RETRACTED: Effects of negative pressure wound therapy on wound infection and healing in patients with open fracture wounds: A meta-analysis
Abstract
A meta-analysis was conducted to comprehensively evaluate the impact of negative pressure wound therapy (NPWT) on wound infection and healing in patients with open fracture wounds. Computer searches were performed in EMBASE, Google Scholar, Cochrane Library, PubMed, Wanfang and China National Knowledge Infrastructure databases for randomized controlled trials (RCTs) on the application of NPWT in open fracture wounds, with the search period covering the databases inception to September 2023. Two researchers independently screened the literature, extracted data and conducted quality assessments. Stata 17.0 software was employed for data analysis. Overall, 17 RCTs involving 1814 patients with open fracture wounds were included. The analysis revealed that compared with other treatment methods, NPWT significantly shortened the wound healing time (standardized mean difference [SMD] = −2.86, 95% confidence intervals [CI]: −3.51 to −2.20, p < 0.001) and fracture healing time (SMD = −3.14, 95% CI: −4.49 to −1.79, p < 0.001) in patients with open fracture wounds. It also significantly reduced the incidence of wound infection (odds ratio [OR] = 0.36, 95% CI: 0.23–0.56, p < 0.001) and complications (OR = 0.29, 95% CI: 0.20–0.40, p < 0.001). This study indicates that in the treatment of open fracture wounds, NPWT, compared with conventional treatment methods, can accelerate the healing of wounds and fractures, effectively control infections and reduce the occurrence of complications, demonstrating high safety.
1 INTRODUCTION
Open fractures are one of the common diseases in trauma orthopaedics. Such fractures can easily cause skin and soft tissue defects, and the fracture site communicates with the external environment, making it more susceptible to environmental influences and thus having a higher infection rate than other types of fractures.1-3 If not handled properly, it may lead to complications such as systemic infection, non-union of fractures, delayed healing, amputation, prolonged course of disease and limb dysfunction.4-6 Despite advances in medical technologies such as debridement, irrigation, antibiotics and surgical treatment, the postoperative infection rate of open fractures worldwide still reaches up to 30%.7 Therefore, how to reduce the occurrence of wound infection and complications of open fractures and promote wound healing has always been a hot topic in trauma orthopaedic research.
With the improvement of modern medical technology and the continuous improvement of treatment methods, negative pressure wound therapy (NPWT) as a new treatment method has gradually been widely used in fractures, chronic non-healing wounds, diabetic feet and infected wounds, and has achieved good results.8-11 NPWT is a wound treatment technique that uses an intelligent negative pressure suction system to generate continuous or intermittent negative pressure in the closed part of the wound to fully drain, control infection and improve tissue perfusion, thereby promoting wound healing.12, 13 A large amount of clinical practice has proven that the implementation of NPWT can effectively control the occurrence of infections and promote wound healing, and has been widely recognized and accepted by doctors and patients.14, 15 Based on this, this study aims to evaluate the impact of NPWT on wound infection and wound healing in patients with open fractures through a meta-analysis, providing a basis for the reasonable use of new NPWT technology in clinical practice.
2 MATERIALS AND METHODS
2.1 Literature search
Keywords such as negative pressure wound therapy, NPWT, topical negative pressure therapy, negative pressure dressings, vacuum assisted closure and open fracture were used in combination with free-text terms to search EMBASE, Google Scholar, Cochrane Library, PubMed, Wanfang and China National Knowledge Infrastructure databases for randomized controlled trials (RCTs) on the application of NPWT in open fracture wounds, with the search period covering the databases inception to September 2023.
2.2 Inclusion and exclusion criteria
2.2.1 Inclusion criteria
(1) Participants: patients clinically diagnosed with open fractures confirmed by x-ray or other imaging; (2) intervention: control group receiving conventional treatment and experimental group receiving NPWT in addition to conventional treatment; (3) outcomes: wound healing time, fracture healing time, wound infection and complications; (4) study design: RCTs.
2.2.2 Exclusion criteria
Duplicate publications; literature lacking relevant raw data, incomplete raw data or unavailable full-text information; reviews, case reports, systematic reviews, conference articles and animal studies.
2.3 Data extraction and quality assessment
Imported literature into Endnote X9, removed duplicates and two researchers independently screened titles, abstracts and full texts based on inclusion and exclusion criteria. Discrepancies were resolved through discussion or with the assistance of a third researcher. Data extraction was performed using Excel, including first author, publication year, sample size, gender, age and outcome indicators (wound healing time, fracture healing time, wound infection and complications). Quality assessment of RCTs was conducted using the Cochrane Collaboration's risk of bias tool.
