; specificity for CRC; cost per strategy; and compliance rate (Figure 2 and Table S5). In the HICs, there is a significant variation in the sensitivity of common screening tests for diagnosing CRC. Colonoscopy has the highest sensitivity (ranging from 91.5% to 100%), followed by FS, MT-sDNA, and CTC with sensitivity values between 95% and 96.6% (only MT-sDNA lowest 54.8%, the remaining two strategies above 75%). The sensitivity of FIT is lower (ranging from 66% to 87.2%), whereas the lowest sensitivity is observed for FOBT with values ranging from 19.1% to 70%. Specificity of these tests varies little (76.6% to 100%). In terms of cost, FOBT prices are the lowest ($4.52 to $29.19), followed by FIT costs approximately between $6.49 to $45.2. Then the overall cost of FS, MT-sDNA, and CTC did not differ significantly, ranging from $300 to $600. Notably, the cost of colonoscopy varies greatly ($80.5 to $1796). For both UMICs and LMICs, with the exception of the higher sensitivity of FIT and FOBT for adenomas in LMICs, the compliance rate with colonoscopy is estimated to be higher in UMICs, whereas the other aspects are similar to HICs.
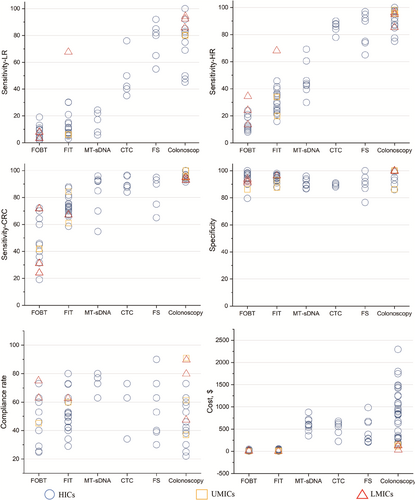
Table S6 clearly showed the adherence rates for screening strategies in different studies. Although some studies assumed the same adherence rate or set it based on the actual screening program, the reality was that the adherence rate for colonoscopy is usually lower than that for fecal based strategies. In addition, studies had set adherence rates for FOBT and FIT screening ranging from 15% to 100%. This suggests that the effect of screening strategies on adherence rates may be underestimated and that such differences may significantly affect cost-effectiveness evaluations.
We summarized the specific content and characters of the following new screening tests for population studies (Table 1 and Table S7). The sensitivity of the new screening tests for diagnosing CRC from high to low is magnetic resonance colonography (MRC) [26], capsule colonoscopy (CCE) [26-28], liquid biopsy (LB) [29], urine metabolomic test (UMT) [30], fecal bacterial biomarker (M3CRC) [31], and methylated Septin 9 blood test (mSEPT9) [27, 28, 30, 32]. The difference in specificity among these tests was relatively small. In terms of cost, CCE was found to be the most expensive (ranging from $645.4 to $1527.67), followed by LB, MRC, mSEPT9, UMT, and M3CRC. Compliance rates, derived from multiple sources including articles and a randomized controlled trial, vary from 25% to 99%, except for a few instances reporting 100% compliance. The data sources and specific content of each new screening tests can be found in the attachment (Table S8).
