Assessment of Intrathecal Pressure in Chondrodystrophic Dogs With Acute Thoracolumbar Disk Disease
Abstract
Objectives
To assess intrathecal pressure (ITP) in chondrodystrophic dogs with thoracolumbar disk extrusion.
Study design
Prospective cohort study.
Animals
Group 1: 11 chondrodystrophic dogs with thoracolumbar disk extrusion and present deep pain sensation. Group 2 (control): 3 healthy chondrodystrophic laboratory dogs without spinal disease.
Methods
Diagnosis was based on neurologic signs, magnetic resonance imaging (MRI) findings, and surgical confirmation. Blood pressure was maintained within physiologic range during anesthesia. A standardized surgical procedure was applied to minimize factors that could influence measurement readings. An extended hemilaminectomy was performed and ITP was measured with a fiber optic catheter. The catheter was inserted in the subarachnoid space 1 spinal segment caudal to the level of herniation and its tip was advanced to the site of compression.
Results
Significantly higher ITP occurred in chondrodystrophic dogs with acute thoracolumbar disk disease compared with controls. ITP was not associated with duration of clinical signs, neurologic status, outcome, degree of spinal cord compression, or signal intensity changes as assessed by MRI.
Conclusion
Acute thoracolumbar disk disease leads to elevated ITP in chondrodystrophic dogs, which may contribute to increased compression of spinal cord parenchyma.
Disk extrusion is the most common spinal neurologic disease in domestic dogs. In chondrodystrophic dogs, 3–6 years of age, thoracolumbar extrusions are overrepresented at intervertebral disk spaces T12–13 and T13–L1.1-3 Clinical signs range from focal back pain to paraplegia, with or without loss of deep pain perception. Variability in clinical signs may be explained by different pathophysiologic factors such as location, force, speed and rate of the herniation, degree and duration of compression, vascular changes, and inflammation.4
Alterations in spinal cord blood flow (SCBF) play an important role in spinal cord injury. Duration of compression-induced ischemia and intensity of blood flow recovery have an influence on the quality of neurologic recovery after spinal cord injury.5, 6 Therefore, maintaining adequate vascular perfusion,7 and decompressing the spinal cord8 are 2 important aspects of clinical management with acute spinal cord injury.9 In dogs, surgical decompression of the spinal cord, which improves arterial and venous hemodynamics, is usually achieved by means of hemilaminectomy through removal of extruded disk material. A significant increase in intraoperative SCBF was observed immediately after spinal cord decompression in dogs with acute thoracolumbar disk extrusion.6, 10 SCBF depends on spinal cord perfusion pressure (SCPP), which itself is defined as the difference between mean arterial pressure (MAP) and the cerebrospinal fluid (CSF) pressure in the intrathecal space (also referred to as the intrathecal pressure [ITP]).9, 11
This suggests that not only MAP but also ITP has a major influence on SCBF. A decrease in MAP or an increase in ITP has been shown to decrease SCPP, thus decreasing SCBF and resulting in ischemia or worsening of existing ischemia.9, 11
The importance of maintaining a stable, sufficiently high MAP in spinal cord injury (SCI) patients is well known. In people with SCI, an intraoperative MAP of 85–90 mmHg is sought, to maintain appropriate spinal cord perfusion.12, 13 Intraoperative CSF drainage is common practice in people undergoing thoracoabdominal aortic aneurysm surgery, as a means to increase SCBF through a decrease in ITP.9 This technique has been reported for prophylactic reduction of ischemic complications in the spinal cord.14-16 Various studies have demonstrated that ischemic damage to the spinal cord may cause lower extremity paralysis secondary to a reduction in SCPP.14, 16, 17 Recent publications now address the effects of lumbar CSF drainage in human spinal cord injury.9 In an experimental canine study, the effects of altering ITP on lumbar spinal cord blood flow was investigated in non-injured dogs18 and showed a relationship between SCBF and ITP. More specifically, an increase in ITP provoked a decrease in SCBF, and lowering ITP back to baseline levels led to an increase in SCBF, the latter however never returning to initial baseline values.18
The importance of ITP in spinal cord physiology and pathology prompted us to study ITP in the setting of naturally occurring disk herniation in chondrodystrophic dogs. We are unaware of similar studies. Our purposes were to assess ITP in dogs with intervertebral disk extrusion, and to compare the ITP in these dogs to ITP in chondrodystrophic dogs without spinal cord injury. We hypothesized that an increase in ITP would be observed at the site of injury.
