Dimensions of Posterior Implant Restorations Related to Intra-Coronal Cantilever and Occlusal Forces: An In Vitro Study
ABSTRACT
Objective
The aim of the present study was to investigate the relation of the implant position to the implant crown and analyze the location and magnitude of bite force.
Materials and Methods
The dimensions of 49 posterior implant-supported restorations were recorded in terms of: 1. implant diameter, 2. crown length, 3. crown width, 4. crown height, 5. occlusal surface of the restoration. The crown/implant height was measured and the distance between the implant center and the restoration center revealed the size of intra-coronal cantilevers. The occlusal force analysis determined the point and magnitude of loading. Correlation coefficient r was used for the statistical process and statistical control was carried out with the aid of t-test with minimum level of significance p < 0.05.
Results
- -
The mean crown-to-implant ratio was 0.9 and in short implants (< 10mm) the ratio was 1.28.
- -
Intra-coronal cantilever extensions ranged from 2.1 mm to 6.35 mm depending on crown size.
- -
Occlusal loading was identified in cantilever areas of the crown.
Conclusions
- -
Implant center deviates from crown center in 71%–82% of the cases depending on site location.
- -
Implants with non-ideal position may support a functionally occluding crown.
Clinical Significance
Intra-coronal cantilevers are a critical factor to avoid clinical complications and should be taken under consideration both in the planning and fabrication phase of implant restorations.
1 Introduction
Correct diagnosis and accurate treatment planning can ensure more predictable results during clinical practice [1]. An implant is regarded as “successful” when it is not only osseointegrated but also it supports an esthetically, functionally and biologically accepted restoration [2]. Consequently, the correct implant position may be a significant factor for successful long clinical function. The ideal implant position is determined during the pre-surgical treatment planning and the design of the optimum final restoration. Design of implant-supported restorations is influenced by numerous factors, which are related to the longevity of the restoration and the prevalence of complications.
Implant placement is nowadays prosthetically driven. The fabrication of radiographic and surgical guides combined to the use of CBCT can contribute to the determination of the prosthetically ideal implant position [3].
Digital technology has contributed significantly to more accurate presurgical planning and guided implant placement can lead to a predictable outcome concerning the position and the inclination of implants in relation to the final restoration [4, 5]. Although it is a promising technology with steadily increasing accuracy that facilitates both planning and surgical phase, many clinicians still use the free hand placement [6, 7]. Guided implant placement also has certain limitations (e.g., reduced mouth opening, additional presurgical stages, increased cost) that does not always allow its use in the everyday clinical practice [8, 9].
Insufficient bone substrate, absence of bone augmentation, poor presurgical planning and/or incorrect handling during the surgical phase may result in deviation of the implants from the ideal position. The frequency of biologic and mechanical complications may be higher in such cases [10, 11].
Implant dimensions relate to the design and morphology of the prosthetic restoration [12, 13] and are in accordance with bone volume, site of implantation and magnitude of functional load generated [14, 15]. Various studies have validated the high survival rates of single implants [16-18] yet at the same time many papers report different types of prosthetic complications [18, 19] many of which relate to force distribution and the platform size of the implant [20, 21]. Especially for single implants in the posterior region, diameter does not have an effect on survival [22-25] but relates to crown dimensions and the non-axial loading that width discrepancies may incur [22, 23, 26]. Variations in implant size, number and prosthetic design are responsible for the presence of cantilevers that although present no validated relationship with bone loss [27-29], they have a strong association with prosthetic complications [30, 31]. Cantilevers incorporated in full arch restorations [32, 33] differ from intra-coronal cantilevers in the rate and types of complications that may develop [34-38]. Clinical efforts have been made to address the anatomical limitations [39, 40] to better control the functional overloading [41-43] or to maximize the implant distribution [44, 45] resulting in cantilevers of various extension and morphology. Occlusal forces on prosthetic restorations and their control in terms of pattern, magnitude and area of development [46-48] is important for minimizing the risk of complications especially in single implants where unfavorable crown to implant ratios incorporate detrimental lever arms in the prosthetic components [49].
