Investigation of Optimal Parameters Setting for Negative Pressure Wound Therapy With Instillation and Dwell Time for Hard-To-Heal Wounds With Necrotic Tissue
Funding: The article processing charge (APC) was supported by Solventum.
ABSTRACT
Negative Pressure Wound Therapy (NPWT) is a standard treatment for chronic wounds. In 2017, NPWT with instillation and dwell time (NPWTi-d) was approved for insurance coverage in Japan. This study aimed to identify optimal NPWTi-d parameter settings for hard-to-heal wounds with necrotic tissue. We conducted a retrospective observational study of consecutive patients treated with NPWTi-d between August 2017 and February 2019. Parameters analyzed included dressing change frequency (three times per week vs. once per week), therapy duration (2, 3, or 3.5 h), negative pressure levels (50–125 mmHg), dwell time (1–10 min), and instillation volume (mL/cm3 of foam). Fifty-six patients were included. Among the 52 patients managed with once-weekly dressing changes, five developed infections. A dwell time of ≥ 5 min significantly shortened the median treatment period to 11 days, compared to 26 days in those with shorter dwell times. NPWTi-d is more effective when treatment parameters are optimized. A dwell time over 5 min and once-per-week dressing replacement are sufficient, reducing both patient burden and healthcare provider workload. These findings provide evidence-based guidance for the efficient clinical use of NPWTi-d.
Summary
- Negative Pressure Wound Therapy (NPWT) is a widely used technology that accelerates wound healing by applying sub-atmospheric pressure to the wound surface, either continuously or intermittently.
- Negative Pressure Wound Therapy with instillation and dwell time (NPWTi-d) combines conventional negative pressure therapy with the intermittent delivery and short-term retention of topical solutions in the wound bed.
- The aim of this study is to determine the optimal NPWTi-d settings for treating hard-to-heal wounds with necrotic tissue. We performed a retrospective analysis to identify the parameters used in clinical cases and evaluate their impact on wound healing outcomes.
- Establishing these optimal parameters could lead to more effective and targeted use of NPWTi-d in clinical practice.
- A dwell time exceeding 5 min was found to be optimal, particularly when the dressing was changed once per week in cases without tendon exposure. The average of WBC significantly decreased between before and after applying NPWTi-d.
1 Introduction
Negative Pressure Wound Therapy (NPWT) is a widely used technology that accelerates wound healing by applying sub-atmospheric pressure to the wound surface, either continuously or intermittently. This device promotes wound healing through drainage and mechanical stress [1, 2]. NPWT is considered the global standard of care for hard-to-heal wounds and is recommended by numerous clinical guidelines [3-6].
A recent advancement in this field is Negative Pressure Wound Therapy with instillation and dwell time (NPWTi-d). NPWTi-d combines conventional negative pressure therapy with the intermittent delivery and short-term retention of topical solutions in the wound bed. This dual-function active therapy has shown promise in reducing bacterial load [7-11] and enhancing wound bed preparation [12]. The cyclic instillation and cleansing of the wound under closed, regulated conditions may also help limit pro-inflammatory markers while improving the removal of wound contaminants. Additionally, the hydromechanical effect of NPWTi-d enhances the overall efficacy of traditional NPWT.
Kim et al. conducted a survey involving 11 international wound care experts to explore the optimal NPWTi-d parameters [6]. However, evidence-based studies to establish these parameters remain limited.
The aim of this study is to determine the optimal NPWTi-d settings for treating hard-to-heal wounds with necrotic tissue. We performed a retrospective analysis to identify the parameters used in clinical cases and evaluate their impact on wound healing outcomes. Establishing these optimal parameters could lead to more effective and targeted use of NPWTi-d in clinical practice.
2 Methods
2.1 Study Design
We conducted a retrospective, observational study of consecutive patients with hard-to-heal wounds containing a small amount of necrotic tissue, with infection under control, who were treated with NPWTi-d between August 2017 and February 2019.
Ethical approval was obtained from the Institutional Review Board of Kyorin University Hospital (Approval No. R06-1102453). Informed consent was obtained using an opt-out method in accordance with institutional guidelines.
2.2 Participants
Our hospital is a 1153-bed acute care facility with 43 units, located in Tokyo, Japan. In our department, we manage a large number of patients with chronic or complex wounds using NPWT.
Patients with deep sternal wound infections or those who received NPWTi-d as a bridge to reconstructive surgery were excluded from this study, as the therapy was often discontinued before achieving more than 80% granulation coverage.