| Strategy | Author, year | Sensitivity for LR | Sensitivity for HR | Sensitivity for CRC | Specificity for CRC | Compliance | Cost, $ | Cost source |
|---|---|---|---|---|---|---|---|---|
| mSEPT9 | Peterse et al., 2021 |
21.2% (95% CI: 15%–23%) |
21.2% (95% CI: 18%–24%) |
68.0% (95% CI: 53%–80%) |
78.8% (95% CI: 76.7%–80.8%) |
100%a | 237.29 | Clinical laboratory fee schedule |
| Barré et al., 2020 | — | — | 66% | 91.00% | 65%b | 158.15 | National Health Insurance | |
| Lew et al., 2018b | — | 11.20% |
48.2% (95% CI: 32.4%–63.6%) |
91.5% (95% CI: 89.7%–93.1%) |
100%a | 190.36 | Assumed | |
| Ladabaum et al., 2013 | 100%a | 205.11 | Assumed | |||||
| UMT | Barichello et al., 2019 |
43.1% (95% CI: 29.5%–56.7%) |
43.1% (95% CI: 29.5%–56.7%) |
— |
91.3% (95% CI: 87.1%–95.5%) |
83.6%c | 86.93 | Based on consultation with the UMT vendor (Metabolomic Technologies Inc.) |
| — | — | 74% | — | |||||
| CCE | Peterse et al., 2021 |
91%d (95% CI: 85%–95%) |
92% (95% CI: 82%–97%) |
92%e (95% CI: 82%–97%) |
83% (95% CI: 80%–86%) |
100%a | 1527.67 | 2017 Physician Fee Schedule |
| Barré et al., 2020 |
86%d (95% CI: 82%–89%) |
87% (95% CI: 81%–91%) |
87%e (95% CI: 81%–91%) |
95.3% (95% CI: 91.5%–97.5%) |
25%f | 645.30 | National Health Insurance | |
| Hassan et al., 2011 |
89%d (95% CI: 70%–97%) |
88% (95% CI: 56%–98%) |
88%e (95% CI: 56%–98%) |
89% (95% CI: 86%–90%) |
40%f | 854.05 | Classification Commune des Actes Médicaux | |
| MRC | Greuter et al., 2016 |
84.0%d (95% CI: 63.9%–95.5%) |
100% (95% CI: 80.5%–100%) |
100%e (95% CI: 80.5%–100%) |
100% (95% CI: 95.2%–100%) |
34%g | 358.59 | Nederlandse Zorgautoriteit |
- Note: Costs were adjusted to 2023 US dollars.
- Abbreviations: CCE, colon capsule endoscopy; CRC, colorectal cancer; HR, high risk adenomas; LR, low risk adenomas; MRC, magnetic resonance colonography; mSEPT9, methylated Septin 9 blood test; UMT, urine metabolomic test.
- a The compliance rate was assumed to be 100%.
- b It was assumed based on the PSA-based prostate cancer screening in France.
- c It was estimated using the available data on adherence of other widely used urine-based screening tests.
- d The sensitivity of new strategy in the detection of polyps with diameters of 6–9 mm.
- e The sensitivity is assumed to be equal to the sensitivity for HR.
- f It was assumed consistency with other analytical strategies included in the study for comparison.
- g It was based on a randomized controlled trial in the Netherlands.
3.3 Model Characters
The study included a total of 36 articles that used Markov models, with 28 from HICs, 4 from UMICs, and 4 from LMICs. Additionally, 18 studies in HICs adopted a microsimulation approach (Table S9). In the Markov model, patients transition between different health states over a specified number of cycles, which is determined by the disease duration. Each cycle represents 1 year, and patients move between health states according to predetermined probabilities. Among the microsimulation models, three studies utilized the National Cancer Institute's Cancer Intervention and Surveillance Modeling Network (CISNET), which includes MISCAN-Colon, SimCRC, and CRC-SPIN. Furthermore, seven studies exclusively used the MISCAN-Colon model, three studies utilized the Policy1-Bowel model, two studies respectively adopted the ASCCA and Archimedes models, and one study each employed the CRC-AIM and SimCRC models. Additionally, one study created and validated a microsimulation model for the French context.