2 Aim
Single implants and their supporting restorations may not have the ideal 3D alignment and depending on implant size and crown volume, intra-coronal cantilevers may develop. For this reason, functional loading on cantilever portions may be responsible for technical complications. The aim of the present study was to investigate the spatial correlation of the implant and implant restoration and look into the location and magnitude of functional loading on the prosthesis.
2.1 Research Hypotheses
- Implant center and long axis coincide with the center of the crown.
- Occlusal loading is developed in the central area of the implant crown.
3 Materials and Methods
Forty-nine fixed implant-supported restorations placed in 18 patients were included in the present study. Only single-tooth restorations on internal connection implants were studied. For multi-unit restorations only the abutment crowns on implants were recorded and considered as a single unit.
The clinical stages of the restorations were performed in the post-graduate Clinic of Prosthodontics in the Dental School of the University of Athens.
Pre-surgical treatment planning, fabrication of radiographic and surgical guides and the prostheses' clinical stages were carried out by the post-graduate students of Prosthodontics under supervision of staff members. Implant placement was carried out by the post-graduate students of Periodontology. The prosthetic restorations were fabricated by selected dental laboratories cooperating with the postgraduate Clinic. Measurements were performed on the working cast prior to delivery by the same clinician with a digital caliper.
To test the first hypothesis the following parameters were recorded: Implant diameter, length of occlusal surface (mesial-distal), width of occlusal surface (buccal/palatal-lingual), height of the implant crown, occlusal table area, intra-coronal cantilevers, and distance between the implant center and the restoration center. The shape of the occlusal table was considered as rectangular, and its area was calculated approximately by multiplying the length by the width of each occlusal unit.
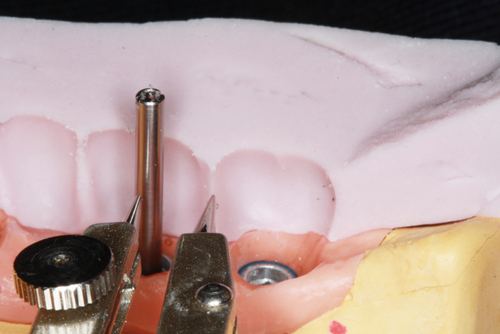
For the measurement of the intra-coronal cantilevers, silicon matrices of the final restorations were fabricated. A long screw representing the implant center was fixed on the master cast. The silicon matrix was cut in two equal parts, a buccal and a lingual part. After the adjustment of each part to the master cast, the distance between the screw (indicating the implant center) and the buccal, lingual, mesial and distal surface was measured with the aid of a measuring compass with pointed ends (Figure 1).
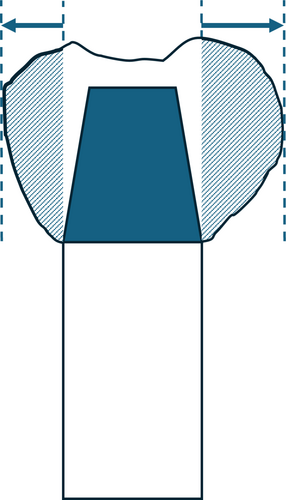
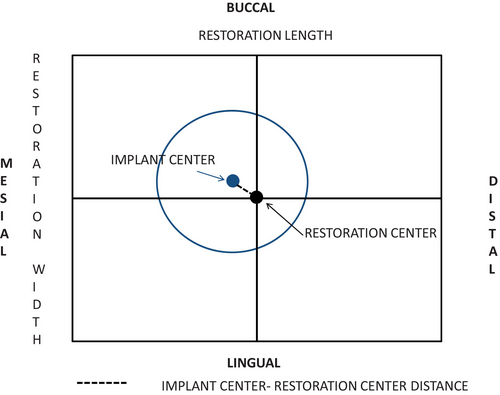
- The restoration was designed in a graph paper as viewed from the occlusal side in the form of a rectangular figure. The figure's length and width represented the restoration's length and width (Figure 3).
