RETRACTED: Comparative effectiveness of pericapsular nerve group block versus fascia iliac compartment block on postoperative wound pain management in patients undergoing hip fracture surgery: A systematic review and meta-analysis
Abstract
Hip fracture surgeries are challenging, with postoperative pain management being a critical component of patient care. This systematic review and meta-analysis aimed to compare the effectiveness of Pericapsular nerve group block (PENGB) and fascia iliac compartment block (FICB) in postoperative wound pain management for patients undergoing hip fracture surgery. The study followed the PRISMA guidelines and was structured around the PICO framework. Comprehensive searches were conducted across PubMed, Embase, Web of Science, and the Cochrane Library. Inclusion criteria were limited to RCTs comparing the effectiveness of PENGB and FICB in adult patients undergoing hip fracture surgery. Key outcomes included pain control effectiveness, safety, and complication incidence. The quality of studies was assessed using the Cochrane Collaboration's risk of bias tool. Statistical heterogeneity was evaluated using I2 statistics, and meta-analysis effect values were calculated using random-effects or fixed-effect models, depending on the degree of heterogeneity. The search identified 1095 articles, with 5 studies meeting inclusion criteria. The meta-analysis revealed that PENGB and FICB were comparable in managing postoperative pain and opioid consumption. However, PENGB significantly reduced the incidence of quadriceps muscle weakness (RR = 0.12, p < 0.05) and did not increase the risk of PONV (RR = 1.36, p = 0.51), suggesting its advantage in maintaining motor function without adding to PONV complications. No significant publication bias was detected. PENGB is comparable to FICB in pain and opioid consumption management after hip fracture surgeries. Its significant benefit lies in reducing the incidence of quadriceps muscle weakness, facilitating better postoperative mobility. Additionally, PENGB does not increase the risk of postoperative nausea and vomiting, underlining its suitability for comprehensive postoperative care in hip fracture patients.
1 INTRODUCTION
Hip fractures, particularly prevalent in the elderly, present a significant challenge to public health due to their high incidence and associated morbidity and mortality. The management of these fractures, especially with Total Hip Arthroplasty (THA), is multifaceted, demanding not just surgical precision but also effective strategies for postoperative pain control.1, 2 Proper pain management is crucial as it promotes the initiation of physical activity and ambulation within the first 24 to 48 h following surgery, diminishes the risk of postoperative complications, and can substantially reduce the length of hospital stays.3, 4
The fascia iliac compartment block (FICB) has long been a traditional method for pain management in THA. The fascia iliac compartment block (FICB) has long been a traditional method for pain management in THA.5 This technique involves administering a local anaesthetic near the iliac fascia, desensitizing the area around the surgical site.6 While FICB is notably effective in mitigating postoperative pain, it comes with certain limitations. These limitations include a risk of local anaesthetic systemic toxicity (LAST), potential nerve damage due to direct needle trauma, a variable block effect due to anatomical variations, and the possibility of lower limb motor weakness.7 The latter is particularly concerning as it may impair the patient's ability to engage in early postoperative activities, potentially delaying the recovery process and extending the duration of hospitalization. Additionally, FICB may lead to an increased use of opioids due to its variable effectiveness in pain control, which can further complicate the postoperative recovery due to opioid-related side effects.8, 9 The primary concern is its potential to decrease motor strength at the surgical site. This reduction in motor strength can significantly hinder the patient's ability to perform early postoperative activities, possibly delaying the recovery process and extending the duration of hospitalization.
On the other hand, the Pericapsular Nerve Group Block (PENGB), a more recent technique, is emerging as a promising alternative to FICB. PENGB aims to anaesthetise the sensory nerves surrounding the hip joint, particularly focusing on the articular branches of the femoral and obturator nerves.10 Its appeal lies in its ability to provide effective pain relief while preserving motor function, which is paramount for early postoperative rehabilitation and recovery.
