Association of depression with hypertensive left ventricular hypertrophy in age, sex, and education level-specific differences
Abstract
Previous studies have shown that hypertension and depression are associated with worse cardiovascular outcomes and reduced quality of life. Left ventricular hypertrophy (LVH) is strongly linked to increased mortality and cardiovascular disease, and depression may be one of the key factors contributing to hypertensive LVH. The authors consecutively enrolled 353 patients with uncomplicated hypertension between November 2017 and May 2021. All participants completed the Hamilton Depression Scale (HAM-D) to assess their depression status, with depression defined as a HAM-D score of 20 or higher. Linear regression analysis revealed a positive association between HAM-D and LVMI (adjusted β, 1.51, 95% CI, 1.19–1.83, p < .001). Logistic regression models showed that individuals with hypertension and depression had a higher risk of LVH than those with hypertension alone (adjusted OR, 2.51, 95% CI, 1.14–5.52, p = .022). The association between depression and LVH significantly interacted with age, sex, education levels, but not BMI and household income. Following age, sex, and education levels stratification, an independent association of depression and LVH was observed only in age <60 years (age <60 years: OR, 7.36, 95% CI, 2.25–24.13, p < .001), male (male: OR, 16.16, 95% CI, 3.80–68.73, p < .001), and higher education levels (high school and above: OR, 11.09, 95% CI, 2.91–42.22, p < .001). Our findings suggest that depression is a significant risk factor for LVH in hypertensive patients, particularly in those who are under 60 years of age, male, and have higher education levels.
1 INTRODUCTION
Echocardiographic assessment of left ventricular hypertrophy (LVH) has been linked to a significantly higher risk of cardiovascular morbidity and death.1, 2 With regard to the development from early hypertension to cardiovascular mortality, hypertensive LVH is a crucial early finding in individuals with essential arterial hypertension and has various pathophysiological consequences.3 Though the exact mechanism causing the elevated mortality risk linked to LVH patients is still being researched. The heterogeneity of LVH occurrence in hypertensive individuals has made LVH unpredictable. As a result, finding potential LVH risk factors is essential for reducing the burden of hypertension.
Depression is a prevalent affective illness. Previous research demonstrated a link between depression and cardiovascular diseases.4-7 There found a high incidence of depression among hypertension individuals.8, 9 Improving patients' psychological health may help in hypertension prevention and therapy.10 Hypertensive patients with depression have a worse cardiovascular prognosis and quality of life.11, 12 Considering the strong association between LVH and increased mortality and cardiovascular disease, we formulated the hypothesis that depression represents a significant mental factor contributing to the development of hypertensive LVH. In this study, we aimed to explore the potential association between depression and hypertensive LVH.
2 MATERIALS AND METHODS
2.1 Study subjects
This study was an observational study. From November 2017 to May 2021, 353 hypertension patients were consecutively enrolled at Shaanxi Provincial People's Hospital. The exclusion criteria were heart failure, coronary heart disease, atrial fibrillation, cardiomyopathy, diabetes, kidney disease, thyroid dysfunction, cancer, active infections, chronic immune-mediated disorders, or current use of immunosuppressive drugs, including corticosteroids. The research was authorized by the Ethics Committee of Shaanxi Provincial People's Hospital, and accomplished in accordance with the principles stated in the Helsinki Declaration. All participants in this study gave their informed permission.