- The figure's center was defined as representing the center of the restoration. The two-dimensional position of the implant and its center as well, were designed to the figure according to the implant diameter and the intra-coronal cantilevers' measurements.
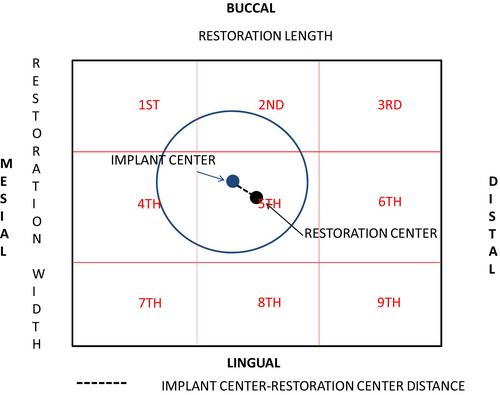
- Following this, the restoration-rectangular figure was divided in nine equal sections as shown in the diagrams in Figure 4.
- Finally, the particular section which contained the implant center was defined.
To test the second hypothesis, the next phase of the study was carried out. Following delivery of the restoration, an occlusal analysis was performed in eight out of the 18 patients of the first phase, carrying 26 restorations in total utilizing the T-Scan III device (T-scan III Pressure Management System, Tekscan Inc., USA).
T-Scan III registers occlusal contacts and analyzes the registration's data which pertain to the point, time, and magnitude of bite forces. More specifically, it is similar to an electronic articulation paper, containing strength receptors for the measurement of force's magnitude and distribution.
T-Scan III has an electronic holder where the registration sensor is adapted. The registration data were transferred and analyzed by the corresponding software.
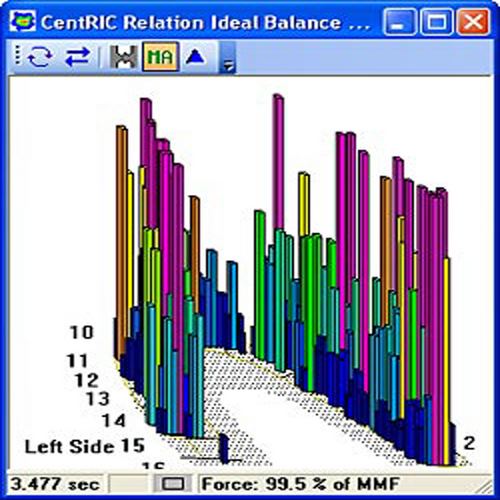
During the present study, T-Scan III registration's data were analyzed to specify the point of the implant restoration's occlusal surface where maximum occlusal force is applied. The maximum force application point was specified with the aid of the three-dimensional imaging of patient's bite registration.
As seen in Figure 5 the rods depict the bite forces. The color and height of the rods vary according to the forces' magnitude. More specifically, the highest rod corresponds to the maximum force application point, which then can be specified in the two-dimensional imaging with the aid of the color graduation (Figure 6).
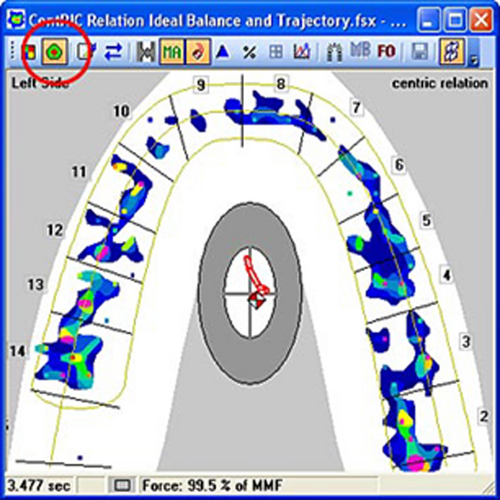
The midline was used as a reference point, to compare the first with the second phase's data. The midline was consistent both in the master cast and the two-dimensional imaging of the electronic bite registration.
