Surgical site infections in thyroid and parathyroid surgery in Japan: An analysis of the Japan Nosocomial Infections Surveillance database from 2013 to 2020
Abstract
Surgical site infections (SSIs) after thyroid surgery are rare complications, with incidence rates of 0.3%–1.6%. Using a Japanese database, we conducted exploratory analyses on the incidence of SSIs, investigated the incidence of SSIs by the National Nosocomial Infections Surveillance risk index, and identified the causative bacteria of SSIs. SSIs occurred in 50 (0.7%) of 7388 thyroid surgery cases. Risk index-0 patients had the lowest incidence rate of SSIs (0.41%). The incidence of SSIs in risk index-1 patients was 3.05 times the incidence of SSIs in risk index-0 patients. The rate of SSI occurrence for risk index-2 patients was 4.22 times the rate of SSI occurrence for risk index-0 patients. Thirty-one bacterial species were identified as the cause of SSIs in thyroid surgery cases, of which 12 (38.7%) SSIs were caused by Staphylococcus aureus and Staphylococcus epidermidis. Of the nine SSIs caused by Staphylococcus aureus, 55.6% (five cases) were attributed to methicillin-resistant Staphylococcus aureus. Therefore, routine prophylactic antibiotic administration should be avoided, while the target for administration should be narrowed, according to the SSI risk. Administration of prophylactic antibiotics, such as 2 g piperacillin or 1 g cefazolin, is considered appropriate.
1 INTRODUCTION
Safe medical practice is the most important aspect of surgical treatment. In terms of medical safety management, surgeons are required to not only explain the procedure but also explain and record the frequency of surgical complications and their countermeasures.1, 2 This is also important in terms of shared decision making between patients and health care providers.3 For example, in thyroid surgery, postoperative haemorrhage, hypoparathyroidism and recurrent laryngeal nerve palsy are well-known complications, with several studies reporting on their frequency, countermeasures and treatment.4-12 However, less frequent and rare complications, such as surgical site infections (SSIs) in thyroid surgery, are only reported in terms of their frequency, which is approximately 0.3%–1.6%.4, 6, 8 Thyroid surgery is considered a clean procedure with a very low incidence of SSIs. The presence of SSIs due to thyroid surgery is a rare complication, and there are no detailed reports on it from Japan.
In contrast, SSIs are associated with increased morbidity and mortality, increased length of hospital stay, higher readmission rates and increased hospital costs. They are now the most common and costly of all hospital-acquired infections, accounting for 20% of these.13 Treatment of infected wounds typically includes debridement, antibiotics, dressings, continuous irrigation suction systems, closed-suction irrigation systems or negative-pressure wound therapy.14 On an average, SSIs extend the hospital length of stay by 9.7 days for treatment.13 The incidence rate of SSIs varies according to the operative procedure and is reported to be 2%–5%.13 Compared with the incidence of SSIs from various surgical procedures, the incidence of SSIs in thyroid surgery appears to be low. However, as the thyroid gland is located in the neck, which is in proximity to critical structures, SSI is an extremely serious medical condition once it occurs and becomes severe enough to require treatment for infected wounds, such as debridement. Therefore, thyroid surgeons need to know the preventive measures for thyroid surgery-induced SSIs, which, despite their rarity, can be difficult to treat once they occur and become severe.
Prophylactic antibiotic therapy is often used to prevent SSIs. However, as thyroid surgery is a clean procedure, routine antibiotic prophylaxis is not recommended by most international standards.15 Despite these principles, the use of antibiotic prophylaxis in thyroid surgery remains controversial. Practice patterns among thyroid surgeons present drastic variations, with 62% of surgeons reporting that they “almost never” use prophylactic antibiotics and 26% of surgeons reporting that they “almost always” use prophylactic antibiotics.16 We also administered prophylactic antibiotics during thyroid surgery to prevent an SSI.
As it was previously stated, SSIs from thyroid surgery are rare complications with no detailed reports of them coming from Japan; therefore, we conducted an exploratory study using the Japanese government database. We conducted three analyses in this study: (1) analysis of the incidence of SSIs due to thyroid surgery in Japan, (2) analysis of the incidence rate of SSIs due to thyroid surgery by risk, and (3) analysis of the causative bacteria of SSIs in thyroid surgery.
This study aimed to propose a method to prevent SSIs in line with the current status of SSIs in thyroid surgery in Japan.
