Biophysical Modeling Predicts Ventricular Tachycardia Inducibility and Circuit Morphology: A Combined Clinical Validation and Computer Modeling Approach
Z. Chen, R. Cabrera-lozoya, and J. Relan contributed equally to the production of the manuscript.
This research received funding from the European Community's Seventh Framework Programme (FP7/2007-2013) under grant agreement n 224495 (EU-Heart project) and the ERC advanced Grant MedYMA 291080. The work was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre at Guy's and St. Thomas' NHS Foundation Trust and King's College London.
Z. Chen received an investigator-led research grant from Medtronic Ltd and Clinical Research Training Fellowship grant from the British Heart Foundation. Other authors: No disclosures.
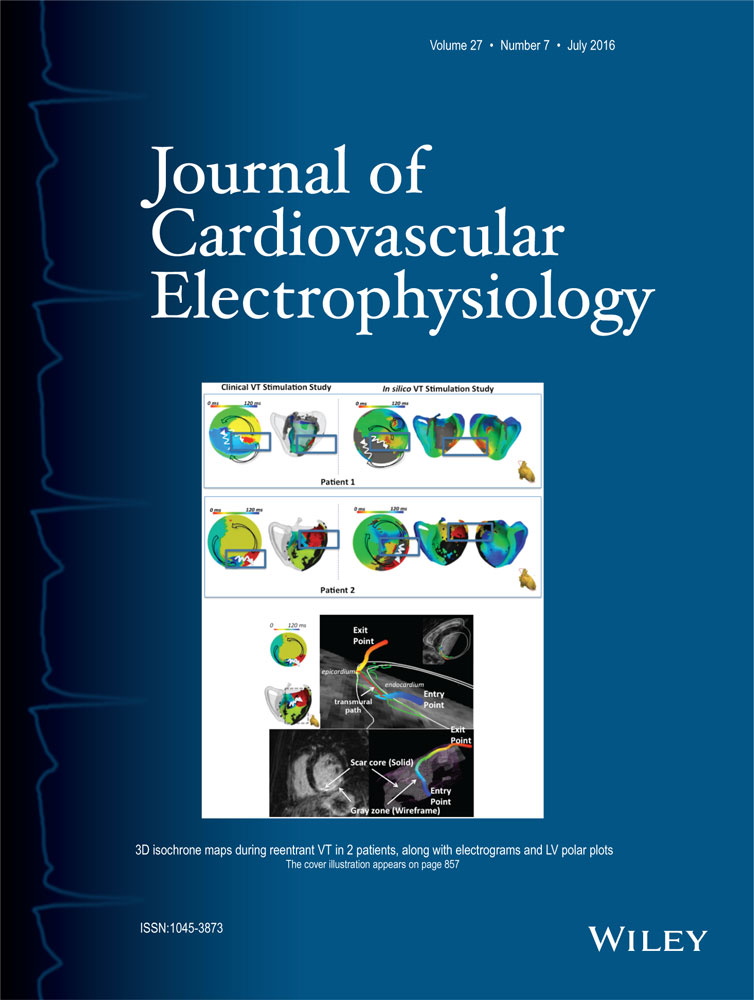
VT Stimulation In Silico
Introduction
Computational modeling of cardiac arrhythmogenesis and arrhythmia maintenance has made a significant contribution to the understanding of the underlying mechanisms of arrhythmia. We hypothesized that a cardiac model using personalized electro-anatomical parameters could define the underlying ventricular tachycardia (VT) substrate and predict reentrant VT circuits. We used a combined modeling and clinical approach in order to validate the concept.
Methods and results
Non-contact electroanatomic mapping studies were performed in 7 patients (5 ischemics, 2 non-ischemics). Three ischemic cardiomyopathy patients underwent a clinical VT stimulation study. Anatomical information was obtained from cardiac magnetic resonance imaging (CMR) including high-resolution scar imaging. A simplified biophysical mono-domain action potential model personalized with the patients’ anatomical and electrical information was used to perform in silico VT stimulation studies for comparison. The personalized in silico VT stimulations were able to predict VT inducibility as well as the macroscopic characteristics of the VT circuits in patients who had clinical VT stimulation studies. The patients with positive clinical VT stimulation studies had wider distribution of action potential duration restitution curve (APD-RC) slopes and APDs than the patient with a negative VT stimulation study. The exit points of reentrant VT circuits encompassed a higher percentage of the maximum APD-RC slope compared to the scar and non-scar areas, 32%, 4%, and 0.2%, respectively.
Conclusions
VT stimulation studies can be simulated in silico using a personalized biophysical cardiac model. Myocardial spatial heterogeneity of APD restitution properties and conductivity may help predict the location of crucial entry/exit points of reentrant VT circuits.