Initially, a long laboratory screw was screwed to the implant analog to define the implant center to the master cast. The distance between the implant center and the midline was measured then. This distance was transferred to the two-dimensional imaging relating the implant center to the registration's diagram. The distance between the implant center and the maximum force application point was subsequently calculated. The aforementioned distance was compared to the implant radius. When this distance was bigger than the implant radius, the bite force was applied on a cantilevered point and these data were recorded.
Furthermore, T-Scan III device records the percentage of the total biting force, which is applied to each occlusal unit. This information related to completed restorations was recorded for further analysis.
In the first phase of the experimental procedure the intra-coronal cantilever was calculated. In the second phase, the exact point of application of the maximum occlusal force was determined. This point could be located either inside or outside the implant periphery. In the second case occlusal loading was taking place on the intra-coronal cantilever area.
Statistical analysis was carried out using Matlab Statistical Program (Matlab R 2013a). Correlation coefficient r was used for the statistical process and statistical control was carried out with the aid of t-test with minimum level of significance p < 0.05.
4 Results
Eihgteen patients participated in the present study with 49 implant-supported cement-retained restorations that were examined and analyzed. Twenty-five restorations replaced premolars (13 maxillary and 12 mandibular) whereas 24 (8 maxillary and 16 mandibular) were molar crowns.
A possible correlation between the implant position and the dimensions of the restoration was investigated. A further correlation between force distribution, implant diameter and occlusal surface of the restoration was investigated.
4.1 Implant Diameter and Occlusal Surface of the Restoration
As can be seen in Figure 7 most premolar implants were either 3.8 or 4.1 mm. The mean width of premolar crowns was 8.3 mm.
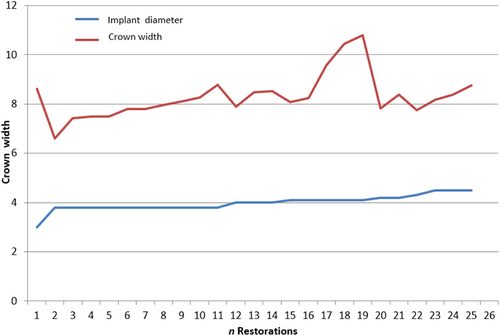
The implant diameter for molar restorations ranged between 3.8 and 6 mm (Figure 8). According to the diagram, concerning the statistical sample of molars, the width of the crown was increased. The mean of molar crown's width was 9.2 mm.
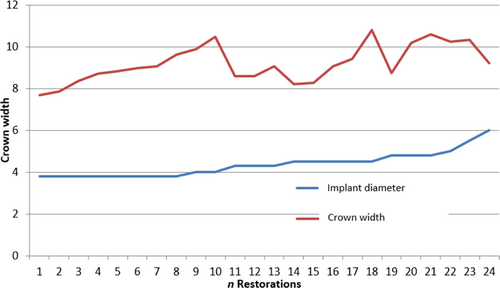
The correlation coefficient r for the pre-mentioned pair of variables was 0.42. The correlation between the two variables was moderate and statistically significant. (t = 3.13, statistical level of significance p < 0.001).
4.2 Measurement of Intra-Coronal Cantilevers
Table 1 displays the minimum, the maximum and the mean value of the intra-coronal cantilevers that were measured. The highest values were recorded for the lingual/palatal cantilever, which means that higher discrepancies relate more to implant position in a lingual/palatal direction.
| Mean (mm) | Min (mm) | Max (mm) | |
|---|---|---|---|
| Mesial cantilever | 2.226 | 0.170 | 6.080 |
| Distal cantilever | 2.116 | 0.230 | 5.570 |
| Buccal cantilever | 1.791 | 0.150 | 4.510 |
| Lingual/palatal cantilever | 2.804 | 0.400 | 6.350 |
Concerning mesial/distal direction, the maximum value of the mesial cantilever was the highest recorded. However, the difference between the mean value of the mesial and the mean value of the distal cantilever was not increased.