MATERIAL AND METHODS
This study was approved by the institutional ethical authority.
Dogs
Chondrodystrophic dogs (n = 14) were enrolled in this prospective study. Group 1 (March 2011–April 2012) consisted of 11 chondrodystrophic dogs with acute deterioration of their neurologic status after intervertebral thoracolumbar disk extrusion. Inclusion criteria were 3 complete neurologic examinations (pre-surgical, 24 hours postsurgical, and at discharge) and magnetic resonance imaging (MRI) or computed tomographic (CT) examination confirming a single extradural compressive lesion. Dogs with a history of chronic clinical signs, with an incomplete neurologic examination, or with traumatic disk extrusion were excluded from the study.
Group 2 consisted of 3 mature healthy chondrodystrophic laboratory Beagles involved in another study independent from the present research. These dogs had no neurologic signs up to the time of surgery, therefore were considered free of spinal disease. Because of an absence of MRI at the test facility, no MR examination was performed. Laboratory dogs were euthanatized at the end of the study for reasons unrelated to the present study.
Clinical Evaluation
Recorded data included age, gender, breed, and duration of the preoperative neurologic signs. Preoperative neurologic signs were considered acute if they had occurred within 48 hours of admission and sub-acute if they occurred >48 hours with worsening of signs within 48 hours of admission. Based on severity, neurologic signs were graded as: grade 1 = only pain; grade 2 = ambulatory paraparesis; grade 3 = non-ambulatory paraparesis; grade 4 = paraplegia with deep pain present; and grade 5 = paraplegia with deep pain absent.19
Imaging
Dogs were anesthetized and positioned in dorsal recumbency for MRI (1 dog: 1.5 Tesla magnet, Phillips Interna 1.5 T, Phillips Medical Systems, PC Best, the Netherlands; 9 dogs: 1.0 Tesla magnet, Philips HFO Panorama, Phillips Medical Systems). The thoracolumbar region (Th10-L4) was examined based on neurologic examination findings. Imaging included a sagittal and transverse T2-weighted fast spin echo sequence (TR 2000–6000 ms, TE 100 ms, slice thickness 2.5–4 mm).
Level and lateralization of extruded disk material were evaluated. The degree of spinal cord compression and signal intensity changes of the spinal cord were assessed subjectively on sagittal and transverse T2-weighted images by an ECVDI board certified radiologist. Three grades of vertebral canal impingement were defined: grade 1-degree of impingement 30–39%; grade 2-degree of impingement between 40–49%; and grade 3-degree of impingement ≥50%. Signal intensity of the spinal cord in T2 weighted images was also subjectively compared to adjacent spinal cord, and the presence of hyperintensity was evaluated.
Because of technical problems, CT instead of MRI was performed in dog 2. The degree of spinal canal impingement and any signal intensity changes in this dog could not be evaluated.
Anesthesia
Dogs were premedicated with fentanyl (0.005 mg/kg intravenously [IV]) and general anesthesia induced with diazepam (0.2 mg/kg IV) and propofol titrated to effect and maintained with isoflurane in oxygen delivered using a rebreathing system. Crystalloid fluids were administered (10 mL kg−1 h−1 IV). Monitoring (ECG, SpO2, blood gas measurements, spirometry, oscillometric blood pressure at the metatarsal artery, and esophageal temperature) was continuous and recorded every 5 minutes. During surgery, constant rate infusion (CRI) fentanyl (5–10 μg/kg/h IV) was administered. If necessary, a bolus of ketamine (0.5 mg/kg IV) followed by 0.6 mg/kg/h CRI was added between the end of the measurements and the end of surgery to further improve intraoperative pain management. Cefazolin (20 mg/kg IV) was administered at the beginning of the surgery and repeated at the end of the surgical procedure.