In the context of postoperative pain management following hip fracture surgeries, effective pain control plays a crucial role in mitigating several key complications. These include, but are not limited to, deep vein thrombosis (DVT), pulmonary embolism (PE), pneumonia, and urinary retention.11, 12 Effective pain management can reduce the incidence of DVT and PE by facilitating early mobilization, thus decreasing the risk of venous stasis. Furthermore, well-managed pain can decrease the risk of chronic pain development and psychological distress, such as anxiety and depression, which are often associated with prolonged pain experiences.13 Therefore, the implementation of effective pain management techniques, such as FICB and PENGB, not only addresses the immediate postoperative pain but also contributes significantly to reducing the overall risk of these postoperative complications, underscoring their importance in the comprehensive care of hip fracture patients.
Building upon the outlined comparison of FICB and PENGB, we hypothesize based on preliminary observations that PENGB might provide enhanced pain control with minimized side effects, notably in preserving motor function and reducing reliance on opioids. These observations form the basis of our hypothesis that PENGB could potentially emerge as a more effective and safer approach for managing postoperative pain in hip fracture surgeries, as compared to FICB. Our systematic review and meta-analysis are thus framed to rigorously investigate this hypothesis. Through an exhaustive analysis of existing clinical trials and observational studies, our study aims to deliver an in-depth comparison of these two techniques. We intend to assess not only their effectiveness in managing pain but also to examine their broader impacts on postoperative recovery processes, including the rate and quality of rehabilitation, incidence of complications, and overall patient outcomes. Such a comprehensive evaluation will not only validate or challenge our initial hypothesis but also aims to contribute significantly to the existing body of knowledge, potentially influencing future clinical practices in the realm of pain management for hip fracture patients.
2 MATERIALS AND METHODS
2.1 Search strategy
During our systematic review and the reporting of our findings, we adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.14 The meta-analysis was designed around the PICO framework, focusing on the following aspects: Patients undergoing hip fracture surgery, the PENGB as the intervention of interest, the FICB as the comparator, and outcomes including the effectiveness and safety of PENGB and FICB in postoperative wound pain management, patient recovery time, and the incidence of complications.
We conducted searches in four electronic databases: PubMed, Embase, Web of Science, and the Cochrane Library, on September 19, 2023, without imposing any time restrictions. Our search strategy employed key terms such as “hip fracture surgery,” “pericapsular nerve group block,” “ fascia iliac block,” “postoperative pain management,” “pain control,” and “total hip arthroplasty.” These keywords were carefully chosen to cover the broad scope of the PICO framework, ensuring a comprehensive collection of pertinent studies for the meta-analysis. We did not apply any language limitations. Additionally, we manually screened the reference lists of relevant articles to identify any further potential records.
2.2 Inclusion criteria and exclusion criteria
Inclusion Criteria: (1) Study Design: Randomized Controlled Trials (RCTs) examining the effectiveness of PENGB and FICB in hip fracture surgeries. (2) Participants: Adult patients (aged 18 years and older) undergoing hip fracture surgery. (3) Interventions: Studies that specifically evaluate the use of PENGB or FICB for postoperative wound pain management. (4) Comparators: Studies comparing PENGB with FICB. (5) Outcomes: Primary outcomes should include measures of pain control effectiveness and safety. Secondary outcomes may include patient recovery time, incidence of complications, and overall patient satisfaction post-surgery.
Exclusion Criteria: (1) Non-Relevant Studies: Studies not focusing on hip fracture surgery or those not evaluating PENGB or FICB. (2) Non-Adult Population: Studies involving paediatric populations or patients under 18 years of age. (3) Non-Original Research: Reviews, editorials, commentaries, and conference abstracts without full-text availability. (4) Incomplete Data: Studies with incomplete outcome data relevant to the comparison between PENGB and FICB. (5) Duplicate Publications: Studies that are duplicate publications or sub-studies of already included trials.
2.3 Data extraction
For your meta-analysis, the data extraction process was meticulously carried out. Two independent evaluators conducted literature screening and data extraction, with discrepancies resolved through discussion or, if necessary, consultation with a third-party reviewer. The data extracted encompassed general information of the included studies, such as authors, publication year, sample size, and types of surgical anaesthesia. Intervention details were also gathered, including methods, timing, concentration, and dosages of interventions. Outcome measures focused on aspects like pain scores, postoperative opioid use, incidence of postoperative nausea and vomiting (PONV), quadriceps muscle weakness rates, and patient satisfaction with pain management. When published reports lacked specific data, we contacted original study investigators to request any unpublished data.