The microsimulation models generally considered the following health states: normal, small adenomas, medium adenomas, large adenomas, preclinical CRC, clinical CRC, and death. The specific definitions of these health states varied among the different analyses. The MISCAN-Colon model and other models used by Barré et al. [28] and Tuan et al. [33] considered the health status of non-progressive adenomas. The mean duration of adenoma varies significantly, ranging from 12.5 to 24.2 years. The shortest duration is observed in the MISCAN-Colon model, whereas the longest duration is found in the CRC-SPIN model. The mean duration of preclinical cancer ranges from 1.6 to 6.7 years. The time from adenomas onset to cancer diagnosis ranges from 17 to 26.4 years, with the shortest duration still observed in the MISCAN-Colon model and the longest in the CRC-AIM model. Except for CRC-AIM, Policy1-Bowel, and ASCCA models employ the American Joint Committee on Cancer Tumor Node Metastasis (AJCC TNM) staging system, whereas the rest use the Union for International Cancer Control Tumor Node Metastasis (UICC TNM) staging system. Although the specific findings varied, each study considered the adverse effects associated with colonoscopy.
3.4 Cost-Effectiveness Analyses
Of the 56 included studies, 40 focused on comparisons based on fecal testing (31 from HICs, 5 from UMICs, and 4 from LMICs), reporting the results of comparisons of common adopted screening strategies with no screening (Table 2). In HICs, 15 studies concentrated on the FOBT strategy, six studies reported that annual FOBT screening generated more QALY or LY and was cost-effective compared with no screening, resulting in CS. Meanwhile, two studies [28, 34] deemed biennial FOBT not cost-effective, but the remaining seven studies endorsed the cost-effectiveness of both annual and biennial FOBT. Additionally, 36 studies explored the FIT strategy, with 14 studies (in 27 studies) indicating that annual FIT was CS. Only one study [35] (in 15 studies) considered biennial FIT as CS. Moreover, 11 studies investigated the MT-sDNA strategy, with only one study [27] indicating that 3-yearly MT-sDNA was dominated, displaying significantly higher incremental cost-effectiveness ratio (ICER) values compared with other strategies. For both UMICs and LMICs, only one study [14, 36] each considered FOBT strategy as CS, whereas the rest indicated that annual or biennial FOBT and FIT strategies were cost-effective.
| Author, year | Country | Annual FOBT | Biennial FOBT | Annual FIT | Biennial FIT | 3-yearly MT-sDNA | 5-yearly MT-sDNA | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ΔCost/LYG | ΔCost/ΔQALY | ΔCost/LYG | ΔCost/ΔQALY | ΔCost/LYG | ΔCost/ΔQALY | ΔCost/LYG | ΔCost/ΔQALY | ΔCost/LYG | ΔCost/ΔQALY | ΔCost/LYG | ΔCost/ΔQALY | ||
| High-income countries | |||||||||||||
| Babela et al., 2022 | Slovakia | — | — | — | — | — | 5012 | — | 2230 | — | — | — | — |
| Naber et al., 2021 | Saudi Arabia | — | — | — | — | — | 15 000 | — | 9367a | — | — | — | — |
| Redwood et al., 2021 | Alaska | — | — | — | — | — | 34 099 | — | — | — | 34 632 | — | — |
| Fisher et al., 2021 | The United States | — | CS | — | — | CS | — | — | — | 7784 | — | — | |
| Peterse et al., 2021b | The United States | — | — | — | — | CS | — | — | — | Dominated | — | — | |
| Barré et al., 2020c | France | — | — | — | Dominatedd | — | — | — | 4544 | — | — | — | — |
| Sekiguchi et al., 2020 | Japan | — | — | — | — | — | CS | — | — | — | — | — | — |
| Coretti et al., 2020 | Italy | — | — | — | — | — | 545 | — | — | — | — | — | — |
| Barichello et al., 2019 | Canada | — | 22,886d | — | — | — | 23 333 | — | — | — | — | — | — |