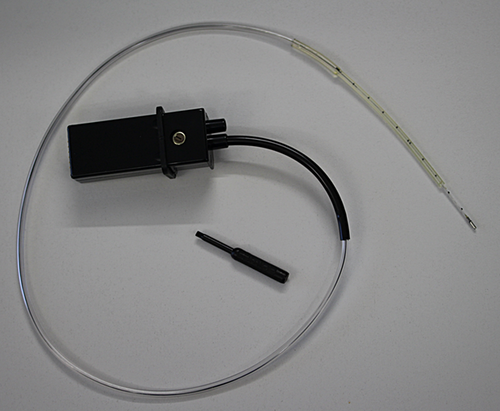
ITP Monitoring
ITP was measured using a SPM-1 device (Single-Parameter Monitor, Camino, LS Integra, Geneva, Switzerland) with a fiberoptic catheter (Camino ICP 110–4L, LS Integra, Geneva; Fig 1) This type of fiberoptic miniature-converter allows continuous, precise and artifact-free waveform registration, without need for recalibration between measurements once pre-catheterization initial zero point calibration has been performed. An intensity-modulating fiberoptic system within the catheter uses bellows as the primary transducer. Light from an LED source is transmitted down 1 fiber, called the sender. The polished surface of the bellows reflects light, which is then collected by another fiber, the receiver. Pressure shifts change the bellows’ position, modulating the intensity of the reflected light. As light is sensed by a light-sensitive device, it is amplified, filtered, and digitized. A 2nd pair of fibers with the same characteristics and length is mounted similarly within the catheter and exposed to the same light source. These fibers are connected by a reference junction. This scheme allows monitoring of LED intensity variations attributed to non-pressure events such as bending of the fiber or semiconductor temperature coefficients. The SPM-1 device automatically compensates for these changes by adjusting the intensity of the LED source, resulting in a stable and constant light intensity delivered to the surface of the bellows. The SPM-1 linearizes the catheter's response in real-time to optimize measurement accuracy. The SPM-1 provides a continuous numeric display of mean intrathecal pressure in the range of −10 mmHg to +125 mmHg.
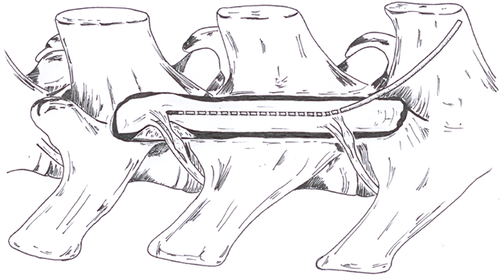
Measurement Methods
Surgery was performed by 1 neurosurgeon to exclude influences on measurements related to surgeon expertise. Dogs were positioned in slightly oblique sternal recumbency with the affected side up. A longitudinally extended hemilaminectomy was performed over 2 intervertebral spaces to expose the spinal cord. Extension of the standard hemilaminectomy was necessary to enable correct probe positioning while preventing an important CSF leak at the site of measurement, which would have influenced the recorded ITP value. The probe was calibrated to zero before insertion. Room temperature was kept constant at 19°C. One intervertebral space caudal to the affected disk, a 1 mm durotomy was performed, the probe inserted and pushed cranially within the subarachnoid space. The center of the compressive lesion detected preoperatively with MRI was determined intraoperatively by identification of the extruded disk material. The probe was positioned over the epicenter of the lesion and secured in place by the surgeon (Fig 2). The ITP value oscillated until stable placement of the catheter tip, and pressure was only recorded after stabilization of displayed value. Recording was stopped after reaching a stable pressure value. Extruded disk material was removed and the affected intervertebral disk space was fenestrated.
Finally, the surgical area was lavaged with lactated Ringer's solution at room temperature. No fat graft was placed over the bony window. The fascia and the subdermal fat tissue were apposed with 1.5 metric polydioxanone, the subcutaneous tissues with 1.5 metric polydioxanone, and the skin with 1.5 metric polypropylene.
In control dogs, an extended hemilaminectomy was performed from T13–L2, and ITP was measured over the intervertebral disk space T13–L1.
Postoperative Care
After surgery, the dogs’ neurologic status and signs of pain were assessed by physical examination. Postoperative analgesia was provided by administration of fentanyl (2.5–10 μg/kg/h IV) for 12 hours, then buprenorphine (0.015 mg/kg subcutaneously every 8 hours for 1–3 days) and carprofen (4 mg/kg orally once daily for 3 days).
During hospitalization, all dogs were rehabilitated in a standardized manner, consisting of massages and passive movements of limbs (stretching and bending) 3 times daily and underwater treadmill training for 10 minutes twice daily starting 2 days after surgery. Magnet field therapy was used twice daily starting the day after surgery. Long-term outcome was confirmed with either the owner or the referring veterinarian by telephone interview.
