Visit-to-visit variability in blood pressure and Alzheimer's disease
Abstract
Alzheimer's disease is the most common type of dementia and one of the leading sources of disability and dependency in the elderly. Given the limited treatment options, understanding the role of modifiable risk factors implied in the disease pathogenesis is a worthwhile endeavor to limit its global burden. Recently, the variability of blood pressure has been suggested to be a significant determinant of brain alterations and a potential therapeutic target. The aim of this article is to review the clinical evidence on the association between visit-to-visit blood pressure variability and Alzheimer's disease, highlight the underlying mechanisms, and suggest future implications.
1 INTRODUCTION
Cognitive impairment represents a worldwide concern in terms of public health and social care. It has striking physical, psychological, social, and economic consequences to patients, caregivers, and the healthcare system, and has an exponentially rising disease burden as a result of the aging population. Worldwide, around 50 million people currently have dementia, and the number is continuously expanding, with nearly 10 million new cases every year.1
Alzheimer's disease (AD) represents the most common type of dementia, accounting for 60% to 70% of all cases, and is a leading source of disability and dependency among older people.2 To date, no effective treatment exists to stop or reverse the course of AD. Hence, the identification of potentially modifiable determinants of the disease pathogenesis would help to develop measures aimed to prevent and delay the onset and progression of cognitive deterioration.
The “visit-to-visit” blood pressure (BP) variability (BPV), ie, the fluctuation of BP levels over months and years, represents neither a background noise nor a random effect phenomenon that dilutes the prognostic value of BP measurements. Instead, it has been associated with anatomical and functional alterations in the brain.3, 4
The aim of the current review was to summarize the evidence about the relationship between visit-to-visit BPV and AD, provide critical insights into the underlying pathophysiology, and suggest future implications. The most relevant clinical studies on this topic were identified through MEDLINE (accessed by PubMed) as of January 2018 (update March, week 1), using the following search strategy: (blood pressure variability) AND (Alzheimer's disease OR dementia OR cognit*). The reference lists of retrieved articles were reviewed to search for additional reports of relevant data. Prospective longitudinal studies were selected if estimates of the visit-to-visit BPV were reported and participants were diagnosed with AD at baseline or follow-up.
2 VISIT-TO-VISIT BPV AND AD: THE EVIDENCE FROM CLINICAL STUDIES
A total of 285 records were identified by database searching, of which 280 were excluded as a result of irrelevance (reviews, comments, unrelated to topic, unavailable data on visit-to-visit BPV, or AD diagnosis). A total of five studies were included in the review. Their main characteristics and results are summarized in the Table.
| Study, year | Study population, age | Blood pressure measurements | Time between visits | Follow-up | Visit-to-visit BPV and cognitive outcome |
|---|---|---|---|---|---|
| Three-City Study,5 2014 | 6506 noninstitutionalized elderly individuals, >65 y | 3 times | 2 y | 8 y |
The higher the variability, the higher the risk of dementia. The risk of dementia for patients in the highest decile of the CV of systolic BP was 1.77 (1.17–2.69) compared with those in the lowest decile. In the fully adjusted Cox model, increased variability of systolic BP was associated with an increased risk of AD (HR for 1 SD, 1.13; 95% CI, 1.00–1.28). |
| preDIVA trial,6 2018 | 2305 community-dwelling older individuals, 70–78 y | 4 times | 2 y | 6 y |
High BPV was associated with stronger decline in MMSE. A higher CV of systolic BP was not associated with AD (HR for 1-point increase in CV, 1.00 (95% CI, 0.96–1.06). In a subgroup of the study population without history of CVD, there was a trend toward a positive association between higher variability and incident dementia. |
| Lattanzi et al,7 2014 | 70 patients with AD, 140 cognitively normal controls matched for age and sex (AD: 79.10 y [±8.76 y]; control: 79.98 y [±7.19 y]) | 7 times | 30 d | 6 mo | Patients with AD had greater SD and CV of BP compared with controls. In the multiple logistic regression analysis after the adjustment for confounding variables, all the indices related to BPV were significantly associated with AD status. Systolic BP: OR for 1 SD, 1.752 (95% CI, 1.477–2.077); OR for 1-point increase in CV, 2.133; (95% CI, 1.701–2.674). Diastolic BP: OR for 1 SD, 1.313 (95% CI, 1.177–1.465); OR for 1-point increase in CV, 1.206 (95% CI, 1.115–1.305). |