The measurement of blood pressure (BP) was carried out with a mercury sphygmomanometer by experienced physicians. After 5 min of rest, two blood pressure readings were collected at least 30 s apart. Systolic blood pressure greater than 140 mmHg, diastolic blood pressure greater than 90 mmHg, or the use of anti-hypertensive medication within the past 2 weeks was considered hypertension.13, 14 Devereux's standard formula was used to determine left ventricular mass (LVM).15 LVH was defined as a left ventricular mass index (LVMI) of greater than 115 (males) or 95 (females) (g/m2), where LVMI is the ratio of LVM to the body surface area (BSA).16 BSA was calculated using the following formulae: BSA men = 0.0057×height (cm) + 0.0121×weight (kg) + 0.0882 and BSA women = 0.0073×height (cm) + 0.0127×weight (kg) − 0.2106.17
2.2 Clinical data collection
Every patient had a thorough cardiac examination, which comprised a 12-lead electrocardiogram, echocardiogram (EPIQ 7 C, Philips, Netherlands), complete medical history, age, sex, and body mass index (BMI). Experienced physicians were responsible for gathering the participants' baseline characteristics. The data were finally added to the database on the network (Likang Times Technology Co. Ltd, Beijing, China). The double-input method was used for data entry. When the values of the two entries were agreed, the data were uploaded into the database. In the absence of this, the system would automatically detect a mistake, which could then be fixed by reviewing the raw data. Different individuals entered identical data twice for the same sample.
2.3 Depression assessment
The Hamilton Depression Scale (HAM-D) assesses depression severity depending on symptoms experienced in the past week, and was administered to each individual enrolled in the study. The scale has 24 items ranging from 0 to 4. Based on HAM-D, the overall score ranges from 0 to 96. The criterion for depression was a HAM-D score of 20 or above. All persons' HAM-D results were gathered at the time of enrollment.
2.4 Blood sampling
After all participants had fasted overnight (more than 12 h) during enrolment, venous blood samples were taken from each. An automated analyzer (AU5800, Beckman Coulter, CA) and enzymatic procedures were used to test triglycerides, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, creatinine, and uric acid.
2.5 Statistical analysis
The Kolmogorov-Smirnov statistical test was used to check the normality of continuous variables. Continuous variables were calculated as means (standard deviation [SD]) or medians (interquartile ranges [IQRs]) and compared using Student's t-test (normal distribution) or the Mann-Whitney U test (non-normal distribution). Categorical variables were expressed as absolute values (percentages) and compared using the chi-square test. The correlation between HAM-D and LVMI was examined using Spearman's correlation test.
We conducted univariate and multivariate logistic regression analyses with the Hamilton Depression Rating Scale (HAM-D) as a continuous variable and categorical variable, respectively, to examine the correlation between HAM-D and LVH in hypertensive patients. We analyzed the association between HAM-D score and LVMI using univariate and multivariate linear regression models. In addition, we calculated variance inflation factors (VIF) to examine the multicollinearity among the independent variables in the multiple regression models. Model 1 was unadjusted. Model 2 was adjusted for age, sex, BMI, cigarette smoking, low income, high school and above. Model 3 was adjusted for age, sex, BMI, cigarette smoking, low income, high school and above, creatinine, uric acid, angiotensin converting enzyme inhibitor (ACEI)/angiotensin II receptor blocker (ARB), β blockers, diuretics, and calcium channel blockers. In addition, we conducted subgroup analyses stratified by age, sex, BMI, household income, and education levels. Household income includes the patients' and their spouses' self-reported annual income. Income below 50,000 Chinese Yuan Renminbi per year were considered low income.18 Interaction tests were conducted to determine if the correlation between depression (HAM-D score ≥ 20) and LVH varied by age (<60 years vs. ≥60 years), sex, BMI (<24 kg/m2 vs. ≥24 kg/m2), household income (low income or not), and education levels (high school and above or not). Statistics were considered significant for p-values < .05.
Statistical analysis was performed with PASS software to calculate the sample size (version 15.0.1). Sufficient sample size was utilized to detect an odds ratio of 1.5 with 85% power at a significance level of 0.05 and a two-sided test. Considering the frequency of LVH among hypertensive Chinese adults of 19.3%,19 the PASS software produced a sample size greater than 350 cases.
Statistical significance was defined as a p-value <.05. The PASW Statistics 26.0 application was used to examine the data (SPSS Inc., Chicago, IL). All statistical tests were two-sided.
