RETRACTED: A meta-analysis of the effect of endoscopic submucosal dissection compared with gastrectomy on the wound infection in early stomach cancer subjects
Cheng Sun, and Weilin Liu contributed equally to the manuscript and both are considered frist authors.
Abstract
We conducted a meta-analysis to assess the effect of endoscopic submucosal dissection compared with gastrectomy on the wound infection in early stomach cancer subjects. A systematic literature search up to November 2022 was performed and 2765 related studies were evaluated. The chosen studies comprised 7842 early stomach cancer subjects participated in the selected studies' baseline trials; 3308 of them used the endoscopic submucosal dissection, while 4534 used gastrectomy. Odds ratio (OR) with 95% confidence intervals (CIs) were calculated to assess the wound infection in endoscopic submucosal dissection versus gastrectomy for early stomach cancer by the dichotomous methods with a random or fixed effect model. The use of endoscopic submucosal dissection resulted in significantly lower wound infection (OR, 0.45; 95% CI, 0.34–0.60, P < .001) with no heterogeneity (I2 = 8%) compared with the gastrectomy for early stomach cancer. The use of endoscopic submucosal dissection resulted in significantly lower wound infection compared with the gastrectomy for early stomach cancer. The small sample size of some studies in the comparison calls for care when analysing the results.
1 INTRODUCTION
The third most common cancer fatality (10%) and the fifth most prevalent malignancy are stomach cancers.1, 2 Regardless of lymph node involvement, early stomach cancer is described as carcinoma that is restricted to the mucosa or submucosa. Historically, the sole curative method for treating early stomach cancer was a radical surgical gastrectomy with lymph node dissection.3 Radical surgery, however, has been linked to increased morbidity and mortality as well as a decline in quality of life.4, 5 Endoscopic mucosal resection and endoscopic submucosal dissection are two components of endoscopic resection. For early stomach cancer that was less than 15 mm in size, endoscopic mucosal excision was initially advised.6 The accepted criteria for endoscopic mucosal excision currently include less than 2 cm of well-differentiated or moderately differentiated adenocarcinoma that is restricted to the mucosa and shows no signs of ulceration or lymphovascular invasion.7 The potential for a limited histological examination, particularly if en-bloc resection was not completed, would be the greatest barrier to the widespread adoption of endoscopic mucosal resection in early stomach cancer. To get over the constraints of endoscopic mucosal resection, endoscopic submucosal dissection was developed. By dissecting the submucosal layer with a needle knife during an endoscopic submucosal dissection, a bigger en-bloc resection can be accomplished. When compared with endoscopic mucosal resection, endoscopic submucosal dissection raised the rates of en-bloc, histologically complete, and curative resection while decreasing recurrence.8 The proposed enlarged indication for endoscopic submucosal dissection was put forth by Gotoda et al. in 2001.9 Although numerous studies have compared the effects of endoscopic submucosal dissection with those of surgical treatment for early stomach cancer, their findings have been inconsistent and their patient populations for both procedures have been heterogeneous.10-14 To compare the wound infection rate of endoscopic submucosal dissection compared with gastrectomy in the treatment of early stomach cancer, a systematic review and meta-analysis were carried out.
2 METHOD
2.1 Eligibility criteria
To create a summary, the study of the endoscopic submucosal dissection in comparison to gastrectomy was selected. The analysis of the effect of endoscopic submucosal dissection compared with gastrectomy on the wound infection in early stomach cancer subjects was the major goal of the study.15
2.2 Information sources
- The study was either a controlled trial, observational, prospective, or retrospective study.
- Early stomach cancer patients made up the intended subjects.
- The intervention program included endoscopic submucosal dissection and gastrectomy.
- The study contrasted the effect of endoscopic submucosal dissection compared with gastrectomy on the wound infection in early stomach cancer subjects.
The significance of comparison outcomes was not highlighted in studies, and studies that did not examine the effects of endoscopic submucosal dissection on wound infection in early stomach cancer subjects, and research on early stomach cancer without endoscopic submucosal dissection or gastrectomy were excluded from consideration.