| Lattanzi et al,8 2014 | 240 patients with AD, 76 y (±7.43) y | 5 times | 3 mo | 1 y |
Systolic BPV explained the decrease in MMSE score (adjusted R2 = 0.513) at multiple linear regression after adjustment for confounding variables. An annual rate reduction in MMSE by about 0.4 points for the unitary percentage increase in systolic BPV. Systolic BPV was an independent predictor of greater cognitive deterioration (MMSE score decline ≥4 points): OR, for 1-point increase in CV, 2.882 (95% CI, 1.772–4.495). The ROC analysis for evaluating the ability of systolic BPV to predict a faster cognitive decline showed an AUC of 0.913 (95% CI, 0.874–0.953); the cutoff point of ≥7.68 yielded a sensitivity of 97.3% and a specificity of 79.4%. |
| Lattanzi et al,9 2015 | 248 patients with AD, 76.02 y (±7.39 y) | 5 times | 3 mo | 1 y |
The change in the MMSE score at 1 year was associated with systolic BPV according to multiple linear regression (adjusted R2 = 0.567) score after adjustment for confounding variables. The median reduction in MMSE scores was 2.7 points. At multivariate logistic regression model, systolic BPV predicted an above average cognitive decline (adjusted OR for 1-point increase in CV, 2.634 [95% CI, 2.028–3.420]). The ROC analysis for evaluating the ability of systolic BPV to predict a faster cognitive impairment showed an AUC of 0.954 (95% CI, 0.928–0.980). |
- AD, Alzheimer's disease; AUC, area under the curve; BP, blood pressure; BPV, blood pressure variability; CI, confidence interval; CV, coefficient of variation; CVD, cardiovascular disease; HR, hazard ratio; MMSE, Mini-Mental State Examination; OR, odds ratio; preDIVA, Prevention of Dementia by Intensive Vascular Care; ROC, receiver operating characteristic; SD, standard deviation.
The Three-City Study was a cohort study conducted in three French cities (Bordeaux, Dijon, and Montpellier) to estimate the risk of cognitive impairment attributable to vascular factors. Among a total of 6506 noninstitutionalized individuals with a mean age of 73.7 years (±5.2 years), 206 participants developed AD over the 8-year follow-up period.5 There was no significant association between the average BP level and dementia risk. Conversely, increased visit-to-visit BPV was significantly associated with the likelihood of developing AD, after the adjustment for potential confounders including sex, education, antihypertensive drug use, history of vascular event, atrial fibrillation, and heart failure. Every increase of 1 standard deviation (SD) in the coefficient of variation (CV) of either systolic or diastolic BP was associated with approximately a 10% raised risk of AD. Results were unchanged when dementia cases diagnosed at the 2-year follow-up examination were excluded.
The preDIVA (Prevention of Dementia by Intensive Vascular Care) trial was a multicenter, open-label, cluster-randomized, controlled study that evaluated the effect of intensive vascular care on incident dementia in a population of community-dwelling older people aged 70 to 78 years in the Netherlands. A total of 2305 individuals, with a mean age of 74.2 years (±2.5 years), attended three or more visits and were considered for the post hoc analysis exploring the effects of BPV.6 After an average follow-up of 6.4 years, 82 participants were diagnosed with AD. Higher visit-to-visit BPV was associated with stronger decline of cognitive functions assessed through the Mini-Mental State Examination (MMSE). A higher CV of systolic BP did not predict an increased risk of AD in the overall population, while a trend toward a positive association was found in a subgroup of individuals without a history of cardiovascular disease. Compared with the Three-City Study, the preDIVA trial was characterized by a smaller sample size, a study population with higher age and cardiovascular risk at baseline, a shorter follow-up, and a lower incidence of dementia, possibly attributable to a less sensitive assessment procedure using a pragmatic and clinical approach as opposed to a neuropsychological test battery.6
The variability of BP was investigated in a cohort of 70 patients with mild to moderate AD aged 79.1 years (±8.7 years) and 140 healthy controls matched for age and sex.7 All participants were followed up for 6 months and individual BP profile was characterized through monthly evaluations. Compared with controls, patients with AD had higher maximum and lower minimum values and greater SD and CV of both systolic and diastolic BP. In the multiple logistic regression analysis, adjusted for demographic characteristics, baseline cognitive performance, vascular risk factors, and medical treatments, all visit-to-visit systolic and diastolic BPV indices were significantly associated with AD status.