4.3 Distance Between implant's Center and restoration's Center
Table 2 displays the minimum, the maximum and the mean value of the distance between implant's center and restoration's center, as it was measured with the aid of the rectangular figure of Figure 5.
| Premolars | Molars | |
|---|---|---|
| Mean value (mm) | 1.392 | 1.427 |
| Min value (mm) | 0.350 | 0.250 |
| Max value (mm) | 3.250 | 3.650 |
In Figure 9 the restorations' distribution per section containing implant center is shown. The section containing the implant center was defined with the aid of the rectangular figure of Figure 5.
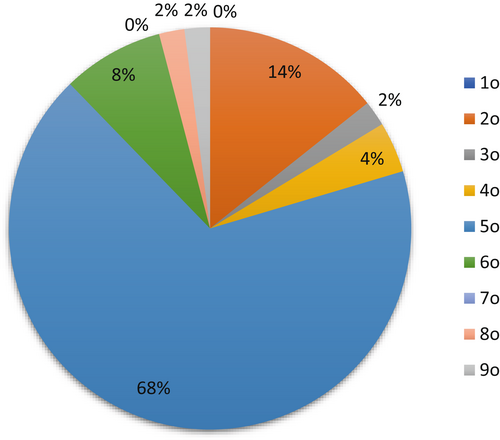
The coincidence of the implant and restoration centers in the 5th section was present for 68% of the cases. The corresponding numbers for the rest of the sections were as follows: in the 2nd section for 14%, in the 6th section for 8%, in the 4th section for 4%, in the 3rd for 2%, in 8th for 2% and in the 9th section for 2% of the restorations.
4.4 Measurement of Occlusal Force
In the second phase of this study the percentage of the total biting force which is applied to each occlusal unit of the implant restoration was recorded by means of the t-scan device. Eight out of 18 patients responded to the recall appointment and 26 out of 49 implant restorations were tested The min value was 0%, the max value 45% and the mean 15% of the total occlusal force.
4.5 Distance Between Implant Center- Point Application of Maximum Force
In cases where the distance between implant center and the point of maximum force application is beyond the implant radius, an intra-coronal cantilever is created.
Intra-coronal cantilever was created in 10 of the 14 premolars' restorations (71% of the total amount). The minimum value was 0.1 mm, the maximum 2.1 mm and the mean 1.095. In 50% of the restorations, cantilever's direction was distal, in 30% the direction was labial, in 10% mesial and in the last 10% palatal/lingual.
Intra-coronal cantilever was created in 9 of the 11 M' restorations (82% of the total amount). The minimum value was 0.1 mm, the maximum value 4 mm and the mean 2.18 mm. In 55% of the restorations, cantilever's direction was mesial, in 22% the direction was distal, in 11% buccal and in the last 11% palatal/lingual.
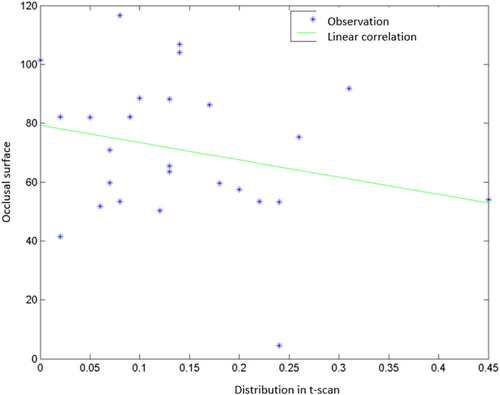
4.6 Force Distribution-Occlusal Surface of the Restoration
The force distribution was correlated to the occlusal surface of the restoration (Figure 10). The r correlation coefficient for the two variables was −0.25 indicating a moderate negative correlation (t = 1.69, p < 0.1). This finding can be explained as the force is diminished when applied to a greater surface but not proportionally. The correlation was not statistically significant.
