RETRACTED: Impact of negative pressure wound treatment on incidence of surgical site infection in varied orthopedic surgeries: A systematic review and meta-analysis
Registration number: CRD42022360189.
Abstract
Negative pressure wound therapy (NPWT) is a popular treatment to heal infected wounds. This meta-analysis aimed to determine if NPWT was more effective than conventional wound dressings for surgical site infections (SSI) in varied orthopaedic surgeries. Literature was retrieved from seven electronic databases (Medline, Web of Science, PubMed, Embase, Google Scholar, Cochrane Library, and CNKI). Randomised control trials (RCT) and retrospective cohort studies (RS) involving arthroplasty, fracture, and spinal surgery were extracted. SSI was our primary outcome, while total complications and length of hospital stay were secondary outcomes. We carried out the risk of bias assessment and meta-analysis using the Cochrane Risk of Bias 2.0 tool and Stata 17.0. Among the 798 studies retrieved, 18 of them met our inclusion criteria. We identified 13 RCTs and 5 RSs. The results of meta-analysis showed that the incidence of SSI in the NPWT group was significantly lower relative to the control group (OR = 0.60, 95% CI 0.47 to 0.77, P < 0.001). Subgroup analyses revealed that the incidences of SSI involving arthroplasty, fracture, and spinal surgery in the NPWT group accounted for 46%, 69%, and 37% relative to the control group, respectively. The incidence of SSI in RS (OR = 0.27, 95% CI 0.13 to 0.56) was significantly lower than that in RCT (OR = 0.69, 95% CI 0.54 to 0.90) (P = 0.02). Moreover, patients in the NPWT group had a lower total complication rate (OR = 0.51, 95% CI 0.34 to 0.76) and shorter hospital stays (SMD = −0.42, 95% CI −0.83 to −0.02), although high heterogeneity existed. NPWT may be an efficient alternative to help prevent the incidence of SSI and total complications as well as achieved shorten hospital stay in varied orthopaedic surgeries. The rational use of NPWT should be based on the presence of patients' clinical conditions and relevant risk factors.
1 INTRODUCTION
Surgical site infections (SSI) usually cause prolonged hospital stay, readmission, reoperation, and deep prosthetic infections, which not only places a significantly heavy burden on the healthcare system, but also results in substantial morbidity and decreased quality of life.1 Patients with SSI have worse clinical outcomes, like continued pain and slow recovery of function, than otherwsie.2 Patients' basic conditions and operation parameters (for example, surgery type and duration) are well-established risk factors for wound infections in orthopaedic surgery.3 As Patel et al. put it, each day of prolonged wound drainage was associated with a 29% increase in postoperative infection, even higher in obese patients.4
Negative pressure wound therapy (NPWT) has been reported to reduce wound complications including dehiscence, infection, hematoma and seroma.5 The combination of the negative pressure and the foam alters the wound environment, making inflammation modulated, excessive fluid drained, and angiogenesis promoted.5 NPWT was recommended to reduce infection risk and accelerate recovery in patients with cardiothoracic, abdominal, and orthopaedic surgeries.6-9 One of the previous studies conducted a meta-analysis to compare the application of NPWT with standard care in open trauma patients, revealing no significant difference in the proportion of wounds healed at 6 weeks follow-up.10 Another meta-analysis pooled six original studies involving the comparison of NPWT with traditional wound dressings in orthopaedic trauma surgery, discovering lower incidence of deep SSI, superficial SSI, and wound dehiscence.11 However, the evidence about the efficacy of NPWT for decreasing the incidence of SSI in varied orthopaedic surgeries is lacking.
The present study aimed to perform a systematic review and meta-analysis to determine whether NPWT is more effective in reducing incidence of SSI, total complication rate, and length of hospital stay after those surgeries involving arthroplasty, fracture and spinal.
2 METHODS
2.1 Registration
This study is registered on the platform of PROSPERO (CRD42020180714).
2.2 Selection criteria
We identified literature that met the following inclusion criteria: (1) Types of studies: clinical studies comparing NPWT versus conventional wound dressings for closed incisions in orthopaedic surgeries, including randomised control trials (RCT) and retrospective cohort studies (RS); (2) Types of participants: adult patients who underwent arthroplasty, fracture, and spinal surgery; (3) Studies published in English and Chinese; (4) Studies reporting the outcomes, including the incidence of SSI; and (5) full-text studies available.