| Naber et al., 2019e | The United States | CS | — | — | — | CS | — | — | — | CS | — | — | — |
| Miguel et al., 2019 | Portugal | — | — | — | — | — | — | — | 3492 | — | — | — | — |
| Jahn et al., 2019 | Austria | CSd | — | — | — | CS | — | — | — | — | — | — | — |
| Lew et al., 2018a | Australia | — | — | — | — | — | — | 4907 | — | — | — | — | — |
| Senore et al., 2018 | Italy | — | — | — | — | — | — | 458f | — | — | — | — | — |
| Lew et al., 2018b | Australia | — | — | — | — | 11 386 | — | 4907 | — | — | — | 39 161 | — |
| McLeod et al., 2017 | New Zealand | — | — | — | — | — | — | — | 4380 | — | — | — | — |
| Barzi et al., 2017 | The United States | — | — | — | — | CS | — | — | — | — | — | — | — |
| Aronsson et al., 2017 | Sweden | — | — | — | — | — | — | — | 3553 | — | — | — | — |
| Goede et al., 2017 | Canada | — | — | — | Dominatedd | — | — | — | — | — | — | — | — |
| Lew et al., 2017 | Australia | — | — | — | — | — | — | 2473 | — | — | — | — | — |
| Greuter et al., 2017 | Netherlands | — | — | — | — | — | 4300 | — | — | — | — | — | — |
| Ladabaum et al., 2016 | The United States | — | — | — | — | — | CS | — | CS | — | 29 500 | — | — |
| Lee et al., 2016 | Korea | — | 6686 | — | — | — | — | — | — | — | — | — | — |
| Kingsley et al., 2016 | The United States | — | — | — | — | — | CS | — | — | — | 18 543 | — | — |
| Pil et al., 2016 | Belgium | — | — | — | — | — | — | — | 3243 | — | — | — | — |
| Berger et al., 2016 | The United States | — | — | — | — | — | — | — | — | — | 13,168g | — | — |
| Greuter et al., 2016 | Netherlands | — | — | — | — | CS | — | — | — | — | — | — | — |
| Wong et al., 2015 | Hong Kong, China | 53 522 | 7537 | 48 768 | 6727 | — | — | — | — | — | — | — | — |
| Sekiguchi et al., 2015 | Japan | — | — | — | — | — | CS | — | — | — | — | — | — |
| Haug et al., 2014 | The United States | CS | — | — | — | CS | — | — | — | — | — | — | — |
| Ladabaum et al., 2013 | The United States | — | CS | — | — | — | CS | — | — | — | — | — | — |
| Sharaf et al., 2013 | The United States | — | CS | — | — | — | CS | — | — | — | — | — | — |
| Tuan et al., 2013 | The United States | — | — | — | — | — | CS | — | — | — | — | — | — |
| Lansdorp et al., 2013 | The United States | — | — | — | — | — | — | — | — | 18 602 | — | 15 0001 | — |
| Sharp et al., 2012 | Ireland | — | — | — | 6393d | — | — | — | 2449 | — | — | — | — |
| Hassan et al., 2011 | France | 4402 | — | 1612 | — | 9507 | — | 4724 | — | — | — | — | — |
| Heitman et al., 2010 | The United States | — | 10 819 | — | — | — | 2110 | — | — | — | 56 392 | — | — |
| Telford et al., 2010 | Canada | — | 9879 | — | 9403 | — | 6719 | — | — | — | 22 950 | — | — |
| Upper-middle-income countries | |||||||||||||
| Ren et al., 2022 | China | — | CS | — | CS | — | — | — | — | — | — | — | — |
| Cenin et al., 2022 | China | — | — | — | — | 9784 | — | 9620 | — | — | — | — | — |
| Wang et al., 2012 | China | 4306 | — | — | — | — | — | — | — | — | — | — | — |
| Lower-middle-income countries | |||||||||||||
| Tran et al., 2021 | Vietnam | — | 1534 | — | — | — | — | — | — | — | — | — | — |
| Phisalprapa et al., 2019 | Thailand | — | — | — | — | — | 576 | — | — | — | — | — | — |
| Melnitchouk et al., 2018 | Ukraine | — | CS | — | — | — | — | — | — | — | — | — | — |
| Barouni et al., 2012 | Iran | — | 11 271 | — | — | — | 813 | — | — | — | — | — | — |
- Abbreviations: CISNET, Cancer Intervention and Surveillance Modeling Network; CS, cost saving; FIT, fecal immunochemical test; FOBT, fecal occult blood test; LYG, life-year gained; MT-sDNA, multitarget fecal FIT-DNA detection; QALY, quality-adjusted life-year.