3 RESULTS
3.1 Baseline characteristics
The ages of the participants ranged from 28 to 84, and men made up 50.1% of the total. HAM-D scores ranged from 0 to 38, while the overall study population's mean HAM-D score was 10.58 ± 7.17. The depression group showed higher heart rate (no-depression: 73.26 ± 10.25, depression: 78.10 ± 9.46 bpm, p = .005), higher systolic blood pressure (no- depression: 130.48 ± 16.69, depression: 143.78 ± 26.58 mmHg, p = .003), higher interventricular septum (no- depression: 10.03 ± 0.94, depression: 10.41 ± 1.29 mm, p = .047), higher LVMI (no- depression: 85.94 ± 23.84, depression: 112.79 ± 27.74 g/m2, p < .001). The depression group showed a greater proportion of education levels (high school and above, no- depression: 38.9%, depression: 56.4%, p = .035), ACEI/ARB use (no- depression: 29.9%, depression: 51.3%, p = .007), β blockers use (no- depression: 34.4%, depression: 53.8%, p = .017), and diuretics use (no- depression: 4.1%, depression: 12.8%, p = .020) (Table 1). In addition, we found that the number of antihypertensive drugs used in the group with HAM-D score ≥20 was significantly higher than that in the group without depression (HAM-D score < 20). Table S1 shows the baseline characteristics of the 353 hypertensive individuals based on LVH. Table S2 displays the baseline clinical characteristics of the study participants stratified by sex.
| Total | HAM-D score <20 | HAM-D score ≥20 | p value | |
|---|---|---|---|---|
| Participants, n | 353 | 314 | 39 | |
| Age, year | 59.29 ± 9.87 | 59.15 ± 9.60 | 60.46 ± 11.95 | .461 |
| Male, n % | 177 (50.1) | 158 (50.3) | 19 (48.7) | .850 |
| BMI, kg/m2 | 24.47 ± 3.11 | 24.36 ± 3.08 | 25.40 ± 3.26 | .094 |
| BSA, m2 | 1.84 ± 0.18 | 1.83 ± 0.17 | 1.88 ± 0.23 | .265 |
| Heart rate, bpm | 73.80 ± 10.27 | 73.26 ± 10.25 | 78.10 ± 9.46 | .005 |
| SBP, mmHg | 131.95 ± 18.48 | 130.48 ± 16.69 | 143.78 ± 26.58 | .003 |
| DBP, mmHg | 79.65 ± 11.59 | 79.20 ± 10.90 | 83.29 ± 15.87 | .211 |
| Cigarette smoking, n % | 95 (26.9) | 84 (26.8) | 11 (28.2) | .847 |
| Low income, n % | 188 (53.3) | 169 (53.8) | 19 (48.7) | .547 |
| High school and above, n % | 144 (40.8) | 122 (38.9) | 22 (56.4) | .035 |
| Uric acid, umol/L | 310.52 (253.26, 363.07) | 308.59 (252.89, 361.99) | 312.98 (265.00, 378.84) | .351 |
| Creatinine, mmol/L | 65.38 (54.40, 76.00) | 66.00 (54.02, 76.03) | 62.90 (55.20, 74.09) | .564 |
| TG, mmol/L | 1.69 ± 1.01 | 1.67 ± 0.98 | 1.85 ± 1.24 | .632 |
| TC, mmol/L | 4.16 ± 1.07 | 4.16 ± 1.06 | 4.15 ± 1.12 | .739 |
| HDL-C, mmol/L | 1.15±0.28 | 1.14±0.28 | 1.16±0.30 | 0.901 |
| LDL-C, mmol/L | 2.33±0.81 | 2.33±0.80 | 2.36±0.89 | 0.686 |
| IVS, mm | 10.07±0.99 | 10.03±0.94 | 10.41±1.29 | 0.047 |