2.4 Quality assessment
In conducting the meta-analysis, we appraised the quality of the included studies using the Cochrane Collaboration's risk of bias tool.15 This assessment was carried out independently by two reviewers, who scrutinized several key domains: the generation of random sequences, the concealment of allocation, blinding of both participants and personnel, the completeness of outcome data, the risk of selective reporting, and any other potential biases. Each of these domains was evaluated and categorized as having a low, unclear, or high risk of bias. In instances where the reviewers had differing opinions, the issues were resolved through discussion, or, when required, by involving a third-party reviewer to reach a consensus.
2.5 Statistical analyses
In our meta-analysis, we adhered to stringent statistical analysis protocols to ensure the accuracy and reliability of our findings. The heterogeneity among the included studies was evaluated using chi-square statistics, with the degree of heterogeneity quantified by the I2 value. Instances where the I2 value was below 50%, and the corresponding p-value was 0.10 or higher, were indicative of negligible significant heterogeneity. Under these conditions, a fixed-effect model was applied to calculate the combined effect size. Conversely, when the I2 value reached 50% or higher, or the corresponding p-value fell below 0.10, this denoted substantial heterogeneity. In scenarios characterized solely by statistical heterogeneity, the random-effects model was utilized to determine the combined effect size. To assess potential publication bias, we analysed the symmetry of the funnel plot. A balanced distribution of data points on both sides of the apex of the funnel plot would imply a lower risk of the results being skewed by publication bias. Furthermore, we employed Egger's linear regression test as a quantitative tool for detecting any publication bias. All statistical analyses were conducted using two-sided tests, with a p-value of less than 0.05 considered to indicate statistical significance. The data analysis was performed using Stata version 17 (StataCorp, College Station, TX, USA).
3 RESULTS
3.1 Search results and study selection
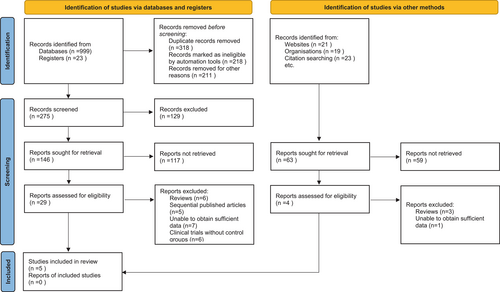
In the initial phase of our systematic review and meta-analysis, a comprehensive search across various electronic databases yielded a total of 1095 potentially relevant articles. To streamline this collection, a duplicate removal algorithm was applied, ensuring that each study was represented only once in our dataset. This was followed by a rigorous screening of titles and abstracts, guided by well-defined inclusion and exclusion criteria. These criteria encompassed various aspects such as study design, demographic characteristics of participants, clinical outcomes measured, and the quality of research methods. This preliminary screening resulted in the identification of 33 articles for a more detailed evaluation. Each of these articles underwent an independent and thorough full-text review by multiple investigators, aimed at ensuring an unbiased and comprehensive assessment. During this phase, 28 articles were excluded for several reasons, specifically: 9 were review articles, 5 were sequentially published works, 8 lacked sufficient data for analysis, and 6 were clinical trials without control groups. Ultimately, 5 articles met the rigorous standards set forth in our research protocol and were selected for inclusion in the final meta-analysis.16-20 This process and the resultant selection are depicted in Figure 1.
