Hepatobiliary and Pancreatic: Challenges in the diagnosis of hepatic nodules in patients with alcoholic liver cirrhosis
A 57-year-old male patient, who has an alcoholic liver cirrhosis (LC) and a history of splenectomy due to traffic accident, was referred to our hepatobiliary center for further evaluation of a 1.3 cm sized hepatic nodule in segment 6 on liver dynamic computed tomography (CT). The lesion showed arterial enhancement on the arterial phase (Figure 1a) along with delayed washout (Figure 1b). Physical examination was normal and the viral markers for hepatitis B or C were negative. Liver function tests showed total bilirubin, 0.4 mg/dL; albumin, 4.8 g/dL; aspartate aminotransferase, 46 U/L; alanine aminotransferase, 18 U/L; and gamma glutamyl transferase, 433 U/L. Tumor markers, including alpha-fetoprotein (3.19 ng/mL), CA 19-9 (24.2 ng/mL), and Des-gamma-carboxy-prothrombin (27.09 mAU/mL), were within normal limits. To further evaluate the lesion, dynamic magnetic resonance imaging (MRI) with Primovist (Gadoxetate disodium) was performed. The lesion showed arterial enhancement on arterial subtraction image (Figure 1c) and low signal intensity on 20-min delayed image (Figure 1d). In addition, a 1.7 cm enhancing lesion was also found on the hepatic dome (Figure 1e). Based on the image findings and the patient's history of liver cirrhosis and splenectomy, hepatocellular carcinoma (HCC) and intrahepatic splenosis should be differentiated on the lesions (Fig. 1). On magnetic resonance imaging (MRI), thin hypointense rim around the mass on T1- (Fig. 2a,b) and T2-weighted image (Fig. 2c,d) was identified. The lesions also showed high signal on diffusion-weighted image (Fig. 2e) along with low signal on apparent diffusion coefficient image (Fig. 2f). Therefore, the patient was diagnosed with intrahepatic splenosis and a 6-month follow-up CT scan revealed no interval changes in these lesions.
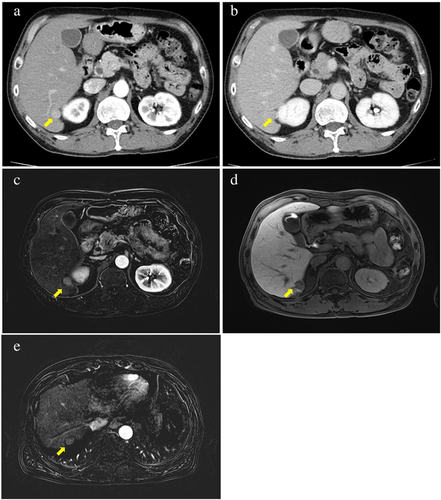

Intrahepatic splenosis, an autotransplantation of splenic tissue, can develop in patients who experienced splenic rupture or splenectomy. Intrahepatic splenosis can shows enhancement on the arterial phase and washout on the delayed phase of CT and MRI, which can be confused by HCC. In patients at high risk for HCC, such as the one with cirrhosis in this case, HCC should be considered as a differential diagnosis. However, thin hypointense rim surrounding the lesion on T1- and T2-weighted images due to fat or fibrous capsule are characteristic findings of splenosis, which can differentiate splenosis from HCC. Moreover, restricted diffusion with lowest apparent diffusion coefficient value, a common feature of spleen, is helpful for diagnosing splenosis. Additionally, when available, further examinations using SPIO contrast-enhanced MRI, contrast-enhanced ultrasound, and technetium-99 m-labeled heat-denatured red blood cells can be instrumental in diagnosing splenosis. In conclusion, to avoid unnecessary biopsy or surgery, it is crucial to carefully evaluate the patient's history and MRI for diagnosing intrahepatic splenosis, particularly in patients with liver cirrhosis, a risk factor for HCC.