| LVPW, mm | 9.89±0.89 | 9.87±0.84 | 10.03±1.18 | 0.595 |
| LVEDD, mm | 46.20±4.97 | 46.45±4.69 | 44.13±6.51 | 0.234 |
| LVEF, % | 62.92±3.80 | 63.00±3.80 | 62.23±3.76 | 0.327 |
| Prior medication, n (%) | ||||
| ACEI/ARB | 114(32.3) | 94(29.9) | 20(51.3) | 0.007 |
| CCB | 99(28.0) | 83(26.4) | 16(41.0) | 0.056 |
| β blockers | 129(36.5) | 108(34.4) | 21(53.8) | 0.017 |
| Diuretics | 18(5.1) | 13(4.1) | 5(12.8) | 0.020 |
| Number of antihypertensive drugs, n (%) | 0.003 | |||
| Untreated | 134 (38.0) | 125 (39.8) | 9 (23.1) | |
| Monotherapy | 109 (30.9) | 101 (32.2) | 8 (20.5) | |
| Two drugs combination | 84 (23.8) | 69 (22.0) | 15 (38.5) | |
| Three drugs combination | 21 (5.9) | 17 (5.4) | 4 (10.3) | |
| Four drugs combination | 5 (1.4) | 2 (0.6) | 3 (7.7) | |
| LVMI, g/m2 | 88.90±25.68 | 85.94±23.84 | 112.79±27.74 | <0.001 |
- Continuous variables were calculated as means (standard deviation [SD]) or medians (interquartile ranges [IQRs]); categorical variables are presented as numbers (percentages).
- Abbreviations: BMI, body mass index; BSA, body surface area; DBP, diastolic blood pressure; HAM-D Hamilton depression scale; HDL-C, high-density lipoprotein cholesterol; IVS, interventricular septum; LAD, left atrial diameter; LDL-C, low-density lipoprotein cholesterol; LVEDD, left ventricular end-diastolic diameter; LVEF, left ventricular ejection fraction; LVH, left ventricular hypertrophy; LVMI, left ventricular mass index; LVPW, left ventricular posterior wall; SBP, systolic blood pressure; TC, total cholesterol; TG, triglyceride; ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin II receptor blocker.
3.2 Association of hamilton depression scale with left ventricular mass index
Hypertension with depression had a markedly higher LVMI than those without depression (Figure 1A). It was also found that the HAM-D score correlates positively with LVMI (r = 0.517, p < .001) (Figure 1B).
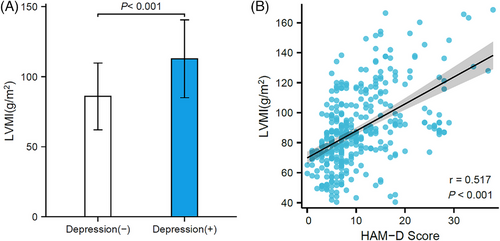
A linear regression analysis revealed an association between HAM-D score and LVMI (β, 1.80, 95% CI, 1.47–2.12, p < .001). HAM-D score also showed a positive correlation with LVMI after adjusting for variables according to Model 2 (β, 1.82, 95% CI, 1.50-2.14, p < .001). When the variables were adjusted for Model 3, the results were the same as in Model 3 (β, 1.51, 95% CI, 1.19-1.83, p < .001). Linear regression models utilizing HAM-D score as a categorical variable (HAM-D score ≥20) showed that hypertensive patients with depression correlated positively with LVMI (Model 1: β, 26.86, 95% CI, 18.74-34.97, p < .001; Model 2: β, 27.52, 95% CI, 19.43-35.62, p < .001; Model 3: β, 20.51, 95% CI, 12.79-28.23, p < .001) (Table 2).