2.3 Duration, Dressing, and Endpoint of NPWTi-d
In Japan, NPWTi-d is reimbursed by the national health insurance system for a maximum duration of 4 weeks. As of February 2019, the ROCF-CC dressing had not yet been approved for use in Japan. According to the Pharmaceuticals and Medical Devices Agency (PMDA) in Japan, the evaluation of NPWT clinical outcomes is based on the period from the initiation of therapy until 80% of the wound area is covered by granulation tissue [13]. Alternatively, the endpoint may be defined as the time at which the wound is ready for definitive closure, either by simple surgical intervention such as direct closure or skin grafting.
2.4 Data Collection and Investigated Parameters
In this study, we investigated key parameters of NPWTi-d. The survey items included: (1) frequency of dressing changes (three times per week vs. once per week), (2) total NPWT duration per cycle (2, 3, or 3.5 h), (3) negative pressure settings (50, 75, 100, or 125 mmHg), and (4) dwell volume, defined as the volume of saline instilled per wound area (based on foam size), and (5) dwell time (1, 2, 3, 5, or 10 min). Negative pressure settings varied according to clinical context: 50, 75, or 100 mmHg were applied for patients with chronic limb-threatening ischemia (CLTI), while 125 mmHg was used for non-CLTI cases. Saline was used as the instillation solution in all cases.
We also assessed six potential patient-related factors that could influence wound healing: age, gender, diabetes status, haemodialysis status, white blood cell (WBC) count, and C-reactive protein (CRP) level.
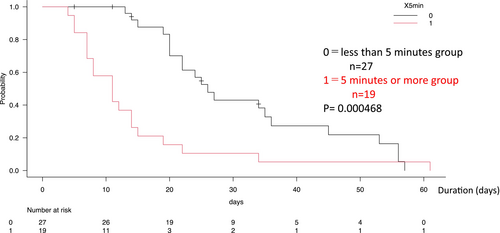
We investigated stratified analysis based on the duration from the start of NPWTi-d to achievement of ≥ 80% wound granulation, comparing dwell times of < 5 min and ≥ 5 min.
The clinical endpoint was defined as the duration from the initiation of NPWTi-d therapy to the point at which ≥ 80% of the wound area was covered with healthy granulation tissue. Patients were stratified into two groups based on the dwell time during the instillation phase: < 5 min and 5 min or more. The outcomes of these two groups were compared to evaluate the potential impact of dwell time on wound healing.
2.5 Stastistical Analysis
Statistical analysis was performed using EZR version 1.68. Variables with a p-value of less than 0.05 were considered statistically significant. The log-rank test was used for comparison.
3 Result
A total of 61 patients with hard-to-heal wounds were initially treated with NPWTi-d in our department. Five patients were excluded from the analysis: those with deep sternal wound infections and those who underwent NPWTi-d as a bridge to surgery. Ultimately, 56 patients were included in the final analysis for the study. Parameter analyses (1–4), along with additional investigations (detailed below), were assessed across all 56 cases.
The mean duration of NPWTi-d application was 19.48 ± 16.51 days (± SD). The mean age (± SD) was 66.53 ± 10.47 years. Of the 56 patients, 45 (80.3%) were male and 11 (19.7%) were female. All patients had undergone maintenance debridement for hard-to-heal wounds on the foot or lower extremities, with a small amount of residual necrosis and infection controlled prior to the initiation of NPWTi-d. Among them, 42 (75%) patients had diabetes, and 24 (42.8%) patients were undergoing haemodialysis.
The etiologies of the wounds were distributed as follows: CLTI in 22 cases, necrotising fasciitis in 12, diabetic foot ulcers (DFU) in 9, venous leg ulcers in 3, osteomyelitis in 3, vasculitis in 2, haematoma in 2, blue toe syndrome in 1, burn in 1, and surgical site infection (SSI) in 1 case (Table 1). NPWTi-d therapy was discontinued once granulation tissue formation achieved 80% or more open wound area.
| Patient demographics | |
|---|---|
| Patients (n) | 56 |
| Age (Average ± SD) | 66.53 ± 10.47 |
| Male, n (%) | 45 (80.3%) |
| Female, n (%) | 11 (19.7%) |
| DM | 42 (75%) |
| Haemodialysis | 24 (42.8%) |
| Diagnosis of wound (n) | |
| CLTI | 22 |
| Necrotizing fasciitis | 12 |
| DFU | 9 |
| VLU | 3 |
| Osteomyelitis | 3 |
| Vasculitis | 2 |
| Hematoma | 2 |
| Blue toe syndrome | 1 |
| Burn | 1 |
| SSI | 1 |
- Abbreviations: CLTI, chronic limb-threatening ischemia; DFU, diabetic foot ulcer; DM, diabetes mellitus; SD, standard deviation; SSI, surgical site infection; VLU, venous leg ulcer.
