Arytenoid Lateralization for Management of Combined Laryngeal Paralysis and Laryngeal Collapse in Small Dogs
Abstract
Objective
To identify combined laryngeal paralysis and collapse in small dogs and describe postoperative outcome after arytenoid lateralization.
Study Design
Case series.
Animals
Small nonbrachycephalic breed dogs with laryngeal paralysis and collapse (n = 6).
Methods
Medical records of small breed dogs with airway problems and undergoing laryngeal surgery (January–December 2008) were reviewed. Dogs with combined laryngeal paralysis and laryngeal collapse (LPLC) had arytenoid lateralization. The immediate, 4 week and 6 month postoperative outcomes were described.
Results
Direct visual laryngeal exam under a light plane of anesthesia revealed bilateral failure of arytenoid and vocal fold movement and concurrent bilateral medial folding with contact of the cuneiform processes in all dogs. None of the dogs had intra- or immediate postoperative complications after arytenoid lateralization. Two dogs required a 2nd contralateral procedure. Follow-up after 6 months revealed marked improvement in clinical signs related to upper airway obstruction, but all dogs continued to have mild respiratory noise.
Conclusion
Concurrent laryngeal paralysis and collapse should be considered as part of the differential diagnosis for small, nonbrachycephalic dogs with upper airway disease. Arytenoid lateralization resulted in improvement of clinical signs related to obstructive airway disease.
Laryngeal paralysis, failure of arytenoid cartilage, and vocal fold abduction is commonly seen in older medium to large breed dogs.1-3 The cause of paralysis may be idiopathic, congenital, traumatic, neoplastic, or iatrogenic.4, 5 Recent evidence strongly suggests that dogs with idiopathic laryngeal paralysis may have an underlying chronic progressive polyneuropathy.6 Laryngeal collapse has been frequently reported as part of the brachycephalic airway obstructive syndrome7-10 and also as a congenital condition.11 Collapse of the larynx can result from excessive negative pressure or a partial vacuum that occurs in the upper respiratory system. Over an extended period, the larynx will undergo changes in response to negative airway pressure.11 The laryngeal cartilage eventually weakens in the face of the chronically exaggerated intraluminal pressure.5 Laryngeal paralysis causes increased resistance to airflow and therefore creates turbulence and abnormal negative pressures in the glottis.
The combined presentation of laryngeal paralysis with tracheal collapse has been reported12; however, to our knowledge this is the 1st report of the combined presentation of laryngeal paralysis and laryngeal collapse (LPLC) in small nonbrachycephalic dogs.
Unilateral arytenoid lateralization has been reported as a successful treatment for long-term management of laryngeal paralysis, 2, 4, 13, 14 but there are few studies that evaluate its role in the management of laryngeal collapse and combined LPLC. Our purpose was to identify the presence of combined LPLC in small dogs and describe postoperative outcome after arytenoid lateralization. We hypothesized that nonbrachycephalic small breed dogs with LPLC would have a successful outcome after arytenoid lateralization.
MATERIALS AND METHODS
Inclusion Criteria (Table 1)
Medical records for all small breed (<10 kg) dogs with airway problems and undergoing laryngeal surgery in our clinic (January–December 2008) were reviewed. Data retrieved included breed, age, sex, medical history, clinical findings, and results of routine laboratory investigations. All dogs included in the study had thoracic and cervical radiographs, laryngoscopy, tracheostomy, and bronchoalveolar lavage (BAL) performed. Dogs were included if no neurologic abnormalities were detected. Findings and details of the surgical treatment were reviewed together with findings of clinical examination 4 weeks after surgery and a telephone follow-up 6 months after surgery.