2.4 Statistical analysis
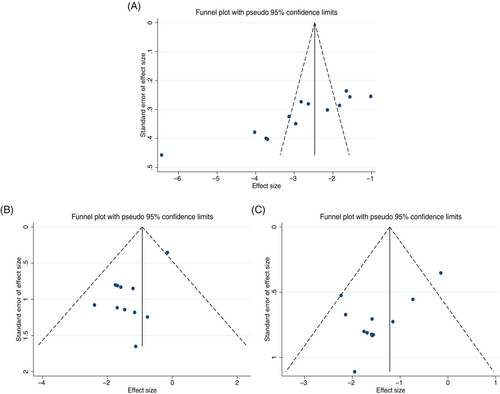
Stata 17.0 software was employed for data analysis. Binary variables were expressed using odds ratios (OR) with 95% confidence intervals (CIs) and continuous variables using standardized mean differences (SMD) with 95% CIs. Heterogeneity was determined using the χ2 test and I2 values. A fixed-effects model was employed when I2 < 50% and p > 0.1, indicating no significant heterogeneity; otherwise, a random-effects model was employed. Sensitivity analysis was conducted to assess the robustness of the study results. A funnel plot was used to assess publication bias when more than 10 studies were included.
3 RESULTS
3.1 Basic characteristics
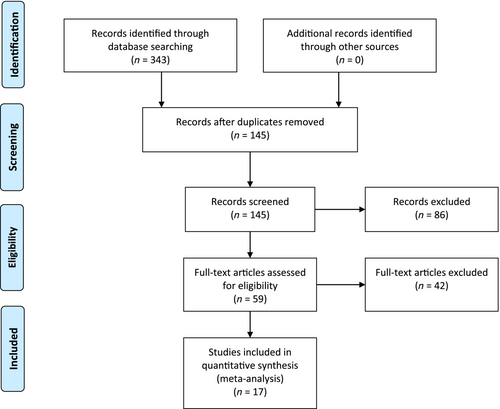
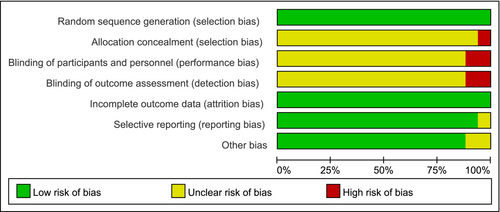
The literature screening process is shown in Figure 1. Initially, 343 articles were identified, 198 duplicates were removed manually and using software and 86 articles that did not meet the research content were excluded based on titles and abstracts. After full-text reading of the remaining 59 articles, 17 RCTs involving 1814 patients with open fractures were included,16-32 with 901 and 913 patients in the NPWT and control groups, respectively. The basic characteristics of the included literature are shown in Table 1. The risk assessment of the literature is shown in Figure 2.
| Author | Year | Number of patients | Age (years) | Sex (male/female) | |||
|---|---|---|---|---|---|---|---|
| Intervention | Control | Intervention | Control | Intervention | Control | ||
| Luo | 2021 | 43 | 43 | 42.52 ± 7.82 | 43.11 ± 7.48 | 27/16 | 28/15 |
| Lin | 2020 | 40 | 40 | 35.2 ± 7.7 | 35.3 ± 7.6 | 24/16 | 22/18 |
| Li | 2019 | 35 | 35 | 34.87 ± 5.87 | 36.74 ± 6.37 | 20/15 | 21/14 |
| Huo | 2021 | 54 | 54 | 39.01 ± 5.19 | 38.65 ± 5.21 | 36/18 | 35/19 |
| Hou | 2021 | 44 | 42 | 36.0 ± 4.8 | 37.0 ± 3.4 | 31/13 | 30/12 |
| He | 2018 | 45 | 45 | 43.5 ± 2.5 | 43.0 ± 2.0 | 25/20 | 23/22 |
| Cao | 2022 | 35 | 35 | 44.45 ± 10.36 | 43.87 ± 9.66 | 20/15 | 18/17 |
| Ma | 2021 | 35 | 35 | 36.01 ± 10.32 | 35.71 ± 10.01 | 19/16 | 20/15 |
| Costa | 2018 | 226 | 234 | 46.1 ± 19.9 | 44.5 ± 19.0 | 178/48 | 164/70 |
| Virani | 2016 | 43 | 50 | 34.8 | 37.4 | 28/15 | 32/18 |
| Zhang | 2022 | 35 | 35 | 46.74 ± 11.32 | 46.83 ± 11.24 | 23/12 | 21/14 |
| Yan | 2019 | 34 | 34 | 47.52 ± 3.35 | 46.28 ± 2.67 | 19/15 | 20/14 |