3.2 Study characteristics of meta-analysis
The included studies in this meta-analysis, spanning from 2020 to 2022, examined the comparative effectiveness of PENGB and FICB in postoperative wound pain management for hip fracture surgery. A total of five studies were analysed, with sample sizes ranging from 20 to 56 participants per group. The age of participants across these studies varied, with means in both treatment and control groups generally within the elderly age range. In terms of anaesthesia methods used, SA was predominant, employed in four out of the five studies, while GA was used in one study. The concentration and volume of Ropivacaine used in the PENGB groups varied, with doses ranging from 0.25% to 0.5% and volumes between 10 and 30 mL. Similarly, the FICB groups across the studies received Ropivacaine or Adrenaline Levobupivacaine in varying concentrations and volumes, demonstrating a range of approaches within the control groups (Table 1).
| Study | Year | Age (PENGB/FICB) | Sample size (PENGB/FICB) | Anaesthesia Method | PENGB group | FICB group |
|---|---|---|---|---|---|---|
| HUA et al. | 2022 | 74 ± 7/74 ± 8 | 24/24 | SA | 0.4% Ropivacaine 20 mL | 0.4% Ropivacaine 30 mL |
| Li Dan et al. | 2021 | 70.49 ± 2.13/70.23 ± 2.87 | 56/56 | GA | 0.5% Ropivacaine 10 mL | 0.5% Ropivacaine 10 mL |
| ALISTE et al. | 2021 | 56.8 ± 13.0/59.6 ± 9.2 | 20/20 | SA | 0.5% Adrenaline Levobupivacaine 20 mL | 0.25% Adrenaline Levobupivacaine 40 mL |
| Cui Mingzhu et al. | 2020 | 74 ± 8/78 ± 8 | 25/25 | SA | 0.4% Ropivacaine 20 mL | 0.4% Ropivacaine 30 mL |
| Xie Yingchao et al. | 2020 | 67.3 ± 16.5/67.9 ± 13.8 | 21/21 | SA | 0.25% Ropivacaine 30 mL | 0.25% Ropivacaine 30 mL |
- Abbreviations: FICB, Fascia Iliaca Compartment Block; GA, general anaesthesia; PENGB, Pericapsular Nerve Group Block; SA, spinal anaesthesia.
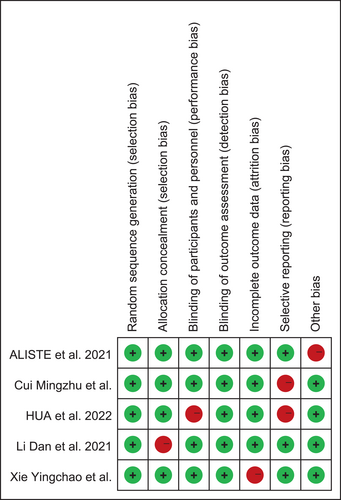
3.3 Results of quality assessment
The overall results indicated a mixed level of bias risk among the studies. Random sequence generation was generally well-handled across most studies, suggesting a low risk of bias in this domain. Allocation concealment was adequately addressed, although some studies presented an unclear risk, indicating potential variability in the methodology. Participant and personnel blinding varied, with several studies showing a high risk, reflecting challenges in maintaining double-blind conditions. Outcome assessment blinding was another area of concern, with multiple studies demonstrating a high risk of detection bias. Regarding the domain of incomplete outcome data, most studies were judged to have a low risk of attrition bias, indicating robustness in handling and reporting of study dropouts or missing data. Selective reporting of outcomes was generally well-managed, although some concerns were noted, suggesting the possibility of reporting bias in a few studies. Finally, the assessment of other potential sources of bias revealed that some studies may be subject to biases not covered by the other domains, warranting a cautious interpretation of these results (Figure 2).
3.4 Meta-analysis comparing the efficacy of pericapsular nerve group block and fascia iliac compartment block.
The meta-analysis evaluated the efficacy of PENGB in the management of perioperative analgesia in patients undergoing THA. The analysis included a total of 4 studies assessing postoperative pain scores, 3 studies examining postoperative opioid consumption, and the incidence of PONV, as well as 2 studies evaluating the incidence of quadriceps muscle weakness. Results indicated moderate heterogeneity in postoperative pain scores (I2 = 59%) and a mean difference (MD) of 0.06, which was not statistically significant (95% CI: −0.36, 0.51; p = 0.69), suggesting that PENGB might not significantly reduce pain scores compared to FICB interventions. Opioid consumption postoperatively also showed low heterogeneity (I2 = 28%) with an MD of −0.25 (95% CI: −0.70, 0.13; p = 0.26), indicating a non-significant reduction in opioid usage. The incidence of PONV had low heterogeneity (I2 = 26%) with a relative risk (RR) of 1.36 (95% CI: 0.43, 2.65; p = 0.51), showing no significant difference between PENGB and FICB groups. Notably, the incidence of quadriceps muscle weakness was significantly lower in the PENGB group (RR = 0.12, 95% CI: 0.06, 0.61; p < 0.05), with no detected heterogeneity (I2 = 0%), highlighting a potential advantage of PENGB in preserving motor function (Table 2).