| Further Surgery/ | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Weight | Biochemical | Bacteriology | Postoperative | ||||||
| Dog | Breed | Age | Sex | (kg) | Clinical Signs | Abnormalities | BAL | Previous Surgery | Laryngeal Inspection |
| 1 | Cavalier King Charles Spaniel | 10 years | NM | 10 | Inspiratory stridor, coughing, exercise intolerance | Raised ALT, ALP, and GGT | Tonsillectomy, palatoplasty | ||
| 2 | Yorkshire Terrier | 8 years | NF | 4.05 | Inspiratory stridor, coughing, dyspnea | Raised ALT, ALP, and GGT | Pasteurella sp | Intraluminal tracheal stent | |
| 3 | Yorkshire Terrier | 5 years 1 month | F | 4.6 | Inspiratory stridor, coughing, cyanosis | Raised ALT, ALP, and GGT | Right side arytenoid lateralization (22 days) | ||
| 4 | Yorkshire Terrier | 11 years 1 month | F | 3.5 | Inspiratory stridor, exercise intolerance, cyanosis, syncope | Pasteurella sp | Palatoplasty | Ovariohysterectomy for pyometra (88 days) | |
| 5 | Pomeranian | 3 years 7 months | NF | 5 | Inspiratory stridor, exercise intolerance, cyanosis, syncope | Escherichia coli | Right side arytenoid lateralization (97 days) | ||
| 6 | Jack Russell Terrier | 11 years | NF | 7.2 | Inspiratory stridor, coughing, dyspnea | E. coli | Tracheostomy | Cholecystectomy for cholangiohepatitis (112 days) |
- NM, neutered male; NF, neutered female; F, female; ALT, alanine transferase; ALP, alkaline phosphatase; GGT, gamma-glutamyltransferase.
Surgical Technique
Airway obstruction was managed by cricoarytenoid lateralization. Dogs were positioned in lateral recumbency for a left lateral cervical approach. After skin incision, the subcutaneous tissue and panniculus muscle were incised to expose the thyroid cartilage. The thyropharyngeus muscle was separated along the direction of the muscle fibers. The dorsal cricoarytenoid muscle was identified and sharply transected in its mid-body. The caudal part of the cricoarytenoid articulation was disrupted to disarticulate the muscular process of the left arytenoid cartilage. Polypropylene suture (1.5 metric) was passed through the cricoid cartilage in a caudocranial direction at the origin of the dorsal cricoarytenoid muscle. The needle was then passed in a mediolateral direction through the muscular process of the arytenoid cartilage and then in a lateromedial direction to create a mattress suture pattern. The suture was anchored without excessive tension resulting in abduction of the arytenoid cartilage. The fibers of the thyropharyngeus muscle were reapposed using 1.5 metric polyglactin 910 and the surgical incision closed in layers.
The rima glottidis was inspected by direct observation postoperatively to ensure that there was an increase in diameter compared with the presurgical diameter. Postoperative analgesia was maintained with opiates (methadone followed by buprenorphine) and nonsteroidal antiinflammatory drugs (carprofen), according to each dog's pain score based on a modified Glasgow pain-scoring system. Dogs were continually monitored for any signs of respiratory distress or difficulty. All dogs were fed their normal diet immediately after surgery and discharged within 3 days.
Statistical Analysis
Descriptive statistics with all results listed as median with range as appropriate.
RESULTS
Six dogs (Table 1) were included. Breeds were Yorkshire Terrier (3), Pomeranian (1), Cavalier King Charles Spaniel (1), and Jack Russell Terrier (1). Median weight was 4.8 kg (range, 3.5–10 kg). Three dogs were spayed females, 2 were intact females and 1 was a castrated male. Median age was 9 years (range, 3 years 7 months–11 years 1 month). Four dogs had a history of previous upper airway surgery including tonsillectomy (1), palatoplasty (2), semipermanent tracheostomy (1), and intraluminal stenting for tracheal collapse (1). The most common presenting signs were: increased respiratory noise (6), coughing (4), cyanosis (3), and exercise intolerance (3). Syncope (2) and respiratory distress (2) were less frequently observed.
Abnormalities on physical examination reported in all dogs included increased respiratory effort and stridor on laryngeal auscultation. One dog had a Grade-III heart murmur. No major abnormalities were identified on complete blood count and serum biochemical profile analysis. Mild elevation in liver enzymes (ALT, ALP, GGT) was observed in 2 Yorkshire Terriers and the Cavalier King Charles Spaniel. Echocardiography findings for dog 1 with a Grade-III heart murmur showed mild-to-moderate mitral valve regurgitation with thickened mitral valve leaflets, but normal left ventricle wall motion was found.