| Xu | 2021 | 48 | 48 | 42.38 ± 10.32 | 44.30 ± 14.27 | 27/21 | 30/18 |
| Xu | 2023 | 49 | 48 | 68.12 ± 12.37 | 67.42 ± 12.50 | 30/19 | 29/19 |
| Wang | 2020 | 40 | 40 | 39.78 ± 3.34 | 39.56 ± 3.26 | 22/18 | 21/19 |
| Wang | 2018 | 35 | 35 | 29.2 ± 7.4 | 27.1 ± 6.8 | 24/11 | 25/10 |
| Wang | 2021 | 60 | 60 | 45.84 ± 4.26 | 45.01 ± 4.12 | 33/27 | 32/28 |
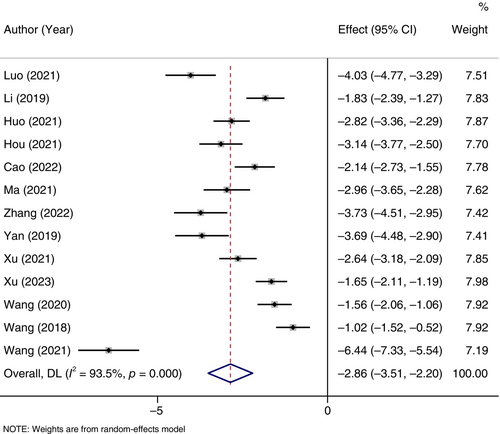
3.2 Wound healing time
Thirteen RCTs reported on wound healing time. There were 547 and 544 patients in the NPWT and control groups, respectively. Significant heterogeneity was found (I2 = 93.5%, p < 0.001), and a random-effects model was employed. It was found that the wound healing time in the NPWT group was significantly shorter than that in the control group (SMD = −2.86, 95% CI: −3.51 to −2.20, p < 0.001), as shown in Figure 3.
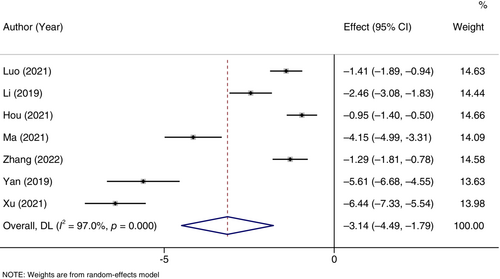
3.3 Fracture healing time
Seven RCTs reported on fracture healing time. There were 274 and 272 patients in the NPWT and control groups, respectively. Significant heterogeneity was found (I2 = 97.0%, p < 0.001), and a random-effects model was employed. It was found that the fracture healing time in the NPWT group was significantly shorter than that in the control group (SMD = −3.14, 95% CI: −4.49 to −1.79, p < 0.001), as shown in Figure 4.
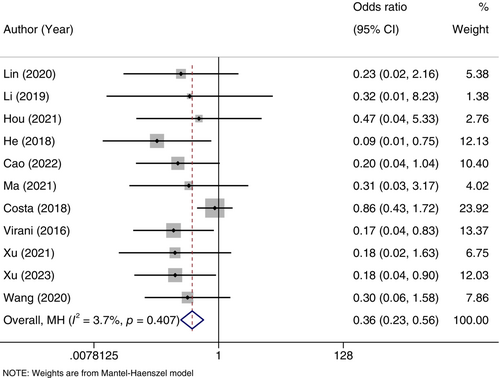
3.4 Wound infection
Eleven RCTs reported on wound infection. There were 640 patients in the NPWT group, with 29 developing wound infections, and 645 in the control group, with 77 developing wound infections. No significant heterogeneity was found (I2 = 3.7%, p = 0.407), and a fixed-effects model was employed. It was found that the incidence of wound infection in the NPWT group was significantly lower than that in the control group (OR = 0.36, 95% CI: 0.23–0.56, p < 0.001), as shown in Figure 5.
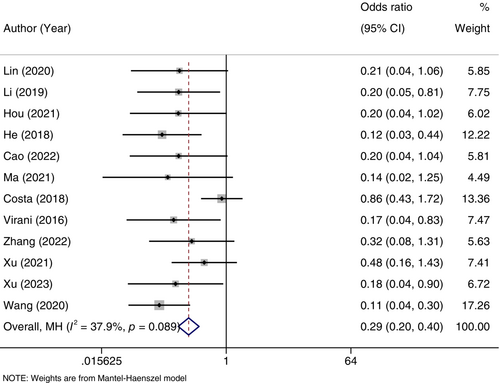
3.5 Complications
Twelve RCTs reported on complications. There were 675 patients in the NPWT group, with 50 experiencing complications, and 680 in the control group, with 144 experiencing complications. No significant heterogeneity was found (I2 = 37.9%, p = 0.089), and a fixed-effects model was employed. It was found that the incidence of complications in the NPWT group was significantly lower than that in the control group (OR = 0.29, 95% CI: 0.20–0.40, p < 0.001), as shown in Figure 6.