3.1 The Parameters of Survey Items
- Frequency of dressing changes (three times per week vs. once per week): There were 4 cases of 3-times-a-week replacement setting without any infection occurrence. There were 52 cases of once-a-week replacement setting, with five (9.6% rate) infection cases (Table 2).
- Total NPWT duration per cycle (2, 3, or 3.5 h): The default setting for the NPWTi-d device at the time of this study was 3.5 h. Regarding NPWT time, there were 5 patients with 2 h, 14 patients with 3 h, and 37 patients with 3.5 h (Table 3).
- Negative pressure settings (50, 75, 100, or 125 mmHg): Regarding negative pressure, there were 4 cases with 50 mmHg, 4 cases with 75 mmHg, 14 cases with 100 mmHg, and 34 cases with 125 mmHg (Table 4).
- Dwell volume: Dwell volume was defined as the amount of saline instilled per wound area, adjusted for foam volume. The average wound area of the 56 cases was 45.8 ± 81.3 cm2 and the average dwelling volume was 28.3 ± 21.0 mL. When the thickness of the foam was 1 cm, the amount of dwelling volume per 1 cm3 was 0.61 mL.
- Dwell time (1, 2, 3, 5, or 10 min): We extracted cases in which ≤80% of the wound area was covered by good granulation tissue. To investigate the relationship between NPWTi-d dwell time and wound healing, cases in which observation could not be continued until the endpoint—due to death, infection, or missing data—were excluded. Of the 56 cases, one patient died, five developed infections, and four had no documented dwell time in the medical chart. Consequently, parameter analysis (5) and stratified analysis focusing on dwell time were conducted on the remaining 46 cases.
| Frequency | Cases | Infection cases (n = 56) |
|---|---|---|
| Once a week | 52 | 5 |
| 3 Times a week | 4 | 0 |
| NPWT (h) | n |
|---|---|
| 2 | 5 |
| 3 | 14 |
| 3.5 | 37 |
- Abbreviation: NPWT, Negative Pressure Wound Therapy.
| Negative pressure (mmHg) | n |
|---|---|
| 50 | 4 |
| 75 | 4 |
| 100 | 14 |
| 125 | 34 |
Among these, 27 cases were categorised into the group with a dwell time of less than 5 min (1 min: 25 cases; 2 min: 1 case; 3 min: 1 case), while 19 cases comprised the group with a dwell time of 5 min or more (5 min: 15 cases; 10 min: 4 cases) (Table 5).
| Dwell time (min) | n |
|---|---|
| < 5 min (n = 27) | |
| 1 | 25 |
| 2 | 1 |
| 3 | 1 |
| ≥ 5 min (n = 19) | |
| 5 | 15 |
| 10 | 4 |
3.2 Stratified Analysis Based on the Duration From the Start of NPWTi-d to Achievement of ≥ 80% Wound Granulation, Comparing Dwell Times of < 5 Minutes and ≥ 5 Minutes
A total of 46 patients who received NPWTi-d therapy were included in this dwell time analysis. Patients were stratified into two groups according to the dwell time during the instillation phase: < 5 min (n = 27) and ≥ 5 min (n = 19) (Figure 1). The outcomes of these groups were compared to assess the potential influence of dwell time on wound healing.

The median duration of NPWTi-d therapy was significantly shorter in the ≥ 5-min dwell time group, with a median of 11 days, compared to 26 days in the < 5-min group (Figure 2).
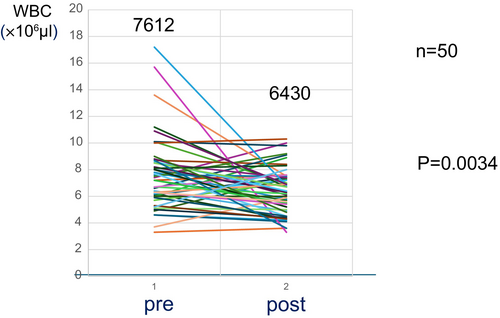
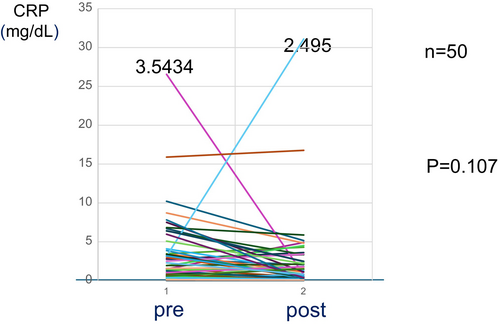
WBC count and CRP levels were compared before and after the application of NPWTi-d. The average WBC count showed a statistically significant decrease following NPWTi-d treatment (Figure 3). In contrast, the average CRP level did not show a significant change before and after NPWTi-d application (Figure 4).
