RETRACTED: The outcome of prolonged postoperative antibiotics on wound healing in orthognathic surgery: A meta-analysis
Abstract
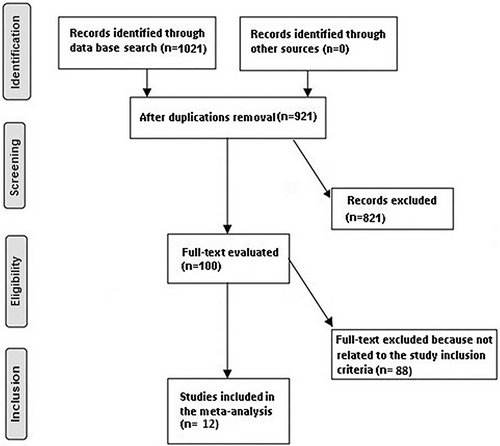
We conducted a meta-analysis to assess the outcome of prolonged postoperative antibiotics (PA) on wound healing in orthognathic surgery (OS). A systematic literature search up to January 2023 was performed and 1021 related studies were evaluated. The chosen studies comprised 1057 OS subjects who participated in the selected studies' baseline, 446 of them used short-term PA, and 611 used long-term PA. Odds ratio (OR) with 95% confidence intervals (CIs) were calculated to assess the effect of prolonged PA on wound infection after OS by the dichotomous methods with a random or fixed effect model. The short-term PA resulted in significantly higher wound infection (OR, 4.27; 95% CI, 2.97–6.14, P < 0.001) with low heterogeneity (I2 = 27%) compared to the long-term PA in OS. The short-term PA resulted in significantly higher wound infection compared to the long-term PA in OS. Though care should be taken when dealing with the results since a large number of the selected studies had <100 subjects as a sample size.
1 INTRODUCTION
The most popular method for treating inherited and acquired dentofacial abnormalities is orthognathic surgery (OS). Although many advantages, such as improved mastication1 and facial aesthetics,2 have been noted, there have also been many documented problems.3 Complications can include wound infection, sinusitis, deviated nasal septum, fever and edema, and nerve transection. In the literature, postoperative infection rates, which range from 1.4% to 33.4%, are the most frequent complication.4 It is debatable whether prophylactic antibiotics should be used during OS. The use of prophylactic antibiotics in OS has been the subject of numerous research that have been described in the literature. In their 1976 research of 98 patients, Peterson and Booth showed virtually little advantage to utilising antibiotic prophylaxis.4 They claimed that antibiotic prophylaxis is not recommended for usage during sagittal osteotomies and is contraindicated during alveolar surgery. On the other hand, Bentley et al. claimed that 5 days would be sufficient coverage and that antibiotic prophylaxis should continue past the immediate postoperative period.5 It has been challenging to develop a normative regimen for postoperative antibiotics (PA) because there are not enough suitable randomised trials. Given the voluntary nature of the treatment and the likelihood that patients will sue, postoperative infections must be prevented at all costs.6 A rigorous quantitative review of randomised controlled trials (RCTs) on the efficiency of PA in OS was the goal of this investigation. This study's main goal was to test the hypothesis of difference against the null hypothesis that there was no difference between short-term (preoperative and perioperative) and long-term (preoperative, perioperative, and postoperative) antibiotics on postoperative wound infection.
2 METHODS
2.1 Eligibility criteria
To create a summary, the studies of the outcome of prolonged PA on wound healing in OS were selected.7
2.2 Information sources
- The study was either a controlled trial, observational, prospective, or retrospective study.
- Patients with OS made up the intended subjects.
- The intervention program included different prolonged PA.
- The study contrasted the outcome of prolonged PA on wound healing in OS.
The excluded studies from consideration were those where the significance of comparison outcomes was not highlighted in the studies, studies that did not examine the effects of prolonged PA on wound infection in OS subjects, and research on OS without prolonged PA.
2.3 Search strategy
A protocol of search approaches was developed following the PICOS concept, and we characterised it as follows: topics for OS, P; Prolonged PA is the “intervention” or “exposure,” whereas the “comparison” was short-term PA compared with a long-term PA; wound infection was the “outcome” and finally, there were no restrictions on the study's design.8
We lead a thorough search of the OVID, Embase, Cochrane Library, PubMed, and Google Scholar databases up until January 2023 using an arrangement of keywords and correlated terms for long-term PA; OS; wound infection; and short-term PA as shown in Table 1. To avoid studies that did not show a relationship between the outcomes of prolonged PA on wound healing in OS, all the papers that had been used were joined into an EndNote file, replicas were eliminated, and the title and abstracts were reviewed, and amended.
| Database | Search strategy |
|---|---|
| Pubmed | #1 “long term postoperative antibiotics” [MeSH Terms] OR “orthognathic surgery”[All Fields] [All Fields] #2 “wound infection”[MeSH Terms] OR “short term postoperative antibiotics”[MeSH Terms] [All Fields] #3 #1 AND #2 |
| Embase | ‘long term postoperative antibiotics’/exp OR ‘orthognathic surgery’ #2 ‘wound infection’/exp OR ‘short term postoperative antibiotics’ #3 #1 AND #2 |
| Cochrane library | (long term postoperative antibiotics): ti, ab, kw (orthognathic surgery): ti, ab, kw (Word variations have been searched) #2 (wound infection): ti, ab, kw OR (short term postoperative antibiotics): ti,ab,kw (Word variations have been searched) #3 #1 AND #2 |
2.4 Selection process
A technique was developed following the epidemiological declaration, which was thereafter arranged and examined in the form of a meta-analysis.