The exclusion criteria were listed as follows: (1) Literature types: abstracts, letters, editorials, conference articles, case reports, reviews, animal studies, and study protocols; (2) Studies that failed to provide a direct comparison between NPWT and conventional wound dressings, or the comparative results impossible to be deduced indirectly from the published results; and (3) Repetitive studies and data.
2.3 Search methods
Two independent reviewers performed a literature search following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA). Seven electronic databases (Medline, Web of Science, PubMed, Embase, Google Scholar, Cochrane Library, and CNKI) were searched from the inception of these databases to August 1, 2022. The following free terms and MeSH terms were used, such as “NPWT”, “fracture”, “orthopaedic trauma”, “arthroplasty”, “spinal surgery”, and “surgical site infections”. All the retrieved literature were scrutinised further, including the title, abstract, and full text to ensure that the selected literature fully met the inclusion criteria.
2.4 Criteria of grouping and associated definitions
Following the well-accepted practice of previous studies,12-16 the NPWT group was recognised as a medical practice of using an open-cell solid foam or gauze laid onto the wound followed by an adherent sealed dressing. In this progress, a sealed tube was connected from the dressing to a suction pump, creating a partial vacuum over the wound. NPWT mainly adopted low negative pressure (generally 55 mmHg-175 mmHg). All hospitals used a sterile dressing sealed from external contamination. The details of the materials used were again left to the discretion of the healthcare team as per routine care at their centres.
2.5 Data analysis
In this study, meta-analysis of the included literature was implemented with Stata 17.0. Odds ratio (OR) and the standardised mean difference (SMD) were adopted, and the 95% confidence interval (CI) was used to describe dichotomous variables and continuous variables. When P < .05, it was considered that there was a statistically significant difference between the experimental group and the control group. The I2 quantitative test was used to evaluate the heterogeneity of meta-analysis results. An I2 < 50% suggests low heterogeneity in the meta-analysis results, then a fixed-effect model can be applied; an I2 ≥ 50% indicates high heterogeneity in the meta-analysis results; then, a random-effect model can be selected; and an I2 > 75% suggests obvious heterogeneity in the meta-analysis results. At this time, the sources of heterogeneity need to be carefully examined through sensitivity analysis. A funnel plot and Egger's test were adopted to examine possible publication bias. When publication bias occurred, the trim and fill analysis was applied to further evaluate the stability and reliability of the results. Finally, we performed the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) to clarify the overall certainty of evidence.17
2.6 Quality evaluation
Two investigators (Yuan and Chen) independently assessed the risk of bias using the Cochrane Risk of Bias 2.0 tool; any disagreement concerning the quality evaluation was resolved by discussion and consensus.18 The Cochrane Risk of Bias tool includes five specific domains: the randomisation process, deviations from intended interventions, missing outcome data, measurement of the outcome, and selection of the reported results. The tool provides an overall rating of a study, and the measured results can be classified into low-risk bias, high-risk bias, or unclear risk of bias according to prescribed judging criteria.
3 RESULTS
3.1 Descriptive statistics
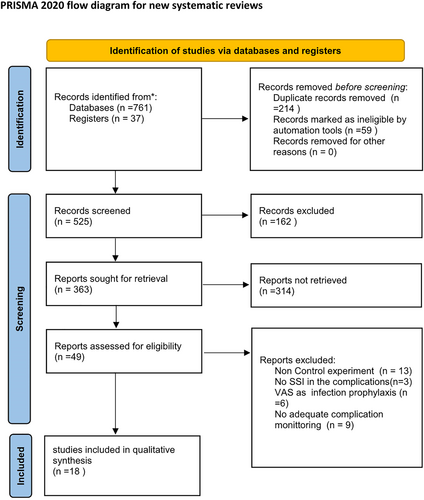
A total of 798 records were identified from the above-mentioned databases. Among them, 525 studies remained after duplicate records and those marked ineligible by automated tools were removed. Forty nine studies remained further after title and abstract screening. Finally, 18 studies were screened for quantitative synthesis and meta-analysis after checked with the selection criteria (Figure 1). It is noteworthy that no restrictions were placed on the types of clinical trial design.