4 Discussion
Medical devices related to wound healing are classified into two categories: (1) A medical device aimed at healing by secondary intention, epithelialisation, complete wound healing by accelerated wound healing, (2) A medical device that improves wound quality and achieves good granulation tissue formation, which is one of the goals of the wound healing process [13]. If ≥ 80% of the wound area is covered with healthy granulation tissue using the medical device described in 2, healing can be achieved in 2–3 weeks with simple surgical procedures such as direct sutures and skin grafting [13, 14]. NPWT is a medical device defined by category 2, improved wound quality, and the achievement of healthy granulation tissue formation. The technology was developed in the 1990s [1] and has evolved into the current state of the art in advanced wound care known as NPWTi-d. Compared to predicate NPWT technology, NPWTi-d therapy utilises an enhanced dressing architecture with improved hydrophilic properties combined with advances in device functionality of specifically automated wound cleansing cycles while the dressing remains in situ [7, 11]. In 2017, NPWTi-d received regulatory approval in Japan and has become a standard of care in hospital care settings across the country. Reimbursement is permitted for up to 4 weeks. Therefore, unlike in the US, therapy is not limited to a mandatory step down to conventional NPWT within 1 week.
Kim et al. reported the outcomes of a consensus meeting conducted by a multidisciplinary panel of global experts in the field of NPWTi-d [6]. The authors reviewed the current applications of NPWTi-d and the various wound etiologies treated with this therapy. Their findings were summarised in 11 consensus statements, which served as the first global guidelines for NPWTi-d use. However, these guidelines were based on expert opinion and empirical data rather than on high-level evidence. Therefore, we conducted an evidence-based study to further evaluate the effectiveness of NPWTi-d.
4.1 Parameter Setting
In general, both the volume of the cleansing solution and the duration of cleansing are critical factors in preventing wound infection. In the context of NPWTi-d, these aspects correspond to dwell volume, dwell time, and the frequency of dressing changes. Therefore, these parameters may play a significant role in infection control and should be carefully optimised during treatment planning.
4.2 Dwell Volume
We did not use the automatic mode to set the dwell volume, as it is time-consuming and often does not provide an appropriate amount. In our clinical experience, manually adjusting the dwell volume tends to yield more suitable results. Based on the findings of this study, we recommend a dwell volume of approximately 0.61 mL per 1 cm3 of foam when the foam thickness is 1 cm.
4.3 Frequency of Dressing Change and Infection
When NPWTi-d was first introduced at our hospital, dressing changes were performed three times per week due to concerns about wound infection. A few months after implementation, we observed the effectiveness of the device's cleansing function and developed confidence in its ability to regulate the wound environment. As a result, the dressing change frequency was reduced to once per week.
During the investigation period, we observed that cases with dressing changes performed three times per week were associated with no instances of infection. In contrast, infections occurred in five cases where NPWTi-d therapy was discontinued due to infection—all of which had been managed with weekly dressing changes and had exposed tendons following debridement.
We hypothesise that in these cases, infection may have spread along the exposed tendon and tendon sheath, leading to the formation of subcutaneous bacterial colonies. This condition may impair the cleansing effect of NPWTi-d in areas with exposed structures.
Based on these findings, we recommend maintaining a dressing change frequency of three times per week in cases involving exposed tendon or performing aggressive and thorough debridement until the tendon is completely removed. At our institution, weekly dressing changes are generally acceptable in the absence of tendon exposure. This approach minimises patient discomfort during foam changes and reduces the workload for healthcare providers.
4.4 Dwell Time and Wound Healing Period
The most significant finding of this study was the relationship between dwell time and the formation of healthy granulation tissue. The study endpoint was defined as the duration from the initiation of NPWTi-d therapy until ≥ 80% of the wound surface was covered with healthy granulation tissue.
Patients were classified into two groups based on dwell time: < 5 min: 27 cases; ≥ 5 min: 19 cases. The median duration of NPWTi-d therapy in the ≥ 5-min group was 11 days, which was significantly shorter than that in the < 5-min group. This indicates that longer dwell times were associated with more rapid granulation tissue formation.
Five patients in the < 5-min group developed infections and were subsequently excluded from the analysis. All five cases of infection involved tendon exposure with suspected tendon sheath infection. In each of these cases, the dwell time was short—either 1 or 2 min. Dwell volume was comparable to that used in non-infected cases, and all five patients underwent dressing changes once per week. The levels of negative pressure varied across these cases and did not show a consistent pattern.