2 MATERIALS AND METHODS
2.1 Definition of SSI
An SSI occurs after surgery in the part of the body that was operated on, typically within 30 days of surgery. We adopted the US Centers for Disease Control and Prevention (CDC) criteria. The CDC describes three types of SSIs: superficial incisional SSI (this infection occurs in the area of the skin where the incision was made), deep incisional SSI (this infection occurs beneath the incision area, in the muscle and tissues surrounding the muscles) and organ or space SSI (this type of infection can occur in any area of the body other than the skin, muscle and surrounding tissues involved in the surgery—this includes a body organ or the space between organs).15
2.2 Japan Nosocomial Infections Surveillance (JANIS) database
JANIS is a national surveillance program organised by the Ministry of Health, Labour and Welfare of Japan, which was designed to provide basic information on the incidence and prevalence of nosocomial infections and antimicrobial-resistant bacteria in Japanese medical settings. It is one of the largest national programs on antimicrobial resistance surveillance in the world. JANIS was launched in 2000 with three divisions: the clinical laboratory division, antimicrobial-resistant bacterial infection division and intensive care unit division. Subsequently, two more divisions, SSI and neonatal intensive care unit, were added in 2002.17, 18
The JANIS-SSI database was established to continuously collect and analyse data on the incidence of post-SSIs by risk factors and their causative organisms and to clarify the incidence of SSIs in health care organisations. The database comprehensively contains SSI occurrences in a total of 49 surgical procedures: 4 general surgical procedures including thyroid and parathyroid surgery, 15 gastrointestinal surgical procedures, 13 cardiovascular surgical procedures, 7 orthopaedic surgical procedures, 2 neurosurgical procedures, 4 gynaecological procedures, 3 urological procedures and 1 head and neck surgery procedure. The database contains patient ID, age, sex, surgical procedure, date of surgery, duration of surgery, wound classification defined by the National Nosocomial Infections Surveillance (NNIS) issued in October 2004,16 American Society of Anesthesiologists (ASA) score, emergency surgery, implantation, endoscopic use, colostomy and SSI details (date of SSI diagnosis, specific site of infection, specimen, isolated pathogen) for these surgical cases.
2.3 Database and statistical analyses
The time interval examined spans from 2013 to 2020. We identified 48 surgical procedures and thyroid and parathyroid surgeries (hereinafter referred to as thyroid surgeries), for a total of 49 surgical procedures, in the JANIS-SSI database. All SSIs identified in the database were examined: superficial, deep and internal organ/body cavity infections. We conducted an exploratory study of annual trends in the incidence of SSI.
Our hypothesis was that the incidence of SSI increases with risk. We examined the occurrence of SSIs using the NNIS System Report risk categories. The risk index (RI) was scored against three risk categories: ASA physical status classification, wound classification and operative time for the surgical procedure. An ASA physical status classification ranges from 1 to 6, with ASA 1 and 2 cases (a normal healthy patient and a patient with mild systemic disease, respectively) given a score of 0 points, and patients with a physical condition worse than ASA 3 (a patient with severe systemic disease) given a score of 1 point. In the wound classification system, I (clean) and II (clean/contaminated) were scored 0, while III (contaminated) and IV (dirty) were scored 1 point. The duration of surgery in the 75th percentile or above was given a score of 1 point for the risk of surgery time.19-21 The scores for these three risk categories were summed to define an RI of 0–3. We calculated risk ratios for each risk category using the incidence of SSIs in the group of patients at no risk (RI-0) as a reference. As routine thyroid surgery is a clean procedure, RI-1 in our study was defined as ASA physical status category 3 (a patient with severe systemic disease) or the duration of surgery in the 75th percentile or above. RI-2 was defined as ASA physical status category 3 (a patient with severe systemic disease) and the duration of surgery in the 75th percentile or above.
Finally, we analysed the results of the culture tests in SSI cases occurring during thyroid surgery. We developed a ranking of the number of culture tests performed, the number of bacteria isolated and the top five SSI-causing bacteria in cases where SSIs occurred each year. Then, drug options for prophylactic antibiotic administration were considered based on the results of the culture tests.