3.2 Quality evaluation
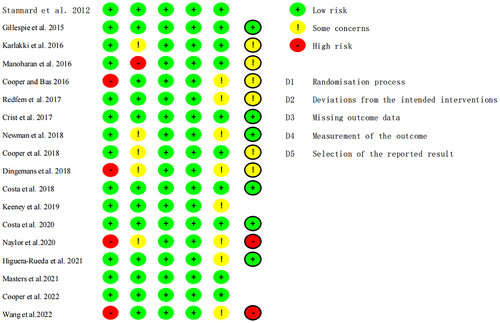
As suggested by the results of the bias risk assessment, five bias areas were evaluated, including the randomisation process, deviation from expected interventions, missing outcome data, outcome measurement, and the selection of reported outcomes. Figure S1 and Figure 2 show that 10 RCTs are confirmed with a low risk of bias, while the remaining eight RCTs are classified with some concerns. The domain highly rated with some concerns was the randomisation process. Ten randomised controlled trials had clear randomization schemes. The patients were well informed of the treatment.
3.3 Characteristics of included literature
The characteristics of the included studies were shown in Table 1. A total of 5525 patients were involved, including 2467 patients in the NPWT group and 2092 patients in the control group (conventional wound dressings). Five of all the studies were retrospective studies,19-24 and the other 13 were RCTs.12-16, 24-31
| Study | Total patients (n) | Study Design | Groups size | Age, mean (SD) | BMI, mean (SD) | Male, No. (%) | Duration of NPWT treatment | Follow-up | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NPWT group (n) | Comparison group (n) | NPWT group (n) | Comparison group (n) | NPWT group (n) | Comparison group (n) | NPWT group (n) | Comparison group (n) | |||||
| Stannard et al. 2012 | 249 | RCT | 130 | 119 | 43 | - | - | 84 (65) | 77 (65) | 59 h | NR | |
| Gillespie et al. 2015 | 70 | RCT (2013–2014) | 35 | 35 | 63.8 (14.0) | 62.5 (12.4) | 29.9 (5.7) | 29.8 (5.3) | 20 (57) | 17 (49) | 5 days | 6 weeks |
| Karlakki et al. 2016 | 209 | RCT (2012–2013) | 102 | 107 | 69.0 (9.0) | 69.2 (9.0) | 30.1 (5.0) | 28.4 (4.6) | 49 (48) | 55 (51) | 7 days | 6 weeks |
| Manoharan et al. 2016 | 33 | RCT (2014) | 21 | 36 | 66 | 29.79 | 19 (58) | - | 8 days | NR | ||
| Cooper and Bas. 2016 | 138 | RS (2021–2015) | 30 | 108 | 71.7 | 70.9 | 31.3 | 29.6 | - | - | 9.2 days | 90 days |
| Redfern et al. 2017 | 596 | RCT (2013–2014) | 196 | 400 | 66.9 (10.2) | 66.8 (10.8) | 30.5 (5.5) | 30.9 (5.0) | 67 (34) | 184 (46) | 7 days | 6 weeks |
| Crist et al. 2017 | 66 | RCT (2008–2012) | 33 | 33 | 44.2 | 43.2 | 29.9 | 31 | 27 (82) | 20 (61) | >2 days | NR |
| Newman et al. 2018 | 159 | RCT | 79 | 80 | 65 (11) | 65 (11) | 31.9 (7.5) | 33.4 (7.5) | 40 (51) | 45 (56) | 2 days | 12 weeks |
| Cooper et al. 2018 | 57 | RS (2010–2016) | 27 | 40 | 76.3 | 73.2 | 27.3 | 29.9 | - | - | 7 days | 90 days |
| Dingemans et al. 2018 | 100 | RS (2000–2016) | 53 | 47 | 43.9 (15.6) | 42.2 (14.6) | 24.4 | 24.7 | 39 (74) | 36 (77) | 7 days | 2–4 weeks |
| Costa et al. 2018 | 460 | RCT (2012–2015) | 226 | 234 | 46.1 (19.9) | 44.5 (19.0) | 46.4 | 47 | 178 (79) | 164 (70) | NR | 1 year |
| Keeney et al. 2019 | 398 | RCT (2014–2017) | 185 | 213 | 60.6 | 60.5 | 34.6 | 36.5 | - | - | 7–35 days | 2 years |
| Costa et al. 2020 | 1519 | RCT (2016–2018) | 770 | 749 | 49.8 (20.3) | 26.4 (5.9) | 26.7 (6.0) | 482 (62) | 482 (63) | NR | 90 days | |
| Naylor et al. 2020 | 469 | RS (2015–2018) | 76 | 393 | 58.1 (13.5) | 60.8 (12.6) | 29.0 (6.1) | 29.4 (6.5) | - | - | 5 days | NR |
| Masters et al.2021 | 432 | RCT | 214 | 218 | 85.2 | 84.9 | - | - | 66 (31) | 59 (27) | NR | 120 days |
| Higuera-Rueda et al. 2021 | 242 | RCT (2017–2019) | 124 | 118 | 64.7 (9.5) | 65.1 (8.5) | 34.7 (6.7) | 34.2 (7.2) | 98 (40) | - | 5 days | 90 days |
| Cooper et al. 2022 | 294 | RCT (2018–2019) | 147 | 147 | 64.9 | - | - | 119 (40) | - | NR | NR | |
| Wang et al. 2022 | 34 | RS (2012–2020) | 19 | 15 | 55.2 (14.4) | 54.3 (15.4) | 24.3 (3.4) | 25.0 (3.2) | 9 (47) | 8 (53) | NR | 90 days |
- Abbreviations: LOS, length of stay; NPWT, negative pressure wound therapy; NR, no reported; RCT, randomised controlled trial; RS, retrospective study.