5 Discussion
The first hypothesis was validated for the majority of the implant crowns. Although implant placement was not facilitated with a surgical guide, implant center was in close proximity with the crown center in the middle third (2–5–8 sections) of 84% of the restorations. Manual placement can be performed in different ways with a varying degree of guidance [6, 7]. In this study, implant placement was initiated with marking in the center of the edentulous ridge and then use the sequence of indicated drills. Deviation during drilling has an effect in the inclination of the implant long axis, resulting in discrepancy with crown center.
The second hypothesis was not validated since for the majority of the restorations (71%–82%) occlusal loading was taking place in a point of intra-coronal cantilever. Cantilever extensions were varying in length and their clinical effect should be evaluated in accordance with crown dimensions, opposing dentition, implant size and magnitude of bite force [42, 47].
Distribution of forces is affected by the three-dimensional implant location [20]. If the implant center diverts from the restoration's center, the applied forces may lead to screw loosening or fracture of implant abutments. Higher occlusal forces in the posterior regions, lateral forces related to the cusps' inclination and bruxism are additional factor causing excessive forces. Repeated screw loosening may indicate non-passive fit, incorrect design of the occlusal surface and/or occlusal overloading, thus being a warning for further complications, if the causing factors aren't successfully encountered. The role of diameter to implants' survival rates has been reported as secondary. The main determinant factors are: optimal operating protocol, adequate initial implant stability and effective oral care [25].
Despite the high survival rates of implant restorations, the occurrence of mechanical complications is frequent and could possibly be related to the implant diameter. In cases of molar restorations, intra-coronal cantilevers are inevitably created. Reducing the occlusal surface of the restorations has been suggested to reduce these cantilevers [22, 23]. In the present study standard diameter implants were used in 13 cases (54%) and wide diameter implants in the remaining cases (56%). In cases where the width of the alveolar ridge was reduced, the restoration's width was not reduced respectively, thus increasing the surface where non-axial forces could be applied [26].
Intra-coronal cantilevers are observed when the implant position is not ideal prosthetically. The mean value of the distance between the aforementioned parameters was 1.392 mm for the premolar restorations and 1.427 mm for the molar restorations. Furthermore, the implant center was in the same section, 5th section (Central section) as it is shown in the diagram (Figure 8) with the restoration's center in 68% of the restorations. The measurements were related to the cantilevers created from unfavorable implant position. During clinical function of the restorations, cantilevers transfer occlusal forces to the restoration, exerted beyond the implant periphery. When the distance between the implant center and the point of application of the maximum force was measured, the results were the following: a. cantilever was observed in 71% of the premolar restorations (maximum value 2.1 mm) and in 82% of the molar restorations (maximum value 4 mm). The maximum value for the molar restorations was double compared to that of premolar restorations. This occurs because even though molars have larger dimensions than premolars, the supporting implant may have the same diameter.
Intra-coronal cantilevers were measured towards all directions. The highest numerical values were recorded for the lingual/palatal cantilever, indicating higher discrepancies in implant position buccally. Concerning mesial/distal direction, the maximum value of the mesial cantilever was recorded. However, the mean values of the mesial and distal cantilever were comparable. Mean values of the mesial, distal, buccal and palatal/lingual cantilever were 2.226, 2.116, 1.791 and 2.804 mm respectively. Prosthetically driven implant installation is the current dogma to ensure health and esthetics. In this study diagnostic wax-up determined the indicated prosthetic restoration and surgical guide was used for the initial pilot drilling. Subsequent implant site preparation was performed free hand. Multiple unit implant restorations were included in the study and only the implant crowns (not the pontics) were included in the analysis. Implant site preparation in these cases followed the same protocol and possible divergence of implant long axis was limited within the volume of the a single prosthetic unit since final restoration was a duplicate of the diagnostic wax-up.