The effect of visit-to-visit BPV on the rate of cognitive decline in AD was also explored. A total of 241 patients with AD with a mean age of 76.0 years (±7.4 years) were evaluated during a 12-month follow-up period at a tertiary research center.8 Only patients without a history of cardiovascular disease, cortical and subcortical brain lesions, atherosclerosis of neck and cranial arteries, and embolyzing cardiopathy were included. Visit-to-visit BPV was calculated through the CV estimated by serial BP recordings obtained at baseline and every 3 months up to the end of the follow-up. The progression of the cognitive impairment was assessed using the MMSE administered at entry and at the end of the study by trained neuropsychologists blinded to the BP evaluation. A strong relationship was found between fluctuations in BP levels and changes in cognitive performance: every unitary percentage increase in systolic BPV was associated with an annual worsening of 0.4 points on the MMSE score. During the 12-month period, nearly one third of the study cohort presented a decline of four or more points on the neuropsychological test, and visit-to-visit BPV was an independent predictor of faster cognitive deterioration, after controlling for age, education, apolipoprotein E genotype, dementia severity, and antihypertensive treatment. The CV of systolic BP allowed the reliable prediction of “fast progression” with a sensitivity of 97% and a specificity of 79%.
The role of BPV as a determinant of cognitive deterioration in AD was confirmed by a longitudinal prospective study, which involved 248 patients with a mean age of 76.0 years (±7.3 years) and no history of cardiovascular or cerebrovascular disease, who were followed up to 12 months.9 Five BP measurements for any patient were used to characterize the individual BP status, and visit-to-visit BPV was estimated through the CV. The cognitive course was investigated with the MMSE, performed at baseline and after 12 months. The median reduction in MMSE score at the end of the study was 2.7 points. Visit-to-visit systolic BPV could independently explain the decrease in MMSE score and was significantly associated with the risk of an above-average cognitive decline in the multivariate regression model. The receiver operating characteristic analysis for evaluating the ability of systolic BPV to predict faster cognitive impairment showed an area under the curve of 0.954 (95% confidence interval, 0.928–0.980).
3 VISIT-TO-VISIT BPV AND AD: THE PATHOPHYSIOLOGY
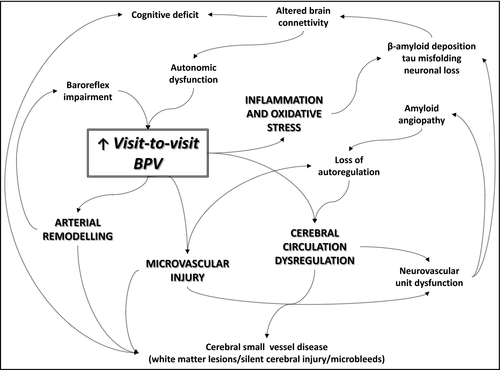
During the past decades, a large body of evidence has demonstrated that vascular and degenerative pathways critically interact and contribute to AD pathology,10 whose hallmarks include brain parenchymal and vascular deposits of amyloid-β peptide (Aβ), neurofibrillary tangles of hyperphosphorylated tau protein, gliosis, and neuronal loss.11 Recently, raised BPV has emerged as a novel risk factor for the development and progression of Alzheimer's dementia. From a pathophysiological perspective, several mechanisms can be advanced to explain these findings (1).