2.3 Search strategy
A protocol of search approaches was developed following the PICOS concept, and we characterised it as follows: topics for early stomach cancer, P; Endoscopic submucosal dissection technique is the ‘intervention’ or ‘exposure’, whereas the ‘comparison’ was endoscopic submucosal dissection compared with gastrectomy; wound infection was the ‘outcome’ and finally there are no restrictions on the study's design.16
We lead a thorough search of the OVID, Embase, Cochrane Library, PubMed, and Google Scholar databases up until November 2022 using an arrangement of keywords and correlated terms for endoscopic submucosal dissection; gastrectomy; early stomach cancer; and wound infection as shown in Table 1. To avoid studies that did not show a relationship between the effect of endoscopic submucosal dissection compared with gastrectomy on the wound infection in early stomach cancer subjects, all the papers that had been used were joined into an EndNote file, replicas were eliminated, and the title and abstracts were reviewed and amended.
| Database | Search strategy |
|---|---|
| Pubmed | #1 ‘endoscopic submucosal dissection’[MeSH Terms] OR ‘early stomach cancer’[All Fields] OR ‘gastrectomy’[All Fields] #2 ‘wound infection’[MeSH Terms] OR ‘endoscopic submucosal dissection’[All Fields] OR ‘gastrectomy’[All Fields] #3 #1 AND #2 |
| Embase | ‘endoscopic submucosal dissection’/exp OR ‘early stomach cancer’/exp OR ‘gastrectomy’ #2 ‘wound infection’/exp OR ‘endoscopic submucosal dissection’/exp OR ‘gastrectomy’ #3 #1 AND #2 |
| Cochrane library | (endoscopic submucosal dissection):ti,ab,kw (early stomach cancer):ti,ab,kw OR (gastrectomy): ti,ab,kw (Word variations have been searched) #2 (wound infection):ti,ab,kw OR (endoscopic submucosal dissection): ti,ab,kw OR (gastrectomy): ti,ab,kw (Word variations have been searched) #3 #1 AND #2 |
2.4 Selection process
A technique was developed following the epidemiological declaration, which was thereafter arranged and examined in the form of a meta-analysis.
2.5 Data collection process
The criteria used to gather the data included the last name of the primary author, the study period, the publication year, the nation or region, the populace type, the clinical and management physiognomies, the categories, the qualitative and quantitative assessment technique, the information source, the result assessment, and statistical analysis.17
2.6 Data items
When there were disparate findings from a single study founded on the appraisal of the effect of endoscopic submucosal dissection compared with gastrectomy on the wound infection in early stomach cancer subjects, we independently collected the data.
2.7 Study risk of bias assessment
The two authors individually evaluated the methodology of the designated articles to ascertain the possibility of bias in each study. The methodological quality was evaluated using the ‘risk of bias instrument’ from the Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. Each study was sorted according to the appraisal criteria and given one of the three risks of bias itemised below: low: A study was rated as having a low risk of bias if all the quality standards were met; if one or more requirements were not met or were not encompassed, a study was rated as having a moderate risk of bias. The study was measured to have a high risk of bias in the case that one or more quality criteria were not met at all or were only partially met. The original article was revised to remove any inconsistencies.
2.8 Effect measures
Only studies that reported and assessed the effect of endoscopic submucosal dissection compared with gastrectomy on the wound infection in early stomach cancer subjects were subjected to sensitivity studies. Sensitivity and subclass analysis were used to compare the effect of endoscopic submucosal dissection compared with gastrectomy on the wound infection in early stomach cancer subjects.
2.9 Synthesis methods
The current meta-analysis used a random- or fixed-effect model with dichotomous techniques to compute the odds ratio (OR) with a 95% confidence interval (CI). It was decided to calculate the I2 index, with a range of 0 to 100%. The values around 0%, 25%, 50%, and 75%, respectively, showed no, low, moderate, and high heterogeneity.18 However, additional characteristics that show a high degree of similarity between the included studies were also analysed to confirm the employment of the correct model. The random effect was considered if I2 was 50% or above; if I2 was less than 50%, the likelihood of employing fixed influence rose.18 A subclass analysis was completed by stratifying the first evaluation based on the previously specified outcome categories. A P-value of 0.05 was used in the analysis to indicate statistical significance for differences across subcategories.