- a FIT tests were conducted biennially for people aged 55 to 65 for this study.
- b Peterse et al. (2020) reported ΔCost/ΔQALY as dominated for annual MT-sDNA.
- c Barré et al. (2020) reported ΔCost/ΔQALY as dominated for 2-yearly MT-sDNA.
- d This fecal occult blood test is based on guaiac (gFOBT); other types of fecal occult blood tests are not specified.
- e Naber et al. (2019) obtained the same results using CISNET model (MISCAN-Colon, SimCRC, and CRC-SPIN).
- f FIT tests were conducted biennially for people aged 58 to 69 for this study.
- g Berger et al. (2016) reported ΔCost/ΔQALY as $23 487 for annual MT-sDNA.
Thirty-seven articles have conducted cost-effectiveness on screening strategies beyond fecal screening and no screening (32 from HICs, 2 from UMICs, and 3 from LMICs) (Table 3). Within HICs, only 4 studies examined 5-yearly CTC. One study [26] indicated its CS, whereas another study [37] found it dominated. The lowest ICER value reported was $12 967 [38]. FS was analyzed in 12 studies, with 5 studies (in 10 studies) demonstrating CS for 5-yearly FS. Additionally, one study [39] indicated CS for once FS. A total of 27 articles investigated colonoscopy. Among them, six studies (in 26 studies) found 10-yearly colonoscopy to be CS, whereas one study [28] found it to be surpassed by other strategies. However, the range of ICER values varied significantly from $2859 to $134 351. Furthermore, there were four studies focusing on once colonoscopy, where one study [40] demonstrated CS, whereas another study found it to be dominated by alternative strategies. Both UMICs and LMICs have explored colonoscopy strategies, with relatively low ICER values, reaching as low as $19.
| Author, year | Country | 5-yearly CTC | 5-yearly FS | Once FS | 10-yearly colonoscopy | Once colonoscopy | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| ΔCost/LYG | ΔCost/ΔQALY | ΔCost/LYG | ΔCost/ΔQALY | ΔCost/LYG | ΔCost/ΔQALY | ΔCost/LYG | ΔCost/ΔQALY | ΔCost/LYG | ΔCost/ΔQALY | ||
| High-income countries | |||||||||||
| Naber et al., 2021 | Saudi Arabia | — | — | — | — | — | — | — | 38,821a | — | 9435a |
| Krzeczewski et al., 2021 | Poland | — | — | — | — | — | — | — | — | 6768 | — |
| Redwood et al., 2021 | Alaska | — | — | — | — | — | — | — | 69 261 | — | — |
| Peterse et al., 2021 | The United States | — | — | — | — | — | — | — | 54 412 | — | Dominated |
| Barré et al., 2020b | France | — | — | — | — | — | — | — | Dominated | — | — |
| Sekiguchi et al., 2020 | Japan | — | — | — | — | — | — | — | CS | — | — |
| Barichello et al., 2019 | Canada | — | — | — | — | — | — | — | 46 553 | — | — |
| Naber et al., 2019 | The United States | — | — | Dominated | — | — | — | 24 333 | — | — | — |
| Miguel et al., 2019 | Portugal | — | — | — | — | — | — | — | 134 351 | — | — |
| Jahn et al., 2019 | Austria | — | — | — | — | — | — | CS | — | — | — |
| Wong et al., 2018 | Hong Kong, China | — | — | 63 852 | — | — | — | 49 422 | — | — | — |
