Cardioneuroablation can be an effective strategy to treat glossopharyngeal neuralgia-related sinus bradycardia and pauses
Nana Liu and Rohan Prasad are the first authors.
Disclosures: None.
Abstract
Introduction
Cardioneuroablation (CNA) has proven effectiveness in addressing hypervagotonia symptoms, such as neurocardiogenic syncope.
Methods and Results
In this case, we present the first-time application of CNA in a case of vago-glossopharyngeal neuralgia (VGPN). A 59-year-old female with near-syncope, sinus bradycardia, and sinus pauses triggered by recurrent right-sided neck pain was diagnosed with VGPN. The patient underwent successful treatment with carbamazepine and CNA. Subsequent follow-up revealed the sustained absence of sinus bradycardia or pauses, even upon neck pain resurgence after discontinuing carbamazepine.
Conclusion
In this patient, CNA successfully prevented pauses associated with VGPN, avoiding permanent pacemaker implantation.
1 INTRODUCTION
Glossopharyngeal neuralgia (GPN) is a rare painful facial syndrome characterized by sudden onset of sharp pain along the distribution of the glossopharyngeal nerve. In some cases, patients with GPN may experience cardiac presyncope or syncope, which is linked to hypervagotonia and manifests as sinus bradycardia, pauses, and/or hypotension. This particular syndrome is referred to as vago-glossopharyngeal neuralgia (VGPN). Historically, the standard treatment approach for hypervagotonia pauses with VGPN has been limited to the implantation of a permanent cardiac pacemaker (PM). In this case study, we utilized cardioneuroablation (CNA) to treat a patient with symptomatic sinus pauses triggered by neck spasms. Her condition was effectively managed through a combination of medical therapy and CNA.
2 CASE REPORT
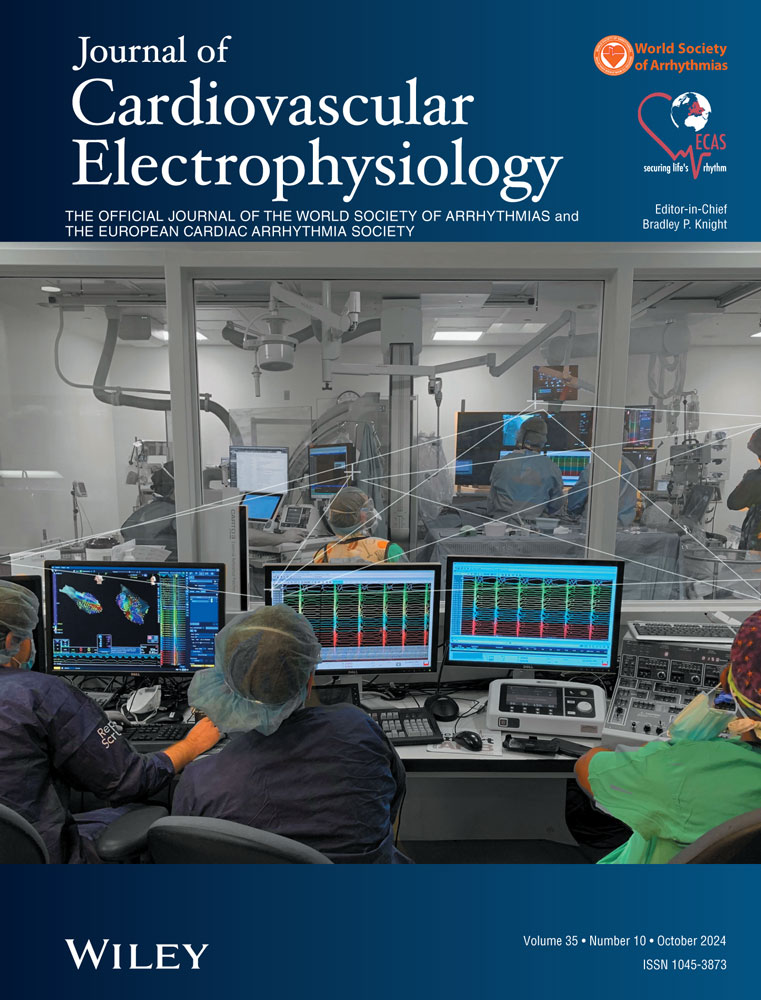
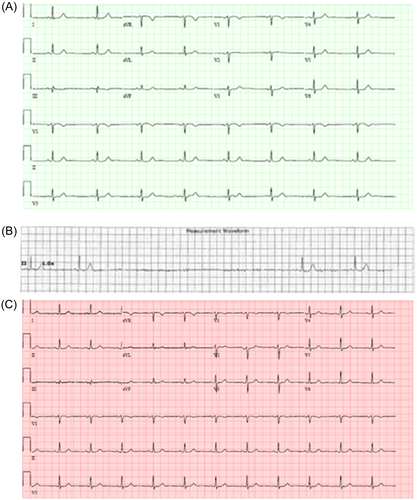
A 59-year-old female with a history of a right-sided middle cerebral artery cerebrovascular accident with encephalomalacia, distal right supra-clinoid ICA aneurysm, tobacco dependence, and chronic obstructive pulmonary disease presented with a 3-day history of right ear and throat pain. She was noted to have erythema and bulging of the right tympanic membrane and was treated for otitis media with amoxicillin, cetirizine, and fluticasone nasal spray. However, over the subsequent 3 weeks, she presented to the emergency department and was hospitalized for worsening episodes of sharp right neck, throat, and ear pain. Episodes were associated with sudden onset of sharp pain, nausea, vomiting, diaphoresis, tremors, right-sided weakness, and at times difficulty speaking and swallowing, dizziness, near syncope, and brief syncope. Physical examination, including neurological examination, was unremarkable. Otoscopic exam and flexible laryngoscopy were also normal. Electrocardiogram (ECG) revealed sinus bradycardia (Figure 1A) and telemetry showed sinus slowing with increased R-R intervals preceding sinus pauses (Figure 1B) up to 8 s associated with neck spasms, presyncope, nausea, dizziness, and diaphoresis. Echocardiography was unremarkable with a left ventricular ejection