| Outcome measure | Studies included | Heterogeneity (I2, %) | Meta-analysis effect value (95% CI) | p-value |
|---|---|---|---|---|
| Postoperative pain scores | 4 | 59 | MD = 0.06 (−0.36, 0.51) | 0.69 |
| Postoperative opioid consumption | 3 | 28 | MD = −0.25 (−0.70, 0.13) | 0.26 |
| Postoperative nausea and vomiting incidence | 3 | 26 | RR = 1.36 (0.43, 2.65) | 0.51 |
| Incidence of quadriceps muscle weakness | 2 | 0 | RR = 0.12 (0.06, 0.61) | <0.05 |
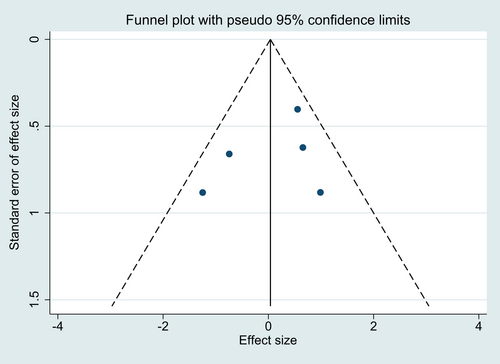
3.5 Assessment of publication bias in meta-analysis
In evaluating publication bias within our meta-analysis, funnel plots were generated for the aggregated data from the included studies. Visual inspection of these plots revealed symmetry, suggesting the absence of publication bias. This symmetry implies that smaller studies with less significant results are as likely to be published as larger studies with more significant outcomes (Figure 3). Further quantitative assessment using Egger's linear regression test corroborated the visual findings, indicating no significant publication bias across the different variables analysed (p > 0.05).
4 DISCUSSION
Hip fractures are a pressing healthcare issue, particularly in the geriatric population, where they are often associated with high morbidity and mortality rates. They pose significant challenges in terms of medical management and healthcare resources.21 Surgery, predominantly in the form of THA, stands as the cornerstone of treatment for these fractures, offering the prospect of pain relief and the restoration of mobility. However, the postoperative period is frequently complicated by substantial pain, which can impede early mobilization and rehabilitation, key factors in the recovery process.22, 23 In addressing this postoperative pain, two regional anaesthesia techniques, the PENGB and the FICB, have gained attention. PENGB targets the nerve supply around the hip joint, offering the potential for effective pain control without significant motor blockade. In contrast, FICB, while also providing pain relief, has been associated with motor weakness, which may delay postoperative functional recovery. The present study adds to the existing literature by providing a comparative analysis of these two techniques.24, 25 It showcases the novelty of PENGB, particularly its association with lower incidences of quadriceps muscle weakness, underlining its clinical value. This insight could steer clinicians towards more refined pain management protocols, optimizing patient outcomes in the context of hip fracture surgery.
The results of this comprehensive meta-analysis provide nuanced insights into the perioperative management of patients undergoing THA with the use of PENGB. While PENGB's impact on postoperative pain scores and opioid consumption was not significantly favourable, its association with a reduced incidence of quadriceps muscle weakness is noteworthy. This particular outcome has considerable clinical implications as it underlines the potential of PENGB to facilitate early postoperative mobilization.26 Early mobilization is critical in orthopaedic surgeries as it not only contributes to enhanced functional recovery but also minimizes the risk of postoperative complications such as deep vein thrombosis and pulmonary embolism. Quadriceps muscle strength is essential for basic activities like walking and standing from a seated position.27 By preserving this strength, PENGB may reduce the duration of hospital stays and improve overall recovery times, thereby enhancing patient outcomes and reducing healthcare costs. The significant reduction in quadriceps muscle weakness aligns with PENGB's mechanism of action, which provides targeted analgesia without extensive motor blockade.