| Senore et al., 2018 | Italy | — | — | — | — | CSc | — | — | — | — | — |
| Lew et al., 2018b | Australia | — | — | — | — | — | — | 25 698 | — | — | — |
| Barzi et al., 2017 | The United States | — | — | CS | — | — | — | CS | — | — | — |
| Aronsson et al., 2017 | Sweden | — | — | — | — | — | — | — | 2895 | — | CS |
| Ladabaum et al., 2016 | The United States | — | — | — | — | — | — | — | 15 000 | — | — |
| Kingsley et al., 2016 | The United States | — | — | — | CS | — | — | — | 3831 | — | — |
| Greuter et al., 2016 | Netherlands | CS | — | — | — | — | CS | — | — | — | |
| Hassan et al; 2015 | The United States | — | — | — | — | — | — | 25 807 | — | — | — |
| Wong et al., 2015 | Hong Kong, China | — | — | — | — | — | — | 29 417 | 4650 | — | — |
| Sekiguchi et al., 2015 | Japan | — | — | — | — | — | — | — | CS | — | — |
| Ladabaum et al., 2013 | The United States | — | — | — | CS | — | — | — | 3299 | — | — |
| Sharaf et al., 2013 | The United States | — | — | — | CS | — | — | — | 3350 | — | — |
| Tuan et al., 2013 | The United States | — | — | — | CS | — | — | — | CS | — | — |
| Sharp et al., 2012 | Ireland | — | — | — | — | — | 2659c | — | — | — | — |
| Vanness et al., 2011 | The United States | Dominatedd | — | — | — | — | — | 34,685e | — | — | — |
| Hassan et al., 2011 | France | — | — | 7277 | — | — | — | 16 323 | — | — | — |
| Heitman et al., 2010 | The United States | — | 12 967 | — | 10 382 | — | — | — | 5052 | — | — |
| Telford et al., 2010 | Canada | — | 20 540 | — | 8455 | — | — | — | 6706 | — | — |
| Upper-middle-income countries | |||||||||||
| Ren et al., 2022 | China | — | — | — | — | — | — | — | 128 | — | — |
| Wang et al., 2012 | China | — | — | — | — | — | — | 474 | — | 19 | — |
| Lower-middle-income countries | |||||||||||
| Phisalprapa et al., 2019 | Thailand | — | — | — | — | — | — | — | 730 | — | — |
| Melnitchouk et al., 2018 | Ukraine | — | — | — | — | — | — | — | CS | — | — |
| Barouni et al., 2012 | Iran | — | — | — | — | — | — | — | 10 815 | — | — |
- Abbreviations: CS, cost saving; CTC, computed tomography colonography; FS, flexible sigmoidoscopy; LYG, life-year gained; QALY, quality-adjusted life-year.
- a Colonoscopy test was conducted 10-yearly for people aged 50 to 65, and then once only at aged 55, for this study.
- b Barré et al. (2020) reported ΔCost/ΔQALY as dominated for 10-yearly flexible sigmoidoscopy.
- c Senore et al. (2018) evaluated once-only flexible sigmoidoscopy at age 58; Sharp et al. (2012) evaluated at age 60.
- d Vanness et al. (2011) reported ΔCost/ΔQALY as dominated for 10-yearly computed tomography.
- e Vanness et al. (2011) used Cancer Intervention and Surveillance Modeling Network (CISNET) models for analysis, of which MISCAN-Colon and SimCRC model concluded that the intervention was dominated, whereas only the CRC-SPIN model estimated the ΔCost/LYG at $34 685 (in $2023).