2.5 Data collection process
The criteria used to gather the data included the last name of the primary author, the study period, the publication year, the nation or region, the populace type, the clinical and management physiognomies, the categories, the qualitative and quantitative assessment technique, the information source, the result assessment, and statistical analysis.9
2.6 Data items
When there were disparate findings from a single study founded on the appraisal of the outcome of prolonged PA on wound healing in OS, we independently collected the data.
2.7 Study risk of bias assessment
Two authors individually evaluated the methodology of the designated articles to ascertain the possibility of bias in each study. The methodological quality was evaluated using the “risk of bias instrument” from the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. Each study was sorted according to the appraisal criteria and given one of the three risks of bias itemised below: low: A study was rated as having a low risk of bias if all the quality standards were met; if one or more requirements were not met or were not encompassed, a study was rated as having a moderate risk of bias. The study was measured to have a high risk of bias in the case that one or more quality criteria were not met at all or were only partially met. The original article was revised to remove any inconsistencies.
2.8 Effect measures
Only studies that reported and assessed the outcome of prolonged PA on wound healing in OS were subjected to sensitivity studies. Sensitivity and subclass analysis was utilised to compare the outcome of prolonged PA on wound healing in OS.
2.9 Synthesis methods
The current meta-analysis used a random-or fixed-effect model with dichotomous techniques to compute the odds ratio (OR) with a 95% confidence interval (CI). It was decided to calculate the I2 index, with a range of 0 to 100%. The values around 0%, 25%, 50%, and 75%, respectively, showed no, low, moderate, and high heterogeneity.10 However, additional characteristics that show a high degree of similarity between the included studies were also analysed to confirm the employment of the correct model. The random effect was considered if I2 was 50% or above; if I2 was <50%, the likelihood of employing fixed influence rose.10 A subclass analysis was completed by stratifying the first evaluation based on the previously specified outcome categories. A P-value of 0.05 was used in the analysis to indicate statistical significance for differences across subcategories.
2.10 Reporting bias assessment
Publication bias was assessed both qualitatively and statistically using the Egger regression test and funnel plots that display the logarithm of ORs vs their standard errors (publication bias was considered present if P ≥ 0.05).11
2.11 Certainty assessment
Two-tailed tests were used to analyse all P-values. The graphs and statistical analysis were created using Reviewer Manager Version 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).
3 RESULTS
From a total of 1021 related research that was examined, 12 articles published between 1984 and 2023 that fit the inclusion criteria and were selected and encompassed in the meta-analysis.5, 12-22 Table 2 presents the findings from these studies. 1057 OS subjects who participated in the selected studies' baseline, 446 of them used short-term PA, and 611 used long-term PA. There were 30 to 405 subjects present the trials' sample size.
| Study | Country | Total | Short-term postoperative antibiotics | Long-term postoperative antibiotics |
|---|---|---|---|---|
| Ruggles, 198412 | USA | 40 | 20 | 20 |
| Fridrich, 199413 | USA | 30 | 16 | 14 |
| Bentley, 19995 | Canada | 30 | 15 | 15 |
| Lindeboom, 200314 | Netherlands | 70 | 35 | 35 |
| Baqain, 200415 | UK | 34 | 17 | 17 |
| Jansisyanont, 200816 | Thailand | 122 | 62 | 60 |
| Kang, 200917 | Korea. | 56 | 28 | 28 |
| Danda, 201018 | India | 150 | 75 | 75 |
| Wahab, 201319 | India | 60 | 30 | 30 |
| Zix, 201320 | Switzerland | 60 | 31 | 29 |
| Davis, 201621 | Canada | 405 | 117 | 288 |
| Remschmidt, 202322 | Austria | 99 | 50 | 49 |
| Total | 1057 | 446 | 611 |
The short-term PA resulted in significantly higher wound infection (OR, 4.27; 95% CI, 2.97–6.14, P < 0.001) with low heterogeneity (I2 = 27%) compared to the long-term PA in OS as shown in Figure 2.
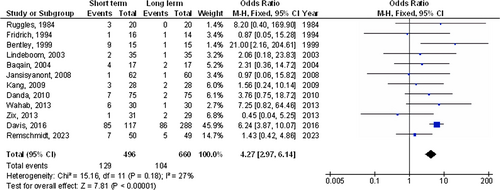
Stratified models could not be utilised to examine the influence of some factors on comparison outcomes, such as gender, age, and ethnicity, due to the lack of data on these variables. No indication of publication bias was found (P = 0.87) after visual analysis of the funnel plot and quantitative assessments using the Egger regression test as shown in Figure 3. The bulk of the included RCTs, however, were found to have subpar methodological quality, no bias in selective reporting, and scant outcome data.