3.1 Hemodynamic instability
Hemodynamic instability is one of the main putative mechanisms that works by promoting both microvasculature injury and cerebral blood flow imbalance.
The shear stress on the vessel wall induced by exaggerated high systemic BP can lead to microvascular damage by promoting endothelial injury and disturbances in vascular smooth muscle functioning.12 The cerebral microcirculatory dysfunction can, in turn, influence the integrity of the blood-brain barrier (BBB) and result in neuronal injury and accelerated neuronal loss.13 The BBB is the largest exchange transport surface area in the brain and the major system to remove potentially neurotoxic molecules from the central nervous system. Dysfunctional BBB promotes Aβ accumulation and allows neurotoxic molecules to enter from circulation into the brain as a result of faulty clearance and altered permeability.14
Marked oscillations in arterial BP can have detrimental effects on cerebral blood flow and hemodynamics.15, 16 Cerebral matter is susceptible to fluctuations and inconsistent perfusion, and exaggerated low systemic BP levels can favor repeated episodes of tissue hypoxia-ischemia. Oligaemia can increase brain amyloidogenesis by enhancing expression and processing of Aβ precursor protein, activate microglia, impair neuronal protein synthesis, and cause neuronal damage and cellular death, particularly in the most vulnerable areas such as the hippocampi,3, 17 which are among the sites to be affected earlier and at a higher degree in AD. High visit-to-visit BPV can also determine ischemic changes in small vessels attributable to cerebral hypoperfusion during low-BP periods.18 Notably, the shift in the limits of cerebral autoregulation toward upper levels, which is common in elderly individuals or patients with long-lasting hypertension, makes cerebral blood flow highly dependent on systemic BP and amplifies the detrimental effects of its fluctuations.19
The dysfunction of cerebral microvasculature and the impairment of cerebral hemodynamics may be detrimental for the neurovascular unit. This is the system formed by neurons, astrocytes, and small vessels. It represents the delicate junction between flow and neural metabolism and is responsible for trophism, immune surveillance, and BBB exchanges.20 The failure of neurovascular coupling and the mismatch between metabolic requirements and blood supply can lead to neuronal energy crisis, hypometabolic, state and perturbed homeostasis, and, in turn, sustain the pathological processes associated with AD.21
3.2 Inflammation and oxidative stress
Inflammatory response and oxidative stress may be adjunctive mediators. The damage to endothelial cells and BBB induced by the BP fluctuations and perfusion imbalance can increase the secretion of proinflammatory cytokines and reactive oxygen species and induce microglia overactivation.22 The upregulation of the neuroinflammatory cascade and the reactive gliosis are key moderators of critical events involved in AD pathogenesis, such as misfolding and aggregation and propagation of Aβ and tau protein.23 Signally, high BPV has been associated with increased levels of biomarkers of inflammatory response and endothelial activation, such as interleukin 6, tumor necrosis factor-α, high-sensitivity C-reactive protein, and soluble E-selectin,24 and anti-inflammatory and antioxidant treatments could reduce end-target organ damage secondary to BP oscillations.25
3.3 Arterial stiffness and small vessel disease
Visit-to-visit BPV is an upstream determinant of artery remodeling, and high fluctuations of BP levels have been independently associated with arterial stiffness.26 Increased large artery stiffness provides direct harmful effects on structure and function of cerebral penetrating arteries.18, 27 BPV could cause a “tsunami effect” towards the cerebral parenchyma leading to cerebral small vessel diseases, including silent infarcts, white matter hyperintensities, and microbleeds,28 which contribute to reactive gliosis, synaptic and neuronal dysfunction, and disruption of brain structure and functional connectivity, either dependently or independently from the Aβ pathway.29
In addition, vessel wall changes can magnify BP fluctuations and augment BPV by reducing the arterial compliance and reflexes mediated by baroreceptors. Thus, higher visit-to-visit BPV correlated with increased carotid intima-media thickness and stiffness and synergic interaction in determining the cognitive dysfunction has been demonstrated between exaggerated BP fluctuations and advanced carotid artery remodeling.30