Eight studies have conducted cost-effectiveness comparing new screening strategies to no screening, all of which were from HICs (Table 4). Two studies [29, 31] found that although annual M3CRC and 3-yearly LB have cost-effectiveness, their ICER values were deemed too high. One study [27] found annual and biennial mSEPT9 to be dominated, whereas the other two studies [28, 41] reported ICER values ranging from $12 627 to $193 830 for biennial mSEPT9. Only one article [30] examined annual UMT with an ICER of $38 729. Three articles [27, 28, 32] investigated CCE, with one study [27] finding that 5-yearly CCE was dominated, whereas the other two studies [28, 32] found that 10-yearly CCE was also dominated. However, there was one study [26] that reported CS for 5-yearly MRC screening.
| Author, year | Country | Annual mSEPT9 | 2-yearly mSEPT9 | Annual UMT | 5-yearly CCE | 10-yearly CCE | 5-yearly MRC | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ΔCost/LYG | ΔCost/ΔQALY | ΔCost/LYG | ΔCost/ΔQALY | ΔCost/LYG | ΔCost/ΔQALY | ΔCost/LYG | ΔCost/ΔQALY | ΔCost/LYG | ΔCost/ΔQALY | ΔCost/LYG | ΔCost/ΔQALY | ||
| High-income countries | |||||||||||||
| Peterse et al., 2021 | The United States | — | Dominated | — | Dominated | — | — | — | Dominated | — | Dominated | — | — |
| Barré et al., 2020 | France | — | — | — | 193 830 | — | — | — | — | — | Dominated | — | — |
| Barichello et al., 2019 | Canada | — | — | — | — | — | 38 729 | — | — | — | — | — | — |
| Greuter et al., 2016 | Netherlands | — | — | — | — | — | — | — | — | — | — | CSa | — |
| Ladabaum et al., 2013 | The United States | — | — | — | 12,627b | — | — | — | — | — | — | — | — |
| Hassan et al., 2011 | France | — | — | — | — | — | — | 29 722 | — | 18 357 | — | — | — |
- Abbreviations: CCE, colon capsule endoscopy; CS, cost saving; LY, life-year; MRC, magnetic resonance colonography; mSEPT9, methylated Septin 9 blood test; QALY, quality-adjusted life-year; UMT, urine metabolomic test.
- a Greuter et al. (2016) reported ΔCost/ΔQALY as CS for 10-yearly magnetic resonance colonography.
- b Ladabaum et al. (2013) evaluated two types of methylated Septin 9 DNA agents. The ΔCost/ΔQALY for the third aliquot is $10 660, whereas the result for two plasma aliquot is in the table.
The optimal strategies at different WTP levels (range $5000–100 000/QALY) are shown in Table S10. A total of seven studies evaluated the six common strategies (annual FOBT and FIT, biennial FOBT and FIT, 5-yearly FS, and 10-yearly colonoscopy) and the no-screening strategy, with MT-sDNA and CTC not included due to limited articles. Four studies in the United States all found 10-yearly colonoscopy optimal. Among other three studies found different optimal strategies for different WTPs. Tuan et al. [33] evaluated annual and biennial FIT, 5-yearly FS, 10-yearly colonoscopy, and no-screening strategy (strategies compared ¼ “All but FOBT”) and found that annual FIT was the optimal strategy when WTP was below $100 000, whereas a 10-yearly colonoscopy became the preferred choice when WTP exceeded $100 000.
4 Discussion
We conducted a comprehensive systematic review of the literature to identify model-based economic evaluations of CRC screening across countries with varying income levels. The review included 56 studies from three countries with different income levels. We observed significant variations in the effectiveness of common screening strategies. Fecal-based methods have lower sensitivity and specificity compared with endoscopic examinations but are much less costly. The differences between countries with different income levels were not significant, except that sensitivity estimates for FOBT were higher in LMICs. New screening methods typically exhibit higher sensitivity and specificity than common strategies but come at a higher cost. Among them, the MRC strategy was found to have high sensitivity as a noninvasive screening strategy, with relatively low cost. This is consistent with the results of two previous systematic review studies. One article [42] reported a sensitivity of 91.7% and specificity of 96.5% for lesions greater than or equal to 10 mm for experienced readers. Another study [43] found that magnetic resonance colonography had a sensitivity of 83.8% and specificity of 95.3% for late-stage tumors.
