IMAGING DIAGNOSIS—TRAUMA-INDUCED TENSION PNEUMOCEPHALUS
Signalment
Two-year-old, 35-kg, intact male German Shepherd dog.
History and Physical Findings
The dog was hit by a car and had external head wounds but was neurologically normal. The head wound was superficial and was debrided. The debridment did not result in entry into the frontal sinus. However, an underlying comminuted right frontal bone fracture was detected and several small bone fragments were removed. Three weeks later, the dog developed what the owners perceived to be back pain. Within 2 days, the perceived pain progressed to inability to rise, leaning to the left, circling to the left, left-sided head tilt, and behavioral change. The dog was then referred for further evaluation. At this time, the dog had loss of menace response in the left eye, loss of corneal reflex in the left eye, head tilt to the left, tongue deviation to the left, positional nystagmus, and severe vestibular ataxia. The pupillary light responses and palpebral reflexes were normal. The proprioceptive reactions and myotatic reflexes were normal and no back pain was elicited. Clinical signs and neurologic examination suggested a multifocal CNS lesion. Because of the dog's clinical signs and history, the major considerations were meningoencephalitis, intracranial hemorrhage, and tension pneumocephalus.
The leukocyte count was elevated at 20,900 cells/μl. The leukogram was consistent with a glucocorticoid-induced leukocytosis with increased segmented neutrophils at 19,019 cells/μl, decreased lymphocytes at 627 cells/μl, and a normal band neutrophil count. There was increased blood glucose at 214 mg/dl, also consistent with a stress response. The coagulation profile was normal.
Imaging
Computed tomography (CT) images of the skull were acquired in transverse and dorsal planes.* There was a comminuted fracture of the right frontal bone with lateral and ventral displacement (Fig. 1). Gas and soft tissue attenuating material was present in the right frontal sinus. A fracture extended from the frontal sinus region into the right dorsal aspect of the cribriform plate. The soft tissue attenuating material in the right frontal sinus heterogeneously enhanced compared with the surrounding muscles, likely representing granulation or inflammatory tissue. There was no abnormal parenchymal brain enhancement. There was moderate gaseous distention of both lateral ventricles, most severe on the right, causing left-sided deviation of the falx cerebri and longitudinal fissure (Fig. 2). Gas extended into the subarachnoid space to the level of C2 (Fig. 3), likely through the lateral recesses. The diagnosis was pneumocephalus secondary to a comminuted fracture of the right frontal bone and cribriform plate. Based on the mass effect and progressive neuropathy, a tension pneumocephalus was diagnosed.
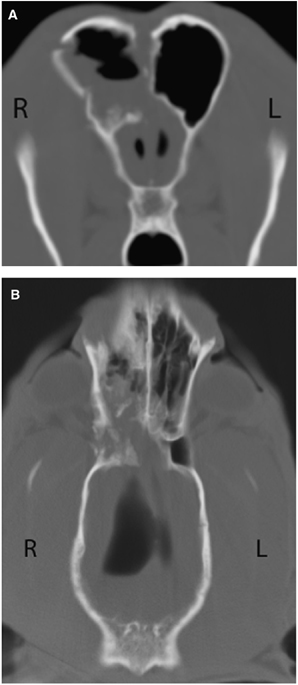
Five-millimeter transverse plane (A) and dorsal plane (B) images of the brain (window width: 2500, window level: 480). The image is at the level of the frontal sinuses, and a comminuted fracture of the right frontal bone with disruption of the cribriform plate can be seen. Mixed soft tissue and gas attenuating material is present in the right frontal sinus. Gas is present in the lateral ventricles and the cavity of the olfactory bulb.
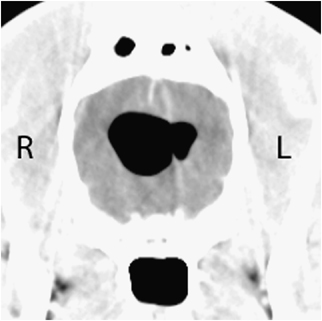
Five-millimeter transverse image of the brain (window width: 150, window level: 40). Note the asymmetric ventricular pneumocephalus, with the right lateral ventricle being larger than the left, and left-sided deviation of the falx cerebri and longitudinal fissure.
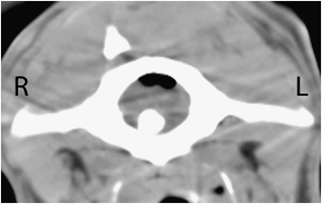
Five-millimeter transverse image at the level of the atlantoaxial junction (window width: 350, window level: 50). Note the air in the subarachnoid space.