| Unstandardized coefficient | Standardized coefficient | |||||
|---|---|---|---|---|---|---|
| B (95% CI) | Std. error | β | t | p value | R2 | |
| Each additional 1 score of HAM-D | ||||||
| Model 1a | 1.80 (1.47–2.12) | 0.17 | .50 | 10.88 | <.001 | 0.25 |
| Model 2b | 1.82 (1.50–2.14) | 0.16 | .51 | 11.10 | <.001 | 0.29 |
| Model 3c | 1.51 (1.19–1.83) | 0.16 | .42 | 9.34 | <.001 | 0.41 |
| HAM-D score ≥20d | ||||||
| Model 1a | 26.86 (18.74–34.97) | 4.13 | .33 | 6.51 | <.001 | 0.11 |
| Model 2b | 27.52 (19.43–35.62) | 4.12 | .34 | 3.04 | <.001 | 0.15 |
| Model 3c | 20.51 (12.79–28.23) | 3.93 | .25 | 5.22 | <.001 | 0.31 |
- Abbreviations: ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin II receptor blocker; CI, confidence interval; HAM-D, Hamilton depression scale; LVMI, left ventricular mass index.
- a Model 1: unadjusted.
- b Model 2: adjusted for age, sex, body mass index, cigarette smoking, low income, high school and above.
- c Model 3: adjusted for age, sex, body mass index, cigarette smoking, low income, high school and above, creatinine, uric acid, ACEI/ARB, β blockers, diuretics, calcium channel blockers, diastolic blood pressure, and systolic blood pressure.
- d Compared with HAM-D score < 20.
3.3 Association of depression with left ventricular hypertrophy
Univariate analysis with HAM-D as a continuous variable revealed a 10% increase in LVH risk for every 1-point rise in HAM-D (OR, 1.10, 95% CI, 1.06-1.13, p < .001). In a multivariate study, increased depression (by one point) was found to be independently and significantly related to LVH (Model 2: OR, 1.10, 95% CI, 1.06-1.13, p < .001; Model 3: OR, 1.08, 95% CI, 1.04-1.13, p < .001) (Table 3).
| Each additional 1 score of HAM-D | HAM-D score ≥20d | |||
|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | |
| Model 1a | 1.10 (1.06–1.13) | <.001 | 3.10 (1.56–6.15) | .001 |
| Model 2b | 1.10 (1.06–1.13) | <.001 | 3.14 (1.56–6.32) | .001 |
| Model 3c | 1.08 (1.04–1.13) | <.001 | 2.51 (1.14–5.52) | .022 |
- Abbreviations: ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin II receptor blocker; CI, confidence interval; HAM-D, Hamilton depression scale; LVH, left ventricular hypertrophy; OR, odds ratio.
- a Model 1: unadjusted.
- b Model 2: adjusted for age, sex, body mass index, cigarette smoking, low income, high school and above.
- c Model 3: adjusted for age, sex, body mass index, cigarette smoking, low income, high school and above, creatinine, uric acid, ACEI/ARB, β blockers, diuretics, calcium channel blockers, diastolic blood pressure, and systolic blood pressure.
- d Compared with HAM-D score <20.
Hypertension with depression showed a greater likelihood of LVH when considered as a categorical variable than those with hypertension alone (OR, 3.10, 95% CI, 1.56-6.15, p = .001). Compared to hypertensive individuals without depression, individuals with hypertension and depression had an odds ratio for LVH of 3.14 (Model 2: OR, 3.14, 95% CI, 1.56-6.32, p = .001) and 2.62 (Model 3: OR, 2.51, 95% CI, 1.14-5.52, p = .022) (Table 3).
3.4 Subgroup analysis of the association between depression and left ventricular hypertrophy
The relationship between depression and LVH interacted substantially with age (<60 years vs. ≥60 years) (Interaction p = .002), sex (Interaction p = .012), education levels (high school and above or not) (Interaction p = .018), but not with BMI (<24 kg/m2 vs. ≥24 kg/m2) (Interaction p = .173) and household income (low income or not) (Interaction p = .234). We conducted stratified analyses by age, sex, and education levels.
