Gastrointestinal: Endoscopic submucosal tunnel dissection for an esophageal bronchogenic cyst
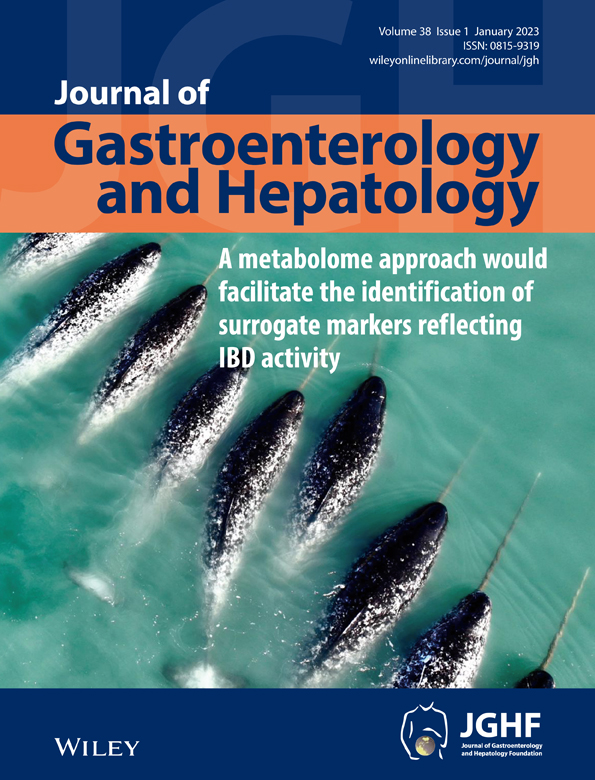
A 46-year-old woman was referred to our hospital for endoscopic resection of an esophageal submucosal lesion that was gradually increasing in size. She did not report symptoms and her physical examination was unremarkable. Abdominal contrast-enhanced computed tomography revealed a 3.2 × 2.7 cm well-defined and low-density mass at the lower end of the esophagus (Fig. 1a). Endoscopy showed a bulging lesion above the cardia (Fig. 1b). Endoscopic ultrasonography examination revealed a hypoechoic lesion arising from the muscular propria (Fig. 1c). Endoscopic submucosal tunnel dissection (ESTD) was performed to expose the intact lesion between the mucosa and muscular layer of the esophagus (Fig. 2a). As continued dissection was difficult, we excised the lesion, confirming it as a cyst. Some yellowish milky fluid was also noted (Fig. 2b). Subsequently, ethanol ablation of the cyst wall was performed with 95% ethanol (Fig. 2c). The mucosal entry was closed with titanium clips. Histopathology showed a ciliated columnar epithelium lined cyst wall, which was consistent with the diagnosis of the bronchogenic cyst (Fig. 2d,e). The patient was discharged without any adverse events. During 3 years of follow-up, endoscopy showed the disappearance of the cystic lesion (Fig. 2f).
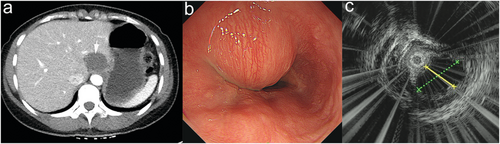
Bronchogenic cysts are congenital malformations derived from the primitive foregut with abnormal budding. This could occur in the mediastinum and pericardium, but is rarely reported in the esophagus. ESTD has been demonstrated safe and effective, but the risk of incomplete dissection exists. In this case, we combined the use of ESTD for the treatment of a bronchogenic esophageal cyst and 95% ethanol for the cyst remnants.