3 RESULTS
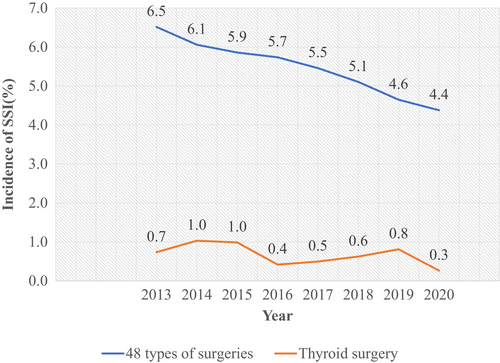
We summarised the JANIS-SSI database from 2013 to 2020 in Table 1. Overall, 2 090 123 cases were analysed, of which 7388 were thyroid surgery cases. There were 2 082 735 patients who underwent 48 surgical procedures, excluding thyroid surgery, of whom 111 655 (5.4%) had SSIs. In thyroid surgery cases, SSIs occurred in 50 (0.7%) of 7388 cases. We investigated the occurrence of SSIs using different surgical techniques (traditional open vs. endoscopic) in thyroid surgery. No SSIs due to thyroid endoscopic surgery were reported. Conversely, 50 cases of SSIs due to thyroid surgery were reported, of which 46 (95.8%) were caused by superficial incisional wounds. Furthermore, two (3.9%) were deep incisional SSIs and two (3.9%) were SSIs extending into the internal organs or body cavity. Since 2016, there have been no reports of SSIs involving deep incisional wounds or internal organs/body cavities.
| Year | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | Total | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 48 types of surgery | Number of 48 types of surgeries | 160 259 | 206 370 | 250 817 | 273 176 | 291 021 | 304 995 | 306 065 | 290 032 | 2 082 735 | |
| Number of SSI | 10 439 | 12 499 | 14 691 | 15 670 | 15 884 | 15 560 | 14 218 | 12 694 | 111 655 | ||
| Incidence of SSI (%) | 6.5 | 6.1 | 5.9 | 5.7 | 5.5 | 5.1 | 4.6 | 4.4 | 5.4 | ||
| Thyroid surgeries | Number of types of surgery | 818 | 874 | 1015 | 956 | 1010 | 965 | 987 | 763 | 7388 | |
| Number of SSI occurrences by types of surgery | 6 | 9 | 10 | 4 | 5 | 6 | 8 | 2 | 50 | ||
| Incidence of SSI by thyroid surgery (%) | 0.7 | 1.0 | 1.0 | 0.4 | 0.5 | 0.6 | 0.8 | 0.3 | 0.7 | ||
| Number of SSI occurrences by depth | Superficial incision wound | 5 | 7 | 9 | 4 | 5 | 6 | 8 | 2 | 46 | |
| Deep incision wound | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | ||
| Internal organs/body cavity | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 2 | ||
- Note: SSI, surgical site infection.
The annual trends in the incidence of SSIs over the 8-year period from 2013 to 2020 are shown in Figure 1. The incidence of SSIs in thyroid surgery ranged from 0.3% to 1%. In contrast, the proportion of SSIs for the other 48 surgical procedures showed a downward trend over the years, decreasing by approximately 2%, from 6.5% in 2013 to 4.4% in 2020.
We examined the incidence of SSIs using RI (Table 2). Of the 7388 cases of thyroid surgeries performed during the aforementioned 8-year period, 5131 (69.5%) had RI-0, 2084 (28.2%) had RI-1 and 173 (2.3%) had RI-2. There were no cases with RI-3; therefore, RI-3 cases were excluded from the present study. We confirmed that the higher the RI, the greater the proportion of SSI occurrence. RI-0 had the lowest SSI incidence (0.41%), while RI-1 had an SSI risk that was 3.05 times higher (1.25%). Furthermore, the rate of SSI occurrence for RI-2 was found to be 1.73%, which is 4.22 times the rate of SSI occurrence for RI-0.