Statistical Analysis
All statistical analyses were performed using software (NCSS 2007 Statistical Software; www.ncss.com). ITP values from group 1 were normally distributed when evaluated with the Shapiro-Wilk test, but normality of the control group could not be established because of the small number of dogs. Differences between groups were therefore analyzed with the non-parametric Wilcoxon rank sum test. Each data point represented the median and 99% confidential intervals (99%CI). P-values <.05 were considered significant (*P < .05, **P < .01, ***P < .001).
RESULTS
Signalment and Preoperative Evaluation
Group 1 comprised 11 chondrodystrophic dogs (median age, 3.5 years [mean, 4.3 years; range: 2–9 years], median weight, 8.4 kg [mean, 7 kg; range, 4–12 kg]) with acute disk disease (3 males, 8 females). Breed distribution was: French Bulldog (n = 3), Pekingese (2), Dachshund (2), Miniature Dachshund (1), Cocker Spaniel (1), Coton de Tulear (1), and mongrel (1).
Preoperative neurologic signs were distributed as grade 2 (5 dogs), 3 (4), and 4 (2). Nine dogs were admitted with subacute clinical signs. Two dogs (6, 9) had surgery with ITP measurement within 48 hours of onset of first neurologic signs. Duration of spinal hyperesthesia as the only clinical sign before neurologic decline ranged from 2–10 days.
Group 2 included 2 male and 1 female Beagle and served as the control group. As part of another study these dogs were enrolled in, a daily physical examination was performed. All dogs were healthy without a history of neurologic deficits or spinal pain. Median age was 4 years (mean, 4.3 years; range, 4–5 years). Body weight ranged from 12–14 kg.
Imaging Findings
Group 1: Extrusion most commonly occurred between T13–L1 (5 dogs), other locations were T11–12 (1), T12–13 (2), L1–L2 (1), L2–3 (1), and L3–4 (1). The severity of vertebral canal impingement was classified as grade 1 (30–39% impingement of the vertebral canal) in 3 dogs, grade 2 (40–49% impingement) in 3 dogs, and grade 3 (≥50%) in 4 dogs. Signal hyperintensity of the spinal cord in T2 sequences was present in 5 dogs. In all dogs, a severe decrease or even disappearance of the CSF subarachnoid space was observed in T2 sequences at the site of compression.
Intraoperative Blood Pressure
MAP was kept between 70–115 mmHg in all but 2 dogs; dog 5 had MAP of 55–60 mmHg and dog 8 was 60–180 mmHg.
ITP
Group 1 median ITP (7 mmHg; 99%CI: 5, 8 mmHg) was significantly higher than group 2 (4 mmHg; 99%CI: 3, 4 mmHg; P < .001).
Clinical Outcome
No intraoperative complications occurred and post-surgical recovery was uneventful in all group 1 dogs. The neurologic grade 24 hours postoperatively was identical to the preoperative grade in 6 dogs; 2 dogs had improved by 1 grade, 2 dogs worsened by 1 grade, and 1 dog worsened by 2 grades. At time of discharge, the neurological grade was 2 (8 dogs) and 3 (3 dogs; Table 1). A follow-up telephone call with owners revealed that all dogs had recovered 8 weeks after surgery.