These findings suggest that shorter dwell times may not fully exploit the granulation-promoting effects of NPWTi-d. In the early phase of NPWTi-d introduction at our institution, there was significant concern that treatment could be interrupted due to leakage of the irrigation solution. As a precaution, shorter dwell times of 1, 2, and 3 min were initially selected to minimise the risk of leakage.
However, as practical experience accumulated and measures to prevent leakage were implemented-such as improved sealing techniques and device handling-the incidence of leakage decreased. Consequently, longer dwell times of 5 and 10 min were gradually adopted in later cases.
This shift allowed for a more thorough instillation phase, potentially enhancing the therapeutic effect of NPWTi-d and contributing to improved wound healing outcomes observed in patients managed with longer dwell times.
Kim et al. previously reported that a dwell time of approximately 10 min is appropriate when using NPWTi-d [6, 7, 15]. Our results support this empirical recommendation, providing evidence-based validation for a ≥ 5-min dwell time as optimal for promoting effective granulation tissue formation.
4.5 Changes in WBC and CRP Before and After NPWTi-d
One patient who died and five patients who developed infections were excluded from this analysis.
WBC count significantly decreased following NPWTi-d treatment, while CRP levels showed no significant change. NPWTi-d promotes the formation of new granulation tissue, and its cyclic wound cleansing function may contribute to a reduction in infection risk. As a result, WBC—a common marker of infection—was observed to decrease after therapy. Although some patients discontinued NPWTi-d due to infection, the needs to debate over its effectiveness in infection control; it is possible that excluding cases with tendon exposure could lead to more favourable outcomes. NPWTi-d may offer greater adjunctive benefits when used in combination with systemic antibiotics [11].
4.6 Measures to Prevent Leakage
Due to concerns about leakage of the cleansing solution (saline), the initial dwell time was chosen to be as short as possible, 1 min.
However, in order to prevent leakage, we have created a dike by applying a thin strip of Adapt Skin Protection Seal (Hollister, USA) or Protective Seal (Brava) (Coloplast, Denmark) to the periwound prior to applying the adhesive drape. Using this approach, it was routinely possible to prevent the cleansing solution from overflowing from the wound area and peri-wound maceration.
1. Apply skin protectant; Cavilon was used.
2. Apply a paste of hydrocolloid for stoma to the peri-wound.
Not just any manufacturer's product will do, but we considered that Coloplast Brava's hydrocolloid was easy to use. It does not stick to gloves and sticks well to peri-wound skin.
3. When loading negative pressure to the NPWTi-d for 2 min and 30 s, applying pressure and warming the hydrocolloid with your hand to blend it on the film into the skin will reduce leakage.
If the dwell time was < 5 min, the performance of NPWTi-d cannot be fully utilised.
Based on the outcomes of this study, a dwell time of ≥ 5 min is recommended. We considered that 10 min is appropriate in dwell time because measures have been established within our hospital to prevent leakage when using NPWTi-d.
We did not observe limitations with NPWT time of 3 or 3.5 h, however; considering concerns of infection, 2 h is considered appropriate for wounds with necrotic tissue, where the possibility of infection is low. If there is a possibility of infection, we considered that increasing the number of dwell cycles by reducing the NPWT phase to 1 h was preferred.
4.7 Recommendation Parameters of NPWTi-d in Our Department
- NPWT time: 2 h (typical), 1 h (higher risk of infection).
- Dwell time: 10 min (> 5 min).
- Negative pressure: 125 mmHg (non-ischemia), 75, 50 mmHg (ischemia).
- Dwell volume: 0.6 mL/cm3.
- DPC mode: 3 min, 3 min.
- Replacement frequency: once a week (without exposed tendon).
4.8 Limitation
One limitation of this study is that all 56 patients presented with foot or lower limb wounds; therefore, the effects of NPWTi-d on wounds located in other anatomical regions could not be evaluated. Additionally, the retrospective design and relatively small sample size may limit the generalizability and broader applicability of the findings.
5 Conclusion
This study investigated parameters that promote granulation tissue formation without increasing the risk of infection during NPWTi-d therapy. Based on the results of this retrospective analysis, NPWTi-d appears to be an effective modality for wound management.
A dwell time exceeding 5 min was found to be optimal, particularly when the dressing was changed once per week in cases without tendon exposure. The average WBC count significantly decreased following the application of NPWTi-d.
When applied under standardised conditions, NPWTi-d can facilitate wound healing while reducing the frequency of dressing changes, thereby minimising patient discomfort and alleviating the burden on medical staff.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The authors have nothing to report.