4 DISCUSSION
In the trials used for this meta-analysis, 1057 OS subjects who participated in the selected studies' baseline, 446 of them used short-term PA, and 611 used long-term PA.5, 12-22 The short-term PA resulted in significantly higher wound infection compared to the long-term PA in OS. Though care should be taken when dealing with the results since 9 out of the 12 selected studies had <100 subjects as a sample size.
Orthognathic procedures are considered clean-contaminated procedures, with an average infection rate of 10 to 15%. The use of a superior method and antibiotic prophylaxis, according to Peterson, can lower infection rates to <1%.23 The two tenets of antibiotic prophylaxis are to spread the drug throughout the tissue and bring it to a therapeutic level prior to the surgery, and to keep it there for the shortest time possible following the procedure when there is a risk of infection.24 Preoperative antibiotic prophylaxis has been shown to be successful in achieving the ideal blood level before the surgery.25-27 After OS, Zijderveld et al. evaluated the wound infection rates in 3 groups.25 patients in group I received 2200 mg of intravenous amoxicillin-clavulanic acid25; patients in group II received 1500 mg of intravenous cefuroxime; patients in group III received a placebo. The medicines were administered to all groups 30 minutes before to the surgery. According to the study's findings, individuals who received placebo had infection rates that were greater (52.63%) than those of groups I and II (11.11 and 17.65%, respectively). Due to the lack of a comparison with an extended antibiotic regimen, this study was left out of the meta-analysis. Numerous studies have demonstrated the significance of antibiotic treatment timing. Classen et al.28 observed when antibiotic prophylaxis was administered in a significant number of clean-contaminated procedures. They discovered that the lowest prevalence of wound infection was connected with the administration of antibiotics 2 h prior to surgery. Burke discovered in an animal experiment that the infection rate was not reduced if the antibiotic was given more than 3 h after the bacterial injection.29 However, the length of postoperative antibiotic therapy is still debatable and varies from 1 day to 7 days depending on the study. With the exception of Bentley et al.,5 none of the individual investigations found a substantial increase in the incidence of infection when compared to the control group in either extreme. To decide whether to extend a regimen, one must consider other patient-and procedure-related criteria. Smokers and people with poor oral hygiene and periodontal health may be at higher risk of infection, according to Cheynet and Chossegros.30 Theodossy and Jackson hypothesized that longer surgeries and older patients had statistically higher rates of infection.31 Additionally, it was thought that long surgeries increased the chance of infectious side effects.31 Contrary to these studies, Chow and Singh examined a large number of patients and found no relationship between age and length of surgery and infection problems.32 The microorganisms that are most likely to be connected to the surgical process must be identified in order to choose the proper antimicrobial agent. The majority of oral microorganisms are resistant to penicillin. When it comes to avoiding infection during intraoral surgeries, it is regarded as the antibiotic of first resort. The effectiveness of clindamycin in preventing wound infections was studied by Lindeboom et al. but it was discovered that penicillin-sensitive streptococci were to blame for all three of the infection cases in that investigation.14 Therefore, it is advised that antibiotics from the penicillin family be used in OS. The mandible was where the majority of infections were discovered in this meta-analysis. There are two possible explanations for this. First, compared to the maxilla, the mandible has a lower blood supply. Second, because of gravity, saliva may collect. Saliva contamination of mandibular osteotomy sites can happen up until the third postoperative day.33 The function of local antibacterial agents has not been thoroughly explained. Regardless of allocation, Lindeboom et al. recommended a mouthwash containing 0.12% chlorhexidine for all patients.14 This could be a perplexing element.
This meta-analysis demonstrated the outcome of prolonged PA on wound healing in OS. More research is still needed to clarify these potential connections.34-41 Larger, more homogeneous samples are required for this investigation. This was also emphasised in previous studies that employed a related meta-analysis technique and found comparable results of the effect.42-51
Because our meta-analysis study was unable to determine whether differences in gender, age, and ethnicity are related to the wound infection, well-conducted RCTs are required to evaluate these factors as well as the combination of different gender, ages, ethnicities, and other variants of subjects. In conclusion, the short-term PA resulted in significantly higher wound infection compared to the long-term PA in OS.
5 LIMITATIONS
Because several of the studies included in this meta-analysis study were not encompassed, there may have been selection bias. The removed publications, nevertheless, did not encounter the requirements for inclusion in our meta-analysis. Furthermore, we were unable to determine whether factors such as age, gender, or ethnicity affected the outcomes. The study aims to evaluate the outcome of prolonged PA on wound healing in OS. The incorporation of data from earlier studies could have added bias due to incomplete or inaccurate data. Potential sources of bias included the nutritional status of the participants as well as their age and gender characteristics. Unfortunately, certain unpublished papers and missing data can bias the effect being studied.
6 CONCLUSIONS
The short-term PA resulted in significantly higher wound infection compared to the long-term PA in OS. Though care should be taken when dealing with the results since 9 out of the 12 selected studies had <100 subjects as a sample size.
Open Research
DATA AVAILABILITY STATEMENT
On request, the corresponding author is required to provide access to the meta-analysis database.