fraction of 60%. Computed tomography with angiography (CTA) of the brain, head, and neck showed no evidence of compressive mass. Magnetic resonance imaging (MRI) of the brain with CISS sequence revealed a tortuous dominant anterior inferior cerebellar artery vessel loop abutting cranial nerves IX–XI in the cerebellomedullary angle (Figure 2). The patient had relief of some symptoms with ondansetron, but not theophylline or meclizine. Her symptoms increased in frequency and severity, leading to transfer to Cleveland Clinic main campus for consideration of a permanent PM or CNA. After transfer, an emergent temporary transvenous PM lead was placed for continuing symptomatic sinus pauses. She was evaluated by neurology and otolaryngology and diagnosed with VGPN triggering vasovagal sinus bradycardia and sinus pauses. She was started on carbamazepine 100 mg twice daily with plans to titrate dosing.
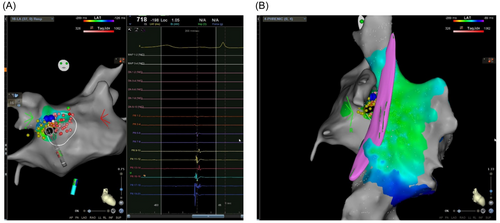
After a discussion of options, the patient elected to undergo CNA. Under general anesthesia with vascular access through femoral veins and transseptal access to the left atrium (LA), electroanatomical maps of the right atrium (RA) and LA were generated using a Biosense Webster CARTO mapping system. At baseline, carotid sinus stimulation via pacing of the right jugular vein reproducibly caused sinus arrest. The area of the right superior ganglion plexus (GP) was targeted by anatomical approach1; in that region, fragmented and multicomponent electrograms can also be recorded (Figure 3). The location of the phrenic nerve was assessed with pacing at high output before ablation around the right superior pulmonary vein (RSPV), and these areas were avoided during the ablation. Using a Biosense Webster CARTO SmartTouch SurroundFlow (STSF) irrigated RF ablation catheter with DF curve and contact force sensing, focal ablations at 30 W for 60 s were delivered to the right superior anterior ganglionic plexus from both the LA and RA. After CNA, repeated carotid sinus stimulation caused PR segment prolongation and sinus bradycardia but not sinus arrest. The endpoint of ablation was an increase in sinus rate by >25%–30% from baseline and abolition of vagal pauses with high-frequency extracardiac vagal stimulation with a multipolar catheter advanced within the right internal jugular vein at the level of the carotid sinus. Shortened PR intervals vs junctional beats were noted after the administration of atropine 2 mg. The P-P intervals remained constant. She tolerated the procedure well, and heart rates after ablation were 70–90 bpm (Figure 1C). The temporary PM was removed, and the patient was subsequently discharged home.
The patient returned to the emergency room a few days after discharge with difficulty swallowing and throat pain, but no bradycardia. She was noted to have stopped taking her carbamazepine due to rash and pruritus. Carbamazepine was transitioned to gabapentin with resolution of her difficulty swallowing, throat pain, rash, and pruritus. On follow-up with neurology 10 months later, the patient reported no recurrence of neck spasm, presyncope, throat pain, or bradycardia.