| MRI | Neurologic Grade | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dog | Group | Breed | Sex | Age (years) | Level | Lesion location | Grade of Stenosis | Signal- Hyperintensity | Duration of Signs | Initial | 24h | Discharge | Blood pressure (mmHg) | ITP | ||||
| 1 | 1 | Coton du Tulear | M | 7 | L2-L3, | left | 3 | yes | subacute | 3 | 3 | 2 | 70–115 | 7 | ||||
| 2 | 1 | Mongrel | SF | 4 | Th13-L1 | no MRI data | subacute | 2 | 4 | 3 | 70–115 | 7 | ||||||
| 3 | 1 | Pekingese | SF | 3 | Th11–12 | ventral | 1 | yes | subacute | 2 | 3 | 2 | 70–115 | 9 | ||||
| 4 | 1 | French bulldog | SF | 2 | L3-L4 | ventral | 1 | no | subacute | 2 | 2 | 2 | 70–115 | 8 | ||||
| 5 | 1 | French bulldog | F | 3 | Th13-L1 | right | 3 | no | subacute | 3 | 2 | 2 | 55–60 | 8 | ||||
| 6 | 1 | French bulldog | F | 3 | Th13-L1 | left, right | 2 | yes | acute | 4 | 3 | 3 | 70–115 | 7 | ||||
| 7 | 1 | Dachshund | F | 6 | Th12–13 | ventral | 3 | no | subacute | 3 | 3 | 2 | 70–115 | 7 | ||||
| 8 | 1 | Pekingese | F | 12 | Th12–13 | right | 3 | no | subacute | 2 | 2 | 2 | 160–180 | 9 | ||||
| 9 | 1 | Cocker Spaniel | F | 9 | L1-L2 | right | 1 | yes | acute | 2 | 3 | 2 | 70–115 | 7 | ||||
| 10 | 1 | Dwarf-Dachshund | M | 3 | Th13-L1 | right | 2 | no | subacute | 3 | 3 | 3 | 70–115 | 8 | ||||
| 11 | 1 | Dachshund | M | 5 | Th13-L1 | right | 2 | yes | subacute | 4 | 4 | 2 | 70–115 | 8 | ||||
| 12 | 2 | Beagle | M | 4 | no MRI data | none | — | — | — | 70–115 | 3 | |||||||
| 13 | 2 | Beagle | F | 4 | no MRI data | none | — | — | — | 70–115 | 4 | |||||||
| 14 | 2 | Beagle | M | 5 | no MRI data | none | — | — | — | 70–115 | 4 | |||||||
- M, male; F, female; SF, spayed female.
DISCUSSION
Our primary goal was to assess ITP in chondrodystrophic dogs with naturally occurring thoracolumbar disk extrusion while under general anesthesia and with an intraoperative blood pressure within physiologic range. In most group 1 dogs, ITP ranged from 5–8 mmHg whereas significantly lower values (3–4 mmHg) were measured in the control group. A local decrease in SCBF may have been the consequence of increased ITP in our dogs with thoracolumbar disk extrusion.10 Because of the small number of dogs evaluated, no statistical correlation between duration and grade of neurologic signs, degree of vertebral canal impingement, 24 hour outcome, and ITP could be established.
In our dogs, frequency of lesion localization, breed, and gender distribution were similar to previous reports of canine thoracolumbar intervertebral disk disease.20, 21
Recovery rates after the extended hemilaminectomy in our dogs were also consistent with previous reports after standard hemilaminectomy.22, 23 No clinical signs of instability were observed in our dogs after extension of the hemilaminectomy over 2 intervertebral disk spaces, consistent with results of a biomechanical study.24 The temporary clinical worsening observed in 2 dogs may be explained by manipulation of the spinal cord during insertion of the catheter into the subarachnoid space, or to causes unrelated to catheter insertion.
We are unaware of other clinical studies describing ITP measurement methods in chondrodystrophic breeds precluding any direct data comparison. In an experimental study, Kazama et al. found ITP in dogs without spinal disease to be slightly higher, with mean ± SD values of 5 ± 2 mmHg.18 Because of different ITP measurement methods and the use of mixed breed dogs (weight, 11–22 kg) not clearly characterized as chondrodystrophic, data cannot be directly compared with our results, which indicate that thoracolumbar disk extrusion in chondrodystrophic dogs resulted in an elevated ITP. As demonstrated by Griffith et al., when spinal cord perfusion pressure (SCPP) decreased secondary to an increasing ITP, SCBF remained constant until SCPP fell to levels in the 50 mmHg range. It was concluded that perfusion pressure is of greater importance in determining SCBF than the ITP.25
Other studies have established that an elevated ITP may lead to a reduced SCBF in people 9 and in experimental dogs.18 Because of the small body size of our dogs and limited access to the spinal cord, it was technically impossible to measure SCBF or medullary partial oxygen saturation simultaneously with ITP without risking iatrogenic injury to the spinal cord. In light of the results of a previous study, our observations suggest that in chondrodystrophic dogs with acute intervertebral disk extrusion an increase in ITP may elicit a decrease in SCBF.10 Reducing SCBF may result in ischemia or worsening of a preexisting ischemia, a well-known complication especially in human thoracoabdominal aneurysm surgery.14, 16, 26