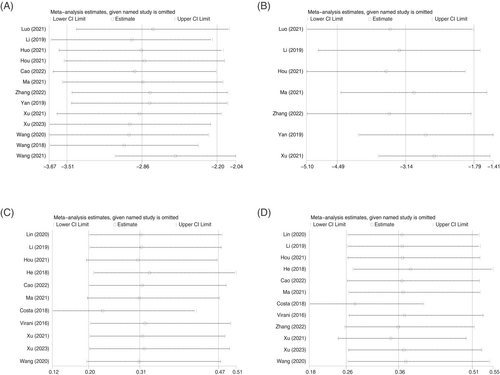
3.6 Sensitivity analysis and publication bias
Sensitivity analysis was conducted by eliminating individual studies one by one, indicating that the study conclusions are robust (Figure 7). The funnel plot, as shown in Figure 8, was mostly symmetrical for the outcome indicators of wound infection and complications, suggesting a low possibility of publication bias; however, the funnel plot for wound healing time was asymmetrical, indicating the possibility of publication bias.
4 DISCUSSION
Open fractures, often caused by violent trauma, are accompanied by soft tissue and skin defects. Compared with closed fractures, they carry a higher risk of infection and disability.33, 34 The treatment of open fracture patients must ensure bone healing and functional recovery of limbs while also preventing wound infection.35 Slow wound healing and various complications in open fracture patients are significant challenges for both victims and medical professionals.36, 37 Therefore, in the treatment of open fractures, emphasizing the prevention of infection and promoting early healing of wounds and fractures are of great importance.
NPWT is a non-invasive wound healing technique used for various complex wounds. Unlike traditional debridement and negative pressure drainage, NPWT works by creating sub-atmospheric pressure to reduce inflammatory exudates and promote granulation tissue growth, thereby optimizing wound healing.38, 39 In severe open fractures, significant damage and crushing to surrounding tissues occur, making wound cleaning and protection crucial.40 Traditional debridement requires constant attention to wound exudate, daily or alternate-day dressing changes, checks for granulation tissue growth and regular debridement of necrotic tissue, making the process cumbersome and prolonging the treatment period.41 Failure to timely drain exudates may lead to deep infections or other complications, causing prolonged non-healing of fractures and severely affecting patients' physical and mental health.42 NPWT simplifies treatment by covering the wound with specialized dressings, significantly reducing the risk of infection caused by dressing changes and drainage.43 By connecting the drainage tube to the negative pressure device for continuous suction, it promotes internal blood flow and stimulates the growth of surrounding granulation tissue, thereby reducing the time required for wound healing.44, 45 Continuous negative pressure suction also timely removes necrotic tissue, blood stasis, fluid and bacteria from the wound, effectively reducing the occurrence of infections and complications and accelerating wound healing.46, 47
This study included 17 RCTs involving 1814 patients with open fractures. The meta-analysis results showed that compared with the control group, the NPWT group had significantly shorter wound healing time and fracture healing time, and significantly lower rates of wound infection and complications. These results fully demonstrate the superiority of the NPWT treatment method, effectively reducing the risk of infection in patients, as well as decreasing the occurrence of complications, shortening the time for wound and fracture healing and accelerating the recovery process. Therefore, the clinical application of NPWT is significantly effective and deserves to be widely promoted.
However, this study still has limitations: Firstly, in addition to objective indicators such as wound healing time, fracture healing time, wound infection and complications, other evaluation indicators such as patient quality of life, satisfaction and costs should be included to comprehensively evaluate the application value of NPWT. Secondly, the total sample size of the included studies is relatively small, which might introduce bias into the meta-analysis results, necessitating further large-sample research in the future. Thirdly, a limited number of studies and sample sizes for certain indicators might influence the combined results. Future research should further explore the application value of NPWT in the treatment of open fractures through large-scale, high-quality RCTs, to provide more accurate evidence-based clinical evidence.
5 CONCLUSIONS
In summary, NPWT technology not only accelerates wound and fracture healing in open fractures but also reduces the occurrence of infections and complications. Its significant clinical treatment effect makes it worthy of widespread clinical implementation and promotion.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.