3.5 Stratified analyses by age
Compare with hypertensive individuals <60 years and ≥60 years without depression, LVMI were higher both in hypertensive individuals <60 years (no- depression: 84.95 ± 23.99, depression: 124.62 ± 29.96 g/m2, p < .001) and ≥60 years (no-depression: 86.95 ± 23.72, depression: 100.34 ± 18.93 g/m2, p = .003) with depression. However, LVMI was elevated more significantly in hypertensive patients <60 years with depression than in hypertensive patients ≥60 years with depression (Figure 2A). Patients younger than 60 years with hypertension (r = 0.584, p < .001) (Figure 2B) have a stronger HAM-D score-LVMI connection than those older than 60 years (r = 0.449, p < .001) (Figure 2C). There was an interaction between age and depression with regard to LVH risk (Model 1: Interaction p = .002; Model 2: Interaction p = .002; Model 3: Interaction p = .014). Depressed hypertensive individuals <60 years had a greater probability of developing LVH than their non-depressed according to the logistic regression models (Model 1: OR, 7.37, 95% CI, 2.72-19.98, p < .001; Model 2: OR, 8.68, 95% CI, 3.00-25.14, p < .001; Model 3: OR, 7.36, 95% CI, 2.25-24.13, p < .001). In contrast, among hypertensive patients ≥60 years, there was no association between depression and LVH (Model 1: OR, 1.18, 95% CI, 0.40-3.50, p = .765; Model 2: OR, 1.10, 95% CI, 0.36-3.33, p = .871; Model 3: OR, 1.14, 95% CI, 0.34-3.83, p = .838) (Figure 3 and Table S3).
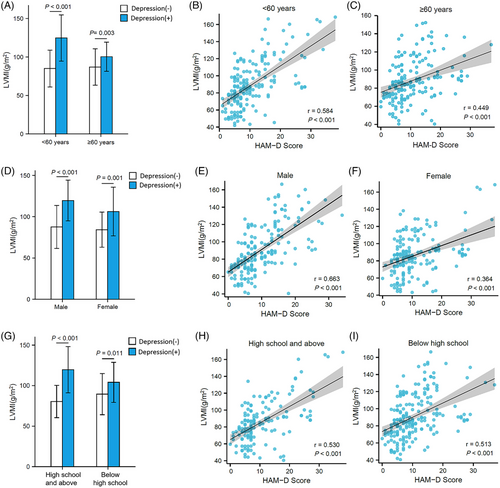
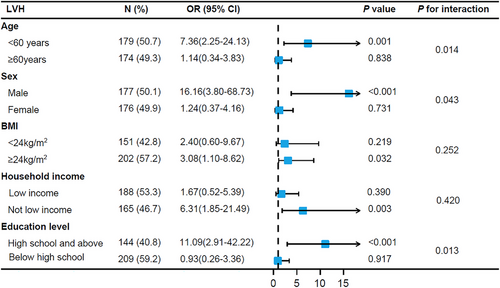
3.6 Stratified analyses by sex
After stratification by sex, LVMI were higher both in men with depression (no-depression: 87.59 ± 26.06, depression: 119.62 ± 24.61 g/m2, p < .001) and women with depression (no-depression: 84.26 ± 23.31, depression: 106.31 ± 29.58 g/m2, p = .001). However, men with depression experienced a greater increase in LVMI than women with depression (Figure 2D). Males (r = 0.663, p < .001) (Figure 2E) exhibit a stronger association between HAM-D score and LVMI than females (r = 0.364, p < .001) (Figure 2F) do. Regarding the likelihood of LVH, there was sex-by-depression interaction. (Model 1: Interaction p = .012; Model 2: Interaction p = .010; Model 3: Interaction p = .043). The logistic regression a nalysis showed that the depression was associated with LVH in men (Model 1: OR, 7.96, 95% CI, 2.88-22.02, p < .001; Model 2: OR, 18.75, 95% CI, 4.95-71.04, p < .001; Model 3: OR, 16.16, 95% CI, 3.80-68.73, p < .001) but not in women (Model 1: OR, 1.24, 95% CI, 0.45-3.45, p = .677; Model 2: OR, 1.16, 95% CI, 0.41-3.28, p = .778; Model 3: OR, 1.24, 95% CI, 0.37-4.16, p = .731) (Figure 3 and Table S3).