We extracted additional items from the original systematic review to provide a more comprehensive description of the different modeling approaches used. The studies showed significant differences in these approaches, which may lead to variations in the results. One of the key differences lies in the choice of health states for the model. Globally, CRC has two major distinct precursor pathways [44]: the conventional adenoma-carcinoma pathway, which accounts for 70%–90% of cases, and the serrated pathway, which leads to the formation of serrated polyps and accounts for 10%–20% of cases. Consequently, studies that solely simulate the entire progression of CRC through the conventional adenoma-carcinoma pathway may yield inaccurate estimates of screening outcomes. Moreover, the failure to consider nonadvanced adenomas in some studies can lead to an overestimation of CRC incidence and the cost-effectiveness of screening strategies. Furthermore, numerous modeling assumptions/parameters are based on models from different countries. Hence, it is crucial to perform internal and external validation of the model once it has been developed.
We found that CS accounted for a higher proportion of the annual FIT and the 10-yearly colonoscopy strategy in HICs than in UMICs and LMICs, for which we specifically analyzed information for studies that included these two screening strategies (Tables S11 and S12). The analysis revealed that national healthcare expenditures exhibited minimal variation among HICs and were higher than in UMIC and LMIC countries. Additionally, adherence rates and colonoscopy expenditures synergistically influenced the cost-effectiveness of screening strategies, with the potential for greater CS when adherence rates were higher and expenditures were lower. We did not observe any significant differences in cost-effectiveness of other screening programs based on country income level. This may be due to the limited and smaller number of screening types included in both UMICs and LMICs. Large differences were observed among different screening strategies, with more studies on annual FIT and 5-yearly FS being CS, but colonoscopy being the most cost-effective screening method at different WTP thresholds. Other common screening strategies were almost cost-effective according to national income thresholds, even UMICs. Most new screening strategies, except for 5-yearly MRC, were dominated, with ICERs reported between $12 627 and $38 729, only being below per capita GDP in HICs. Although some reviews have indicated that MRC has a high diagnostic value for CRC [45-47], there are no long-term population-based cohort studies to confirm that MRC reduces CRC morbidity/mortality. Future research should address this gap to more accurately assess the comprehensive clinical benefits of MRC. When considering whether to implement a new screening strategy, the impact of the disease on the local financial burden and the local medical capacity should be considered. Early local implementation of some population-based projects with new screening strategies may inform future decisions on screening strategies in UMICs and LMICs.
Our review had several limitations. First, the majority of studies did not specify the type of FOBT used, except for two articles that mentioned the use of guaiac-based FOBT (gFOBT). Additionally, a significant portion of the studies did not specify the brand name of the reagents used, making it difficult to make accurate assessments. Secondly, our literature search was limited to English articles, which means that studies describing cost-effectiveness analyses in languages other than English could not be included. This limitation may result in an incomplete evaluation of the available evidence. Thirdly, although our study aimed to comprehensively search for studies from countries with different income levels, there were limited studies available from UMICs and LMICs. Moreover, among the included UMICs, only China was represented, which may limit the generalizability of the cost and effectiveness findings to the overall UMICs. Lastly, our review primarily focused on single-method strategies. If combination strategies become more widely adopted in the future, evidence regarding the cost-effectiveness of such strategies should be included.
In conclusion, studies identified in this systematic review focused on the cost-effectiveness of CRC screening strategies in countries with different income levels. Most studies found that commonly adopted strategies including annual and biennial gFOBT, annual and biennial FIT, 3- or 5-yearly MT-sDNA, 5-yearly CTC, 5-yearly FS, 10-yearly colonoscopy, once FS/colonoscopy, and newer strategies such as 5-yearly MRC were cost effective compared with no screening. Comparisons between strategies found colonoscopy and FIT screening to be more cost-effective than other strategies. There were no significant differences between results from different income countries. Whether novel screening strategies should be implemented in UMIC and LMIC requires a large population-based study before it can be determined.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or non-for-profit sectors.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data supporting the findings of this study are available upon request from the corresponding author.