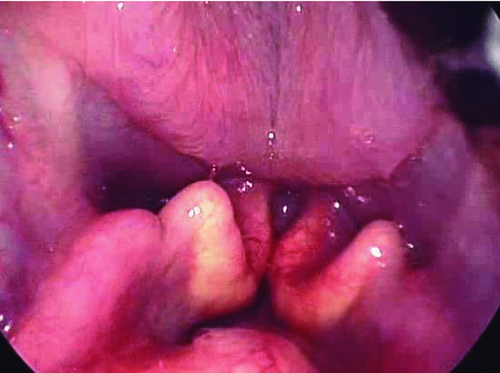
Direct visual laryngeal exam under a light plane of anesthesia revealed bilateral failure of arytenoid cartilage and vocal fold movement, consistent with laryngeal paralysis in all 6 dogs. Concurrent bilateral medial folding with contact of the cuneiform processes was evident in all dogs (Fig 1). Eversion of the saccules or involvement of any of the other laryngeal cartilages was not identified. Thoracic radiographs revealed mild tracheal collapse in 2 dogs (dogs 4, 5). No radiographic abnormalities were seen in the cervical region. Tracheoscopy confirmed mild collapse (Grade 1) in the region of the thoracic inlet with mild erythema and inflammation of the tracheal mucosa in dogs 4, 5. No substantial tracheal collapse was observed during endoscopy in dog 2 that had undergone intraluminal stenting, however, there was some inflammation around the cranial and caudal part of the stent with granulation tissue formed around these areas. BAL results showed suppurative inflammation with mixed bacterial infection in 4 dogs; bacteria isolated were Pasteurella sp (2) and Escherichia coli (2).
No complications were observed before discharge. Two dogs required a contralateral arytenoid lateralization procedure at days 22 (dog 3) and 97 (dog 5) because of right sided collapse and ongoing respiratory difficulty. The remaining dogs were reexamined 4 weeks after surgery and had no obvious inspiratory stridor. None of the dogs were coughing, were no longer cyanotic after mild exercise, and had improved exercise tolerance; however, mild stridorous wheeze was heard on laryngeal auscultation. Dogs 4 and 6 had unrelated anesthetic and surgical procedures at 88 and 112 days after arytenoid lateralization. Direct visual inspection of the larynx under a light plane of anesthesia in dogs 3, 5, and 6 showed good abduction of the left arytenoid cartilage with no sign of medial displacement or folding of the right arytenoid in dogs 4 and 6. Dogs 3 and 5 that required contralateral procedures were reexamined 4 weeks after the 2nd surgery and were progressing well, with similar improvement in clinical signs.
All owners were contacted by telephone at least 6 months after surgery and questioned about their dog's respiratory noise during rest and exercise, exercise tolerance, coughing episodes, and if they had cyanosis of their mucous membranes or collapsing episodes. All dogs had marked improvement of clinical signs related to the upper airway obstruction, with increased exercise tolerance, and no further coughing episodes. None of the dogs had experienced a collapsing episode and all owners perceived a reduction in inspiratory stridor.
DISCUSSION
Laryngeal paralysis occurs with failure of vocal fold abduction and is most commonly reported in older medium to large breed dogs.1, 4, 5 A congenital form of the condition has been described in Bouvier de Flandres, Bull Terriers, Dalmatians, Rottweilers, and Huskies.2 It has also been described in cats.15 The incidence of laryngeal paralysis in dogs <25 kg ranges from <4% to 13% in previous studies.4, 13 The underlying cause of most cases of acquired laryngeal paralysis remains unclear and the condition is frequently described as idiopathic.1, 4, 5 A recent report suggests that some dogs diagnosed with idiopathic laryngeal paralysis have a chronic, progressive polyneuropathy, and that until the disease is better understood, it may be better referred to as ‘‘geriatric onset laryngeal paralysis polyneuropathy syndrome.’’6 Any underlying causes should be ruled out. No neurologic abnormalities were detected in any of our dogs, but EMG and thyroid function tests were not routinely performed. Several reports describe the incidence of laryngeal paralysis in combination with other upper airway diseases in small dogs, most notably tracheal collapse.12 A previous report describes the diagnosis of laryngeal paralysis in brachycephalic dog 7; however, we are unaware of reports of concurrent LPLC in dogs.