In a clinical study the mesial and the distal cantilever were measured radiographically [27]. The values measured were 2.75 ± 1.65 mm and 2.24 ± 1.6 mm respectively. Non-statistical difference in bone loss was found with molars and premolars and cantilevers could not be related to bone loss. The results of two other clinical studies were similar concerning the bone loss observed in restorations with and without cantilevers [28, 29].
Cantilevers have been considered as mechanical risk factors because these restorations are more susceptible to bending forces. The frequency of technical complications' occurrence in cases of restorations with cantilevers has already been reported [30]. The cantilever length is the determinant factor as it is related to magnification of occlusal forces. When the mesial- distal dimension of the cantilever is increased, the compressive and the tensile forces are increased too [31]. The effect of an intra-crown cantilever on the longevity and the possible complications of a single implant crown has not been investigated thoroughly in the literature. In our study intra-crown cantilever was measured in order to confirm the magnitude of its existence. Cantilever was determined with reference to the point of occlusal contact on the restoration surface. However, implant inclination has an effect on the vector of the developed occlusal force and pattern of functional loading. The mode of prosthesis retention, either cemented or screw retained also plays a role on the type of complications that may arise. Future studies could examine the prevalence of complications in association with functional loading of intra-crown cantilevers. Lateral forces on the implant crown may predispose for screw loosening [34-36]and intra-coronal cantilevers were shown as predisposing factor for mechanical complications [37]. In an extended systematic review focused on the factors associated with loosening of the abutment screws, intra-coronal cantilevers increased the risk of screw loosening [38].
In a systematic review focused on single implant supporting two-unit cantilever Fixed Dental Prostheses, the implant survival was 97%–100% but the rate of technical complications was increased. Similar findings were reported in another clinical trial with 3 years follow-up [39, 40]. An implant molar crown supported by an implant positioned in the distal or mesial root has mechanical similarity to a two-unit single-implant restoration located in the area of the maximum occlusal force. In a clinical trial statistically significant difference was found in the rate of prosthetic complications between molar crowns supported by one compared to two implants [41]. On the other side in two clinical trials for implants replacing a single molar no difference was found between restorations supported by one or two implants and no significant rate of technical complications [42, 43].
A consensus report of the European Association of Osseointegration based on a systematic review concluded that there is evidence for the successful use of cantilevers in partially edentulous patients but the reported complication rate was higher both on a patient and a prosthesis level [44].
The position, length and the diameter of the implant, the abutment's height, the shape and size of the occlusal surface, the initial torque of the fixing screw, the passive fit of the restoration and the frequent and detailed control of occlusion must be taken into account, not only during treatment planning but also during follow-up, to ensure long-term survival of the restorations [31, 37, 38].
In this study, the presence of intra-coronal cantilevers was confirmed in various directions of the prosthetic restoration. The extend of the cantilever part, the location of the occlusal contact, the magnitude of functional loading, the dimensional parameters of the implant components, the material selection and morphology of the prosthesis are critical factors for the development of clinical complications and should be taken into consideration during the planning and restorative phase.
The present study had the following limitations: it included only cement-retained posterior implant restorations and the occlusal measurements were recorded only in static relation. Further clinical trials are needed to establish a sound conclusion on the effect of intra-coronal cantilevers on the clinical function of fixed implant restorations.
6 Conclusions
Within the limitations of this study, implant center although coinciding with central portions of the crown, leads to the development of cantilever segments that participate in functional loading. Location of cantilever extension and magnitude of loading force should be clinically evaluated upon delivery of the prosthesis.
Disclosure
The authors do not have any financial interest in the companies whose materials or devices are included in this article.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.