| Year | Total number of thyroid surgeries | RI-0 | RI-1 | RI-2 | RI-3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of thyroid surgeries | Number of SSI occurrences | Incidence of SSI (%) | Number of thyroid surgeries | Number of SSI occurrences | Incidence of SSI (%) | Number of thyroid surgeries | Number of SSI occurrences | Incidence of SSI (%) | Number of thyroid surgeries | Number of SSI occurrences | Incidence of SSI (%) | ||
| 2013 | 818 | 582 | 1 | 0.2 | 223 | 5 | 2.2 | 13 | 0 | 0.0 | 0 | - | - |
| 2014 | 874 | 618 | 3 | 0.5 | 237 | 6 | 2.5 | 19 | 0 | 0.0 | 0 | - | - |
| 2015 | 1015 | 712 | 2 | 0.3 | 284 | 7 | 2.5 | 19 | 1 | 5.3 | 0 | - | - |
| 2016 | 956 | 663 | 2 | 0.3 | 277 | 2 | 0.7 | 16 | 0 | 0.0 | 0 | - | - |
| 2017 | 1010 | 706 | 3 | 0.4 | 286 | 2 | 0.7 | 18 | 0 | 0.0 | 0 | - | - |
| 2018 | 965 | 660 | 5 | 0.8 | 281 | 0 | 0.0 | 24 | 1 | 4.2 | 0 | - | - |
| 2019 | 987 | 673 | 5 | 0.7 | 275 | 3 | 1.1 | 39 | 0 | 0.0 | 0 | - | - |
| 2020 | 763 | 517 | 0 | 0.0 | 221 | 1 | 0.5 | 25 | 1 | 4.0 | 0 | - | - |
| Total | 7388 | 5131 | 21 | 0.41 | 2084 | 26 | 1.25 | 173 | 3 | 1.73 | 0 | - | - |
| Risk ratio | - | - | - | 1 | - | - | 3.05 | - | - | 4.22 | - | - | - |
- Abbreviations: RI, risk index; SSI, surgical site infection.
Details of causative bacteria in thyroid surgery SSIs are shown in Table 3. Culture tests were performed on 21 patients (42%). We found that Staphylococcus aureus was the most commonly reported bacterium causing SSIs in thyroid surgery; this goes in line with reports from five of eight years since 2013. We identified 31 bacterial species that could be causing SSIs in thyroid surgery, of which 12 (38.7%) were Staphylococcus aureus and Staphylococcus epidermidis. Of the nine SSI cases caused by Staphylococcus aureus, 55.6% (five cases) were due to methicillin-resistant Staphylococcus aureus (MRSA). After Staphylococcus, Streptococcus was the second most common causative organism of SSIs in thyroid surgery. Seven (22.6%) were Streptococcus spp., of which three (9.7%) were Propionibacteria and two (6.5%) were Corynebacteria.
| Year | Number of SSI occurrences | Number of culture tests performed | Number of bacteria identified | SSI cause bacterium Upper 3 types | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | Number of bacteria identified | 2 | Number of bacteria identified | 3 | Number of bacteria identified | ||||
| 2013 | 6 | 1 | 2 | Escherichia coli | 1 | Klebsiella pneumoniae | 1 | ||
| 2014 | 9 | 4 | 7 | Staphylococcus aureusa | 2 (1) | Staphylococcus epidermidis | 2 | Corynebacterium spp. | 1 |
| 2015 | 10 | 4 | 6 | Staphylococcus aureusa | 2 (1) | Streptococcus spp. | 2 | Clostridium spp. | 1 |
| 2016 | 4 | 1 | 2 | Streptococcus spp. | 1 | Staphylococcus epidermidis | 1 | ||
| 2017 | 5 | 1 | 4 | Streptococcus spp. | 2 | Staphylococcus aureusa | 1(1) | Escherichia coli | 1 |
| 2018 | 6 | 5 | 5 | Staphylococcus aureusa | 2 (1) | Streptococcus spp. | 2 | Propionibacterium sp. | 1 |
| 2019 | 8 | 4 | 4 | Staphylococcus aureusa | 1 (0) | Corynebacterium spp. | 1 | Gram-negative bacilli | 1 |
| 2020 | 2 | 1 | 1 | Staphylococcus aureusa | 1 (1) | ||||
| Total | 50 | 21 | 31 | ||||||
- a Methicillin-resistant Staphylococcus aureus (MRSA) is listed in parentheses.