We found elevated liver enzymes (ALP, ALT, GGT) in 3 dogs with laryngeal dysfunction. This is similar to a previous study, which concluded that hypoxia can induce hepatocellular damage and can lead to chronic hepatic dysfunction.16 All dogs in our series with combined LPLC had signs of inspiratory stridor, coughing, and exercise intolerance. These signs are typical clinical features of laryngeal paralysis.1, 4, 5 An additional and prominent feature of LPLC was the presence of high-pitched wheezes localized to the larynx on auscultation.17 All dogs in our series had bilateral laryngeal paralysis with early changes of laryngeal collapse. These consisted of medial folding with contact of the cuneiform processes but surprisingly there was no eversion of the laryngeal saccules. Although previous reports have described a grading system for laryngeal collapse,9-11 we felt that it could not be applied to our dogs because the criteria for early changes, namely eversion of the saccules was not evident despite all dogs having marked folding of the cuneiform processes.
Although arytenoid lateralization is not limited by patient size and has been reported to be successful in small breeds and even cats,4, 15, 18, 13 it is not normally considered appropriate for the management of laryngeal collapse because generalized weakening of the cartilaginous structures does not provide sufficient support for the lateralized arytenoid cartilage.3 However, we found that in these dogs the laryngeal cartilages were still strong enough to permit surgical correction. In 4 dogs, we reexamined the larynx after left arytenoid lateralization. Two dogs required a contralateral procedure because of a moderate degree of laryngeal collapse caused by medial displacement of the right arytenoid process during inspiration.1, 19 Two dogs had a normal position of the right arytenoid cartilage without further collapse. We presume that these nonbrachycephalic breeds have concurrent LPLC that is related in a way we do not completely understand. It is also possible that these dogs have congenital malformed, medially displaced cuneiform processes that can lead to secondary laryngeal paralysis.
Recurrent clinical signs associated with an inadequate glottic opening are reported after ineffective arytenoid lateralization and may result from failure to mobilize the arytenoid cartilage or undertensioning of the prosthetic suture.4, 19, 14 In our series, 2 dogs required a 2nd (contralateral) procedure. This was not considered because of an inadequate widening of the airway through technical failure but because of further medial displacement of the opposite arytenoid cartilage after initial lateralization. We suspect that this reflects the ongoing weakening of the cartilaginous structure.
Although aspiration pneumonia and dysphagia have been reported as complications after arytenoid lateralization,4, 20-22no major immediate or short-term complications were observed in our dogs. This may be explained by preservation of the function of the thyropharyngeus muscle by splitting it along its fibers instead of transecting them during the surgical exposure thereby maintaining postoperative swallowing function and reducing the risk of short-term aspiration because of dysphagia.22 Another explanation could be that laryngeal collapse caused continued reduction in the rima glottis opening, which prevented aspiration. All dogs were reexamined on at least 2 occasions postoperatively and a telephone follow-up call to owners was made after 6 months. The overall impression was of satisfaction among owners with all reporting improved exercise tolerance, reduced cough, and less respiratory noise, although all dogs continued to have a mild degree of inspiratory stridor.
Limitations of this study include its retrospective design, the small number of dogs evaluated, limited follow-up time (≥ 6 months), and reliance on subjective owner assessment of outcome. A number of aspects of LPLC remain unanswered including the cause of the underlying paralysis, the cause of the concurrent laryngeal collapse in small dogs that does not appear to be encountered in the many medium/large breed dogs with laryngeal paralysis. Concurrent laryngeal paralysis and collapse should be considered as part of the differential diagnosis for small, nonbrachycephalic dogs with upper airway disease. Arytenoid lateralization appears to be effective for LPLC and results in improvement of clinical signs, providing a comparatively simple surgical solution with minimal intra- and postoperative complications.