Treatment
A transfrontal craniectomy was performed. The soft tissues were reflected and the fractured right frontal bone was identified. The frontal sinus was filled with bone fragments, debris, and tissue, all of which was debrided. The dissection was continued until a tear in the dura was found. The dural tear was repaired using a temporalis fascial graft. A needle was directed into the right ventricle and using gentle suction, 9 ml of air was removed. The skull was repaired using methyl methacrylate and the soft tissues were closed routinely. Cerebral spinal fluid (CSF), bone fragments found in contact with the dura mater, and a swab of the same area were submitted for culture and no growth was found. The dog's clinical signs improved immediately after surgery and resolved completely over the next 2 weeks.*
A CT examination was repeated 2.5 months later. There was no evidence of intracranial air but there was a persistent defect within the right dorsal aspect of the cribriform plate. The previously observed deviation of the falx and longitudinal fissure were no longer evident. There were no conclusive abnormalities of the olfactory portions of the brain. There was hyperattenuating material within the right frontal sinus consistent with bone cement, with evidence of remodeling and callus formation at the level of the frontal bone fractures.
Discussion
Pneumocephalus is asymptomatic intracranial air. In humans, pneumocephalus has resulted from craniotomy, craniectomy, cranial trauma, ventriculoperitoneal shunting, lumbar drain placement, and neoplasms arising from the frontal or paranasal sinuses that erode though the bone and dura matter.1–3 Pneumocephalus is estimated to occur in 0.5–1% of all human head injuries and does not require treatment.1 The presence of pneumocephalus after supratentorial surgery has been estimated to occur in 100% of patients; the amount of intracranial air will vary and usually reabsorbs within 2–3 weeks postsurgery.4 Tension pneumocephalus is symptomatic intracranial air. It is due to accumulation of air within the cranial cavity causing compression of the brain. As more air accumulates, the increased intracranial pressure will lead to clinical neuropathy. The transformation of pneumocephalus into tension pneumocephalus rarely occurs.2,4,5
Two main hypotheses have been proposed to explain the entrance of air into the cranial cavity.1,2 In both hypotheses, a defect in the dura mater and a fistula in the brain parenchyma must be present. One hypothesis is a ball-valve mechanism. Positive pressure is created extra-cranially, within the sinuses, with a cough or sneeze. This positive pressure forces air into the cranial cavity. It then moves through the dural defect and through the fistula in the brain parenchyma into the ventricular system. At the end of the cough or sneeze, the intracranial pressure is higher than the extracranial pressure. The air is unable to escape because the brain returns to its normal position, sealing the defect and trapping the air. In the second hypothesis, a CSF leak, also through a fistula and dural defect, creates negative pressure within the central nervous system. This negative intracranial pressure is equalized with the influx of air. With this hypothesis, CSF rhinorrhea can occur. This dog did not have aqueous nasal discharge. The owners reported that it was possible that he had been sneezing. Based on these historical findings, we suspect that the cause of this dog's tension pneumocephalus was the ball-valve mechanism.
Pneumocephalus can be classified according to its location as epidural, subdural, subarachnoid, intercerebral, or intraventricular.2 Intraventricular is the most common form of pneumocephalus.6 This patient had both intraventricular and subarachnoid pneumocephalus via communication through the dural defect. A discrete brain fistula was not identified on the CT images. A small brain fistula may have been present but may have not been resolved as the slice thickness was 5 mm. Additional modalities used in humans to localize small dural defects and/or fistulas include plain high-resolution CT (HRCT), HRCT cisternography, and MR cisternography.7,8
To our knowledge there are only three reports of tension ventricular pneumocephalus in the dog.6,9,10 In all of these, pneumocephalus was secondary to surgery, either rhinotomy or craniectomy. To our knowledge, there are no reports of tension pneumocephalus in the dog occurring secondary to trauma. Although this dog did undergo wound debridement just after his traumatic incident, this was only superficial debridement and the technique did not result in penetration of the frontal sinus.
In this dog, tension ventricular pneumocephalus was identified as causing several cranial nerve deficits and a behavioral change, with the cranial nerve deficits arising from the pons and medulla. Behavior change is attributed to a forebrain lesion. These multifocal brain lesions can be explained by the diffuse compressive lesion that was present. Clinical signs of tension pneumocephalus reported in animals include aqueous nasal discharge (CSF rhinorrhea), depressed mental status, ataxia, postural reaction deficits, absent menace response, tremoring, and aimless wandering.9,10
Treatment of pneumocephalus in humans depends on the cause, severity of clinical signs, and degree of tension. If tension pneumocephalus is suspected, it is considered to be a surgical emergency due to progressive increase in intracranial pressure leading to brain hypoxia, cerebral infarction, and potential for cerebral or brainstem herniation.2,5 Thus far, the treatment choice in dogs has been to repair the dural defect.6,9,10 Aspiration of air with temporary extra-ventricular drainage has been suggested but leads to management difficulties.9
Footnotes
ACKNOWLEDGMENTS
The authors wish to thank Dr. Federica Morandi for her critical review of the manuscript before submission.