4 DISCUSSION
We first analysed the current occurrence of SSIs from various surgical procedures in Japan and the characteristics of SSIs during thyroid surgery. The incidence rate of SSIs for thyroid surgery over an 8-year period was 0.7%, in consistency with the results of previous studies.4, 6, 8 We examined the difference in the incidence of SSIs between 48 common surgical procedures and thyroid surgery in Japan using a chi-square test and found that thyroid surgery caused fewer SSIs than other common surgical procedures, with a statistically significant difference. Thyroid surgery is considered a clean procedure in well-vascularised areas that have no contact with the upper aerodigestive tract, such as the trachea, larynx, pharynx and oesophagus. In addition, 95.8% of SSIs were superficial incisional wounds because the thyroid gland is an anatomically superficial organ. Bures et al also reported that 93.8% of SSIs due to thyroid surgery were caused by superficial incisional wounds, which is consistent with the results of our study.22
We subsequently showed that the incidence of SSIs in thyroid surgery is three to four times higher with an increased risk. In the JANIS-SSI database, a score of 1 point is assigned if the overall condition is worse than ASA 3 in the ASA physical condition classification. For example, patients classified with ASA 3 have substantive functional limitations and one or more moderate-to-severe diseases, including poorly controlled diabetes mellitus, hypertension, chronic obstructive pulmonary disease, morbid obesity (body mass index [BMI] ≥40 kg/m2), active hepatitis, alcohol dependence or abuse, implanted pacemaker, moderate reduction of ejection fraction, end-stage renal disease undergoing regularly scheduled dialysis, history (>3 months) of myocardial infarction, cerebral vascular accident, transit ischemic attack and coronary artery disease/stents. Bures et al. also reported that ASA physical status classification and duration of surgery were independent risk factors for SSI occurrence in thyroid surgery.22 Myssiorek et al. reported that age ≥80 years, male sex, BMI of 40–50 kg/m2, current smoking and ventilation within 48 hours preceding surgery are also risk factors.23 Generally, thyroid surgery is a clean procedure, and prophylactic antibiotics are not recommended.24-27 However, we argue that prophylactic antibiotics should also be considered in thyroid surgery, as the incidence of SSI is three to four times higher in patients with a general condition worse than ASA 3 and in those whose operation lasts longer than the duration of surgery in the 75th percentile or above. Myssiorek et al. also established that routine use of antibiotics should not be undertaken in patients undergoing thyroidectomy and should only be considered for high-risk patients or for patients with contaminated wounds.23
As aforementioned, the risk of SSI increases by one level in the RI, as it increases when the operative time exceeds the 75th percentile. In the JANIS-SSI database, the cut-off time for thyroid surgery is based on surgical data from each year of registration. As shown in Table 4, the risk of SSI increased for thyroid surgeries exceeding an average duration of 154.75 min.
| Year | Cut-off surgical time of thyroid surgeries (min) |
|---|---|
| 2013 | 204 |
| 2014 | 185 |
| 2015 | 177 |
| 2017 | 170 |
| 2018 | 165 |
| 2019 | 161 |
| 2020 | 176 |
| Average | 154.8 |
Finally, we examined the causative bacteria of SSIs during thyroid surgery. We reported that Staphylococcus aureus was the most common causative bacterium. Bures et al also reported that 51.8% of the causative bacteria of SSIs after thyroid surgery were Staphylococcus aureus.22 We further reported that 55.6% of the Staphylococcus aureus detected were MRSA. Given that resistant bacteria account for half of all such cases, routine prophylactic antibiotic administration should be avoided. Furthermore, as indicated above, we argue that the target for administration should be narrowed according to the risk of SSI. When considering prophylactic antibiotics in individuals who retain risk factors for the risk of developing SSI in thyroid surgery, antibiotics that cover staphylococci in superficial incisional wounds should be considered. In a randomised controlled trial examining antibiotics to prevent the occurrence of SSIs in thyroid surgery, Urno et al. reported that 2 g piperacillin or 1 g cefazolin could be safely administered.24 We also administered 1 g cefazolin along with prophylactic antibiotics during thyroid surgery.
This study has several limitations. First, the study used the JANIS-SSI database and items not included in the database survey could not be considered. For example, although we showed that the incidence of SSI for thyroid surgery increased with risk, the basis for determining ASA 3 or higher was not included in the database. Second, with respect to the search for bacteria responsible for SSIs in thyroid surgery, culture tests were only performed in 42% of cases of SSI occurrence. Culture testing should be performed to select the appropriate antimicrobial agents.
Despite the limitations of our study, it has a large sample size, covering approximately 2 million cases and more than 7000 thyroid surgeries. In conclusion, thyroid surgery-associated SSIs are extremely rare adverse events, and we have shown that they occur at a rate of 0.7% in Japan. We also showed that prophylactic antibiotics should be administered on a risk-based basis, specifically to patients with a poor general condition (those with ASA 3 or above) and to patients whose operative time exceeds the 75th percentile or above. Continued updating of the database in the future and its analysis will allow preventative measures to be taken for SSIs in thyroid surgery, according to the current situation in Japan.
FUNDING INFORMATION
This research received no external funding.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.