3.7 Stratified analyses by education levels
After stratification by education levels, LVMI was higher both in education levels of high school and above with depression (no-depression: 80.35 ± 23.99, depression: 119.56 ± 28.61 g/m2, p < .001) and below high school with depression (no-depression: 89.49 ± 25.43, depression: 104.03 ± 24.69 g/m2, p = .011) in hypertensive individuals. However, education levels of high school and above with depression experienced a greater increase in LVMI than those below high school with depression (Figure 2G). HAM-D score was significantly positively correlated with LVMI in education levels of high school and above (r = 0.530, p < .001) (Figure 2H) and in below high school (r = 0.513, p < .001) (Figure 2I). Regarding the likelihood of LVH, there was an education levels by depression interaction (Model 1: Interaction p = .018; Model 2: Interaction p = .014; Model 3: Interaction p = .013). The logistic regression analysis showed that the depression was associated with LVH in education levels of high school and above (Model 1: OR, 7.37, 95% CI, 2.78-19.55, p < .001; Model 2: OR, 9.55, 95% CI, 3.00-30.40, p < .001; Model 3: OR, 11.09, 95% CI, 2.91-42.22, p < .001) but not in education levels of below high school (Model 1: OR, 1.25, 95% CI, 0.42-3.73, p = .689; Model 2: OR, 1.27, 95% CI, 0.42-3.85, p = .675; Model 3: OR, 0.93, 95% CI, 0.26-3.36, p = .917) (Figure 3 and Table S3).
Figure 3, Figure S1, and Table S3 indicated the results of the association examination of depression for LVH in subgroups stratified by BMI and household income.
4 DISCUSSION
In this study, we revealed an association between depression and LVH in hypertensive patients. However, the relationship between depression and LVH interacted substantially with age, sex, and education levels, but not with BMI and household income. After stratification by age, sex, and education levels, only age <60 years, men, and higher education levels were found to have an independent correlation between depression and LVH.
Previous studies have established a connection between depression and hypertension.10, 20 There found a high proportion of depression among hypertension individuals.8 The relationship between depression and LVH was observed in a limited amount of prior research. These studies found that depression was related to LVH,21, 22 which was consistent with our findings. However, LVH was assessed by electrocardiogram rather than echocardiography in these studies. Meanwhile, these studies did not perform interaction analyses. Our research discovered a possible link between depressive disorder and LVH in hypertensive patients. Both logistic and linear regression models were used to evaluate the relationships between depression and hypertensive LVH. The relationships between depression and LVH were investigated using HAM-D scores as continuous and categorical variables by several logistic and linear regression models (Models 1–3) to further evaluate the validity of our findings. To eliminate the effects of other disorders, we enrolled patients with uncomplicated hypertension and excluded patients with heart failure, coronary heart disease, atrial fibrillation, cardiomyopathy, diabetes, kidney disease, thyroid dysfunction, cancer, active infections, chronic immune-mediated disorders, or current use of immunosuppressive drugs including corticosteroids. The findings of the study indicated that depression was an independent risk factor for LVH in hypertensive patients.
In depressive disorder, a crucial pathological finding is hypothalamic-pituitary-adrenal (HPA) axis dysfunction.23-25 They exhibit elevated levels of circulating catecholamines.24, 26 Chronic stimulation of negative psychosocial factors can activate the sympathetic nervous system and the HPA axis, and this could increase cardiovascular load, risk of LVH, and life-threatening dysrhythmias.27, 28 HPA hyperactivity may be a consequence of the depressive disorder and contribute to secondary pathology such as LVH.