The lack of significant reduction in pain scores and opioid consumption warrants further discussion. Pain management is a multifactorial issue, with a myriad of factors influencing its perception and treatment efficacy. The variability in individual response to nerve blocks can be attributed to genetic factors, psychological state, and previous exposure to pain, which may affect the efficacy of regional anaesthesia. Additionally, the analgesic regimen used postoperatively, including the choice and timing of analgesic administration, could also influence the overall pain experience and opioid requirements. The baseline pain thresholds of patients, which vary widely, may also affect the perceived intensity of pain and, consequently, the reported effectiveness of pain interventions.28 Despite the lack of significant findings in pain reduction, the consistency of outcomes across studies, as indicated by the low heterogeneity, strengthens the reliability of these results. It suggests that although individual studies may vary in design and execution, the overall trend remains stable. The observation that PENGB does not increase the risk of PONV is particularly encouraging. PONV is a significant contributor to patient discomfort and dissatisfaction post-surgery, and its management is a critical component of postoperative care. The ability of PENGB to avoid exacerbating this risk suggests it is a safe alternative to other analgesic techniques that may have higher associated risks of PONV.
Our meta-analysis suggests using PENGB for hip fracture surgeries in patients needing motor function preservation, especially the elderly or those requiring early mobility. While PENGB and FICB show similar efficacy in pain and opioid use, FICB is a viable alternative when PENGB resources or expertise are lacking. Clinical decisions should balance PENGB's benefits in motor function against FICB's ease of use, considering patient-specific factors like age and comorbidities. This evidence-based guidance aids in selecting the most suitable pain management technique for individual patient needs in hip fracture surgeries.
Given our findings of lower quadriceps muscle weakness with PENGB, we recommend its use for patients needing motor function preservation, particularly the elderly and those requiring quick post-surgery mobilization. While PENGB and FICB showed no significant difference in pain and opioid use, FICB remains suitable where PENGB is unavailable or less familiar to practitioners. A patient-centred approach, considering age, comorbidities, and surgical specifics, is advisable in selecting between PENGB and FICB. Healthcare professionals should receive training in PENGB, a newer technique, to enhance its application. Continued research is essential to monitor long-term effects and update clinical guidelines. These recommendations aim to optimize patient outcomes, aligning pain management with overall recovery.
The heterogeneity observed in the meta-analysis could stem from several sources. Variations in study design, such as differences in the size and demographics of patient populations, can contribute significantly. Additionally, the exact technique and dosage of the nerve blocks, as well as the timing of their administration, might vary across studies. Postoperative care protocols, including additional analgesic use, rehabilitation regimens, and patient-reported outcome measures, can also introduce variability. Finally, the skill and experience of the practitioner performing the nerve block may affect efficacy and, consequently, the heterogeneity of the results. Identifying and understanding these sources is crucial for interpreting the meta-analysis and applying its findings to clinical practice. This meta-analysis has several limitations. Firstly, the small number of studies included may not provide a comprehensive view of the available evidence. Secondly, potential variations in the technical execution of PENGB and FICB, as well as differences in analgesic adjuncts used across studies, may influence outcomes. Finally, publication bias, despite not being detected, cannot be entirely ruled out due to the limited scope of the literature search.
5 CONCLUSIONS
In conclusion, compared to FICB, PENGB demonstrates comparable efficacy in reducing opioid consumption and managing postoperative pain and PONV rates. Crucially, PENGB offers a distinct clinical advantage by significantly decreasing the incidence of postoperative quadriceps muscle weakness, thereby preserving motor function, which is essential for patient recovery and rehabilitation following surgery.
ACKNOWLEDGEMENTS
Thank my colleagues for their participation.
FUNDING INFORMATION
None.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.