2.10 Reporting bias assessment
Publication bias was assessed both qualitatively and statistically using the Egger regression test and funnel plots that display the logarithm of ORs versus their standard errors (publication bias was considered present if P ≥ .05).19
2.11 Certainty assessment
Two-tailed tests were used to analyse all P-values. The graphs and statistical analysis were created using Reviewer Manager version 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).
3 RESULTS
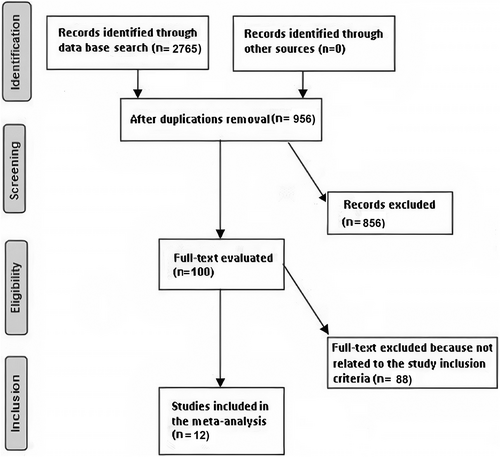
From a total of 2765 related research that was examined, 12 articles published between 2012 and 2022 that fit the inclusion criteria and were encompassed in the meta-analysis were selected.20-31 Table 2 presents the findings from these studies. Seven thousand eight hundred and forty two early stomach cancer subjects participated in the selected studies' baseline trials; 3308 of them used the endoscopic submucosal dissection, while 4534 used gastrectomy. There were 79 to 2065 subjects present when the trials first began.
| Study | Country | Total | Endoscopic submucosal dissection | Gastrectomy |
|---|---|---|---|---|
| Chiu, 201220 | China | 114 | 74 | 40 |
| Park, 201421 | Korea | 225 | 108 | 117 |
| Kim, 201422 | Korea | 158 | 107 | 51 |
| Choi, 201523 | Korea | 375 | 261 | 114 |
| Fukunaga, 201724 | Japan | 308 | 181 | 127 |
| Chang, 201725 | Korea | 153 | 74 | 79 |
| Gong, 201726 | Korea | 79 | 40 | 39 |
| Park, 201827 | Korea | 493 | 111 | 382 |
| Lee, 201828 | Korea | 1823 | 907 | 916 |
| Hahn, 201829 | Korea | 1988 | 786 | 1202 |
| Guo, 202030 | China | 40 | 20 | 20 |
| Kim, 202231 | Korean | 637 | 252 | 385 |
| Total | 7842 | 3308 | 4534 |
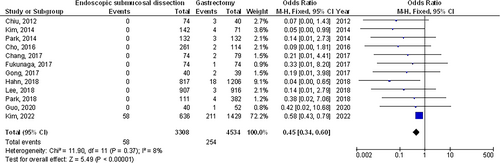
The use of endoscopic submucosal dissection resulted in significantly lower wound infection (OR, 0.45; 95% CI, 0.34–0.60, P < .001) with no heterogeneity (I2 = 8%) compared with the gastrectomy for early stomach cancer as shown in Figure 2.
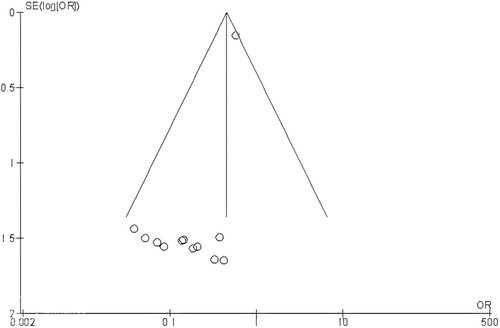
Stratified models could not be used to examine the influence of some factors on comparison outcomes, such as gender, age, and ethnicity, because of the lack of data on these variables. No indication of publication bias was found (P = .88) after visual analysis of the funnel plot and quantitative assessments using the Egger regression test as shown in Figure 3. The bulk of the included randomised controlled trials, however, was found to have subpar methodological quality, no bias in selective reporting, and scant outcome data.