Although controversy exists about its clinical value, CSF drainage is commonly performed during thoracoabdominal aneurysm surgery in people to lower the ITP and to enhance SCBF.14-17, 27, 28 CSF drainage is hypothesized to improve outcome in spinal cord injury where ITP is elevated.9 Other studies have confirmed that elevation of ITP significantly reduced SCBF; however, CSF drainage only increased SCBF in circumstances where ITP was abnormally elevated.18 In dogs, lowering normal range ITP through drainage of CSF per se did not increase SCBF, but if ITP was abnormally elevated to 20 mmHg or even 40 mmHg, SCBF was significantly reduced.18 In these cases, lowering ITP through CSF drainage led to improved SCBF, although SCBF did not regain initial levels.18 Consequently one can assume that a durotomy, during which CSF leakage occurs, may have effects similar to direct CSF drainage and may also reduce ITP. It has been suggested that durotomy relieves, to some degree, intramedullary compression in chondrodystrophic dogs with naturally occurring disk extrusion, but its real therapeutic value is still debated.29, 30 In our study, ITP in dogs with disk extrusion was significantly elevated compared with ITP in healthy dogs (control group); however, ITP of dogs with disk extrusion (group 1) were less than those reported in the experimental study by Kazama et al.18 Based on the observation that SCBF only seems to be influenced where ITP is markedly increased (up to 20/40 mmHg), it may be hypothesized that the effect of a CSF drainage (durotomy) on SCBF may depend on the magnitude of ITP increase. Therefore the use of durotomy should probably be reserved for such cases.
The increased ITP is also a possible explanation for thinning of the contrast medium column on myelography and of subarachnoid CSF space on MRI, a thinning which most often extends far beyond the visible area of compression. As discussed above, the extruded disk material leads to an increased subdural pressure. Because the subarachnoid space is the least resistive space, it might be the first space to collapse.
Some additional limitations should be considered when interpreting our results. One limitation is the limited number of dogs with high neurologic severity grade (group 1 only had 2 dogs at grade 4 and no grade 5 dogs). Severity of neurologic signs may be associated with higher ITP and could support the hypothesis of SCBF improvement after ITP release. Previous studies with identical set-up in which paraparetic dogs were enrolled assessed SCBF after durotomy.10, 30 Blaser et al. showed that directly after decompression and durotomy a decrease in SCBF occurred.30 One of the main limitations of our study is that using a fiberoptic catheter intraoperatively does not allow ITP recording before surgery or in the hours or days after surgery. This aspect would have been of interest because Kwon et al., investigating the effect of CSF drainage in human spinal cord injury, observed a reduction in ITP 40 hours after decompression and drainage, but not in the non-drainage group.9
The non-invasive blood pressure assessment we used only allowed a rough determination of MAP because the size of the cuff can significantly influence the results. An invasive measurement of the blood pressure might have been more precise. We also did not use invasive diagnostic techniques such as biopsy, as this would likely have influenced clinical outcome. Therefore the degree of induced ischemia and the effects of increased ITP at a microscopic level remain unclear. In rabbits, CSF drainage resulted in significantly smaller areas of tissue damage at the injury site 4 weeks after injury compared to that without CSF drainage. Improved histologic outcome did not however correlate with improvements in either motor or electrophysiologic outcome.31 With the measurements limited to the site of extrusion only, we were unable to establish whether the increase in ITP is a focal, more extended, or even generalized process. Furthermore, the present population is composed of a small number of dogs with naturally occurring disk extrusion and severity of spinal cord lesions might have been different in each single dog. We presumed control dogs had entirely normal spines but did not confirm this with either MRI or histology. Another limitation might be the different anatomic locations of the measurements (control group all at T13–L1, clinical group at different sites). Whether anatomic location influences ITP values is unknown. Any conclusion should be drawn accordingly.
In summary, we found a significant elevation of ITP in chondrodystrophic dogs with naturally occurring thoracolumbar disk extrusion and preserved deep pain sensation compared with healthy control dogs. Results of a previous study30 do not support the use of durotomy as a means to lower ITP in an attempt to increase SCPP, in dogs with mild increases in ITP such as those observed in the paraparetic and paraplegic dogs in our study.
DISCLOSURE
The authors report no financial or other conflicts related to this report.