3 DISCUSSION
Often misdiagnosed as trigeminal neuralgia, GPN is a very rare facial pain syndrome with an incidence of 0.7 per 100 000 people.2 Patients usually present with unilateral sharp neck or throat pain, abrupt in onset, frequently triggered by swallowing, chewing, coughing, yawning, sneezing, or neck movements. Symptoms can resolve spontaneously. The pain attacks are mostly intermittent, leading to multiple ED visits thereby posing a diagnostic dilemma. When the pain radiates to the ear, it can mimic otitis externa or media, as seen in our patient, although the erythematous and bulging tympanic membrane suggests possible initiation of her symptoms by an episode of otitis media. Diagnosis is mainly clinical, as physical, otolaryngoscopic, and neurological examinations are usually unrevealing. Imaging, including CT, CTA, MRI, and MRA of the head and neck are usually performed to exclude other diagnoses, such as tumors and vascular compression. In the present case there was a high suspicion of a microvascular compression syndrome as a parsimonious explanation for the patient's unilateral facial pain and likely vagal nerve-mediated hemodynamic irregularities. A specialized MRI sequence with constructive interference in steady state (CISS) was acquired for visualization of the lower cranial nerves in this context. This provided valuable radiographic supporting evidence of the diagnosis which would not have been available with routine MRI imaging of the brain. The use of such sequences is common in the workup of unilateral lancinating facial pain syndromes and in the present case helped us to differentiate between more common disease conditions (e.g., trigeminal neuralgia which would have similar pain features but would not explain the hemodynamic symptoms) and VGPN.
Treatment can be pharmacological or surgical. Carbamazepine or oxcarbazepine are recommended as initial therapy.3, 4 Other medications, such as gabapentin or pregabalin can be considered for those who do not respond to or tolerate initial therapy. Our patient's symptoms improved on administration of a starting dose of carbamazepine and after the transition to gabapentin, she had no symptom recurrence after 4 months. For patients refractory to or not tolerant of at least two medications, neurosurgery, such as microvascular decompression, rhizotomy, and stereotactic radiosurgery, can be considered. The prognosis is variable, and most patients have a resolution of symptoms after medical management. Patients must be educated extensively about the condition and close symptom follow-up is required.
Hypervagotonia, such as bradycardia and pauses can occur in up to 10% of GPN patients, which can lead to presyncope, syncope, seizure, or even cardiac arrest.5 It is proposed that the close anatomical relationship between the glossopharyngeal and vagal nerves in the medulla oblongata and or possible vagoglossopharyngeal reflex arc cause the stimulation of the vagal nerve.6 Besides the medications mentioned before, permanent PM implantation has been reported in a few case reports to treat the hypervagotonia effects of VGPN.7-9 However, the treatment efficiency of pacing long-term is uncertain. A Japanese patient suffered recurrent syncope after PM implantation,8 while no pacing occurred in one patient during the first year.9
To our knowledge, this case is the first to report the application of CNA to treat sinus bradycardia and pauses for VGPN. Here CNA was applied via endocardial radiofrequency ablation targeting the GP clusters located epicardially between the RA and LA that primarily mediate parasympathetic activation. CNA has been applied to treat hypervagotonia, such as vasovagal syncope (VVS), sinus node dysfunction,1 and functional atrioventricular block10 since 2005. Observational studies for CNA in patients with VVS, or functional AV block report excellent medium and long-term results with syncope-free rates ranging from 73% to 100%.11-14 Besides the efficacy of CNA in controlling hypervagotonia symptoms, it also can avoid implantation of a PM and its associated complications. Notably, a recent randomized controlled trial of CNA versus optimal nonpharmacological treatment in 48 VVS patients reported that syncope occurred in only 8% of the CNA group compared to 54% in the control group with substantial improvement in the quality of life in CNA-treated patients.15 A study comparing the efficacy and safety of CNA in 61 patients and PM implantation in 101 patients with cardioinhibitory VVS reported 97% and 89%, respectively, remained syncope-free at 1-year follow-up. After adjusting for patient characteristics, the medium-term syncope recurrence risk and the safety profile of these two groups were similar.16 In our case, the patient reported significant improvement in quality of life with no recurrence of syncope, presyncope, dizziness, nausea, or diaphoresis. This indicates that medical therapy was effective in reducing the GPN-triggered episodes of pain and CNA was effective in preventing cardiac effects of hypervagotonia in this patient. Overall, it is important to initiate pharmacotherapy treatment once VGPN is diagnosed, and for certain patients who cannot tolerate medications or experience recurrent hypervagotonia symptoms, CNA can be considered as the next relatively safe and efficacious procedure of choice.
4 CONCLUSIONS
VGPN is a subset of GPN capable of causing symptomatic bradyarrhythmias. Besides pharmacological therapy, CNA can be an effective strategy for VGPN to treat hypervagotonia symptoms while avoiding implantation of a permanent PM.
ACKNOWLEDGMENTS
The authors would like to thank all the wonderful nurses and allied health staff who participated in the care of this patient.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.