4 DISCUSSION
In the trials used for this meta-analysis, 7842 early stomach cancer subjects participated in the selected studies' baseline trials; 3308 of them used the endoscopic submucosal dissection, while 4534 used gastrectomy.20-31 The use of endoscopic submucosal dissection resulted in significantly lower wound infection compared with the gastrectomy for early stomach cancer. The small sample size of some studies (2 out of 12 were less than 100 subjects) in the comparison calls for care when analysing the results.
Following gastrectomy, there is a greater prevalence of wound infections. Most typically, the middle or lower portion of the stomach is where primary early gastric malignancies first appear.
Total adverse events happened less often in endoscopic submucosal dissection subjects than gastrectomy, thus shorter hospital stays, less trauma, and better quality of life were gained in endoscopic submucosal dissection subjects. In addition, endoscopic submucosal dissection was related to less expensive cost. The most frequent problems in endoscopic submucosal dissection subjects were bleeding and perforation.32 In most cases, although, these advert events can be effectively treated under endoscopic therapy. Otherwise, further surgery would be applied. With a distal gastrectomy, the entire high-risk section of the stomach is removed, leaving just the lower-risk portion. Additionally, endoscopic submucosal dissection enables the persistence of intestinal metaplasia and atrophic gastritis in the remaining mucosa after the procedure.33 Also, endoscopic submucosal dissection is less intrusive than surgery, leading to a superior quality of life. Therefore, if metachronous lesions are found early and removed, the increased quality of life with endoscopic submucosal dissection over surgery may offset the minor risk of those lesions. Bleeding and perforation are the primary endoscopic submucosal dissection consequences, and both can be effectively treated intraprocedural in skilled hands.34 However, anastomotic leakage, intestinal obstruction, and anastomotic stricture are among the surgical complications that frequently have a considerably greater influence on patients' quality of life, length of hospital stay, and mortality.35, 36
This meta-analysis demonstrated how endoscopic submucosal dissection and gastrectomy for early stomach cancer introduce wound infection. More research is still needed to clarify these potential connections and compare the wound infection in endoscopic submucosal dissection and gastrectomy for early stomach cancer. Larger, more homogeneous samples are required for this investigation. This was also emphasised in a previous study that employed a related meta-analysis technique and found comparable wound infection in endoscopic submucosal dissection and gastrectomy for early stomach cancer.32 Because our meta-analysis study was unable to determine whether differences in gender, age, and ethnicity are related to the wound infection, well-conducted randomised controlled trials are required to evaluate these factors as well as the combination of different gender, ages, ethnicities, and other variants of subjects. In conclusion, the use of endoscopic submucosal dissection resulted in significantly lower wound infection compared with the gastrectomy for early stomach cancer.
5 LIMITATIONS
Because several of the studies included in this meta-analysis study were not encompassed, there may have been selection bias. The removed publications, nevertheless, did not encounter the requirements for inclusion in our meta-analysis. Two out of 12 studies had a low sample size (less than 100 subjects). Furthermore, we were unable to determine whether factors such as age, gender, or ethnicity affected the outcomes. The study aims to compare the wound infection in endoscopic submucosal dissection versus gastrectomy for early stomach cancer. The incorporation of data from earlier studies could have added bias because of incomplete or inaccurate data. Potential sources of bias included the nutritional status of the participants as well as their age and gender characteristics. Unfortunately, certain unpublished papers and missing data can bias the effect being studied.
6 CONCLUSIONS
The use of endoscopic submucosal dissection resulted in significantly lower wound infection compared with the gastrectomy for early stomach cancer. The small sample size of some studies in the comparison calls for care when analysing the results.
Open Research
DATA AVAILABILITY STATEMENT
On request, the corresponding author is required to provide access to the meta-analysis database.