Gastrointestinal: Solid pseudopapillary neoplasm of the pancreas with high-grade malignant transformation
A 64-year-old man undergoing postoperative follow-up for colon cancer was incidentally found to have a 40-mm pancreatic head mass on a computed tomography (CT) scan (Fig. 1a). The tumor had increased in size over the past 12 months of follow-up. On heavy T2-weighted magnetic resonance imaging (MRI), the main pancreatic duct (MPD) near the mass was dilated and disrupted, with unclear demarcation in some areas, suggesting tumor invasion of the MPD (Fig. 1b). Diffusion-weighted imaging showed high signal intensity tumor, with apparent diffusion coefficient (ADC) value being 0.7 × 10−3 mm2/s (Fig. 1c,d). Duodenoscopy revealed irregular nodular mucosa in the papilla of Vater, suggestive of tumor invasion. Endoscopic ultrasonography (EUS) revealed a mass with distinct borders in the pancreatic head, part of which protruded into the MPD with suspected invasion (Fig. 1e).
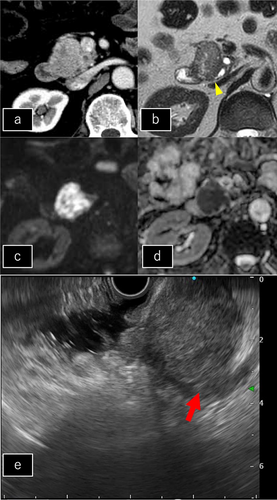
EUS-guided fine-needle biopsy confirmed the diagnosis of a solid pseudopapillary neoplasm (SPN). The patient subsequently underwent a subtotal stomach-preserving pancreatoduodenectomy.
Macroscopically, the tumor presented as a solid mass with a variegated appearance and had invaded the MPD, which was confirmed by microscopic examination (Fig. 2b). Microscopically, the tumor cells proliferated mostly in trabecular and alveolar patterns in the background of the mucinous stroma, with inconspicuous pseudopapillary structures (only focally found). Nuclear atypia and pleomorphisms with abundant mitotic figures were observed (Fig. 2a). The Ki-67 labeling index was 63% in the hot spot, suggesting high malignant potential. Nuclear pleomorphism, high-grade atypia, and abundant mitotic figures indicated pleomorphic-type SPN with high-grade malignant transformation. One year postoperatively, metastases developed in the para-aortic lymph nodes and liver.
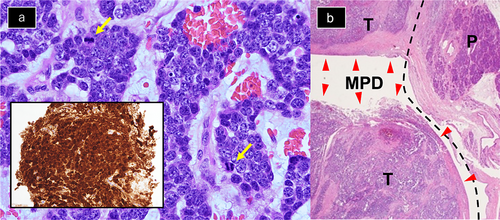
SPN is a rare tumor that accounts for 0.9–2.7% of all pancreatic tumors, with 90% of cases occurring in women.1 SPN is generally considered low-grade, with a reported 5-year survival rate of 95–97%, although poor prognoses have been reported in middle-aged male patients.2 Metastasis or recurrence can be fatal, and many cases are associated with an undifferentiated component, referred to as an SPN, with high-grade malignant transformation. In this case, macroscopic invasion of the SPN into the MPD was suggested by preoperative EUS and MRI and confirmed by the pathological analysis. MPD dilatation due to the SPN has been reported; however, to the best of our knowledge, this is the first report in which the invasion of the SPN into the MPD could be suspected by preoperative EUS and MRI. Furthermore, the low ADC value in our case also suggested high-grade malignancy, in contrast to the generally reported high ADC values of SPN (1.16 ± 0.36 × 10−3 mm2/s).3
Although SPN is generally considered to have a good prognosis, patient with SPN suspected of having high-grade malignant transformation by preoperative EUS and MRI, as in our case, should be carefully treated.