Cerebral arterial remodeling can also contribute to the disruption of vascular dynamics involved in perivascular flow and clearance of Aβ,31 and a relationship between arterial stiffness and cerebral Aβ deposition was found.32 Notably, amyloid angiopathy is commonly observed in pathology analysis of AD-affected brains, is associated with lobar distribution of cerebral microbleeds, and directly correlates to cerebrospinal levels of both Aβ and p-tau protein and the degree of cognitive decline of patients with AD.33
3.4 Autonomic dysfunction
The interplay between BPV, neurodegeneration, and autonomic abnormalities is an intriguing issue. The causes of disrupted visit-to-visit BPV are still debated: autonomic dyscontrol, arterial baroreflexes impairment, sympathovagal imbalance, and hypothalamo-pituitary-adrenal axis dysregulation caused by factors such as emotional and environmental stress or sleep disturbances are suggested to be underlying mechanisms.3
Notably, AD-related changes progress through the brain in a hierarchical sequence that starts in the mesiotemporal cortex and progressively invades the frontal, temporal, and parietal lobes. The early involvement by neurofibrillary tangles of the insular cortex, which is part of the cortical network implied in the central control of autonomic nervous system, may likely contribute to the impairment of cardioregulatory functions.18 Hence, BP instability may partly reflect and represent an epiphenomenon and a marker of AD pathology, even in subclinical stages. These points raise the possibility of a reverse causality between BPV and AD. Higher BPV could be an upstream risk factor of AD onset and progression, and the pathological process itself could amplify and mediate this relationship to some degree by enhancing BPV and its detrimental effects on the brain.
4 IMPLICATIONS FOR CLINICAL PRACTICE AND FUTURE RESEARCH
Alzheimer's dementia is a multifactorial disease, and as the knowledge of the underlying genesis and modifiable risk factors increases, so does the chance to develop effective strategies to reduce its global burden.
The notion that high BPV may contribute to AD pathology is intriguing and points out implications for clinical practice and future research. It would be advisable that clinicians and investigators pay attention to record the BP values of patients as accurately as possible to analyze fluctuations over time. A standardized assessment of the visit-to-visit BPV, however, is still lacking, and efforts should be directed to determine the most reliable index and appropriate schedule to obtain reproducible and valid estimates, define the ranges of normality, and identify the pathological thresholds according to age classes. Future research is also needed to explore the correlations between age, BPV, and cardiovascular disease. As suggested by the preDIVA trial, it is conceivable that in older people with a higher cardiovascular burden, cerebrovascular damage may already be too advanced to detect a significant influence of BPV on dementia incidence.6 Likewise the detrimental effects that result from long-standing hypertension and the association between midlife high absolute BP and late-life dementia, the relationship between high BPV in midlife or early late-life and cognitive impairment in late-life may be stronger.34
A postmortem study of 291 patients found substantially fewer neuritic plaques and neurofibrillary tangles in the medicated hypertensive than in the nonhypertensive groups, and suggested that antihypertensive agents may interfere with AD-associated neuropathology.35 Although clinical trials have shown conflicting results on the benefit of antihypertensive therapy towards the onset and progression of dementia, diuretics and calcium channel blockers, which are the most effective drug classes to minimize BP fluctuations,36-38 have been associated with reduced risk of AD in community-dwelling adults and patients with mild cognitive impairment.39, 40 Hence, the stability of BP levels could be a neglected interventional target to preserve cerebral functions and prevent or delay cognitive decline.
5 CONCLUSIONS
Prospective, interventional studies evaluating in parallel visit-to-visit BPV, cognitive performance, and structural and functional brain changes should be encouraged to provide more details on the pathophysiological links between BP fluctuations and the dementia process, explore whether reducing BPV can effectively impact the neurocognitive dysfunction, and evaluate whether heterogeneity in treatment effects can be explained by the different influence of antihypertensive regimens on BPV.
CONFLICT OF INTEREST
None.