In addition, we conducted subgroup analyses stratified by age, sex, education levels, BMI, and household income. The associations between depression and hypertensive LVH showed interactions with age, sex, and education levels, but not BMI and household income, according to interaction analyses. As a result, we performed age, sex, and education level-specific subgroup analyses. According to the findings of our study, males alone showed an association between depression and LVH, and females did not show this association, which was in accordance with the findings of prior research.29, 30 Our study also found that depressed patients younger than 60 years were more likely to develop LVH. Our research confirms the findings of Melanie and colleagues which showed depression among males and those under the age of 70 years increased the risk of death.30 A possible explanation for this difference is that depression in males and middle-aged people have higher biological stress responses and cardiovascular responses to a psychological stress protocol.31-33 Our results also showed that depression was associated with LVH in higher education levels in hypertensive patients. It is well-established that higher education levels are often associated with increased stress and pressure. Individuals pursuing higher education are frequently exposed to demanding academic workloads, competitive environments, and high expectations. This chronic stress can contribute to the development of depression. Depression, in turn, has been linked to alterations in the autonomic nervous system, including increased sympathetic activity and reduced parasympathetic tone, which can result in physiological changes such as increased heart rate and blood pressure.34 These changes, when sustained over time, can contribute to the development of LVH.35 The results of our study highlight the association between depression and LVH in age, sex, and education level-specific differences. These findings have significant implications for clinical practice and research. Recognizing the interactions between depression and demographic factors can help healthcare providers identify individuals at higher risk of developing LVH and tailor interventions accordingly. Moreover, understanding the specific subgroups in which the association is strongest can guide targeted prevention and treatment strategies. However, it is important to acknowledge the limitations of our study. The cross-sectional nature of the data prevents us from establishing causal relationships or determining the temporal sequence of events. Longitudinal studies are warranted to confirm our findings and explore the mechanisms underlying the observed associations.
Our study has a few limitations. Everyone who took part in the research was from the native Chinese population and came from a single center. Moreover, only a single HAM-D score was acquired at enrollment; further HAM-D evaluations were not obtained. Thirdly, this study's sample size was small. These variables affect the generalisability of our findings. Finally, we did not directly evaluate medication adherence, which is an important factor in hypertension management. While our results demonstrated a higher proportion of hypertensive patients using antihypertensive medications in the depressive group, we were unable to provide detailed information on the extent of medication adherence among our study participants. This limitation restricts our ability to fully understand the impact of medication adherence on the association between depression and hypertensive LVH. Future studies should aim to include comprehensive assessments of these confounders to confirm and extend our findings. In view of these limitations, it is imperative to interpret our findings cautiously, taking into account the specific context of our study design. Subsequent research endeavors should aim to address these limitations by incorporating larger and more diverse study populations, implementing assessments of depressive symptoms at multiple time points, and conducting comprehensive evaluations of medication adherence. These concerted efforts will serve to validate and expand upon our current findings, leading to a more comprehensive understanding of the intricate relationship between depression and hypertensive LVH. Moreover, an exploration of the underlying mechanisms and pathways through which depression influences hypertensive LVH holds the potential to enhance our comprehension of the complex interplay between mental health and cardiovascular well-being.
5 CONCLUSIONS
Our findings show that depression is associated with a higher incidence of LVH, especially in age <60 years, men, and higher education levels hypertensive patients. Differences in age, sex, and level of education in relation to depression emphasize the necessity of prevention and therapy in this population. Treatment in mental health to ameliorate depressive illnesses should focus on those patients. Despite the fact that a causal link between depression and LVH has still not been confirmed, our findings suggest the association between depression and LVH in age, sex, and education level-specific differences in patients with hypertension.
AUTHOR CONTRIBUTIONS
Shuang Shi conducted research, performed data analysis, wrote the paper; Gongchang Guan and Junkui Wang performed data collection; Rutai Hui assisted in editing of the manuscript; Yong Zhang provided statistical consultation; Qianwei Cui, Jingsha Zhao, and Ling Zhu designed and planned the study, revised the article. All authors reviewed and approved the manuscript.
ACKNOWLEDGMENTS
This work was supported by the Science and Technology Talents Support Program of Shaanxi Provincial People's Hospital (No. 2021BJ-10). Science and technology development incubation fund of Shaanxi Provincial People's Hospital (No. 2022YJY-06).
Open Research
DATA AVAILABILITY STATEMENT
The data were able to be obtained through reasonable request on the corresponding author.