4 DESCRIPTION OF RESULTS
4.1 The incidence of SSI
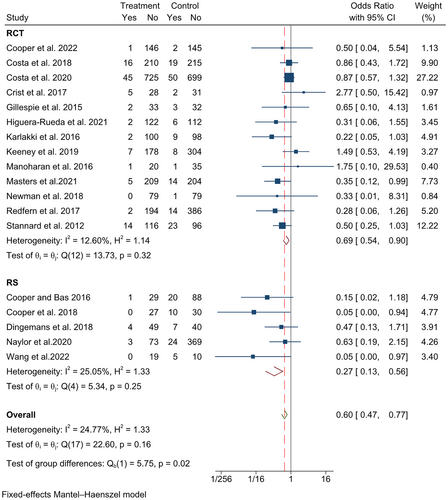
The forest plots synthesised all the data involving SSI, of which 110 of 2467 patients were found with SSI in the NPWT group and 218 of 3092 patients in the control group. The incidence of SSI in the NPWT group was significantly lower than that in the control group (OR = 0.60, 95% CI 0.47-0.77, P < 0.001) (Figure 3). Subgroup analyses were conducted according to study design and operation site. The incidence of SSI in the NPWT group after arthroplasty was 46% relative to the control group (95% CI 0.27 to 0.79), followed by fracture (OR = 0.69, 95% CI 0.52-0.91), and spinal surgery (OR = 0.37, 95% CI 0.12-1.12). There was no significant difference by operation site (P = 0.29) (Figure 4). Furthermore, RS (OR = 0.27, 95% CI 0.13-0.56) achieved a better result than RCT (OR = 0.69, 95% CI 0.54 to 0.90). A significant difference was found by study design (P = 0.02) (Figure 5).


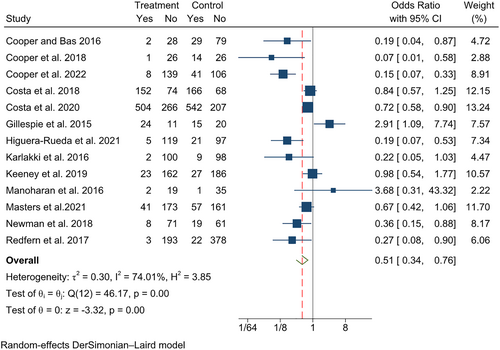
4.2 Total complications
Total complications were reported in 13 studies, with 2156 patients found in the NPWT group and 2485 patients in the control group. 35.95% of the patients in the NPWT group underwent complications, and 38.75% in the control group. The total complication rate in the NPWT group was significantly lower relative to the control group (OR = 0.51, 95% CI 0.34-0.76), although high heterogeneity existed (Figure 6).
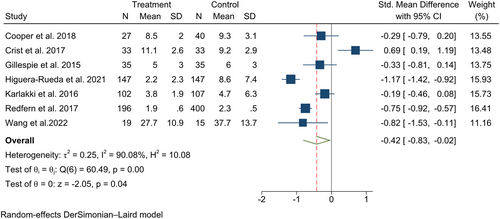
4.3 Length of hospital stay (LOS)
Length of hospital stay was reported in seven studies, comprising 559 patients in the NPWT group and 777 patients in the control group. The average LOS of 4.20 and 5.06 days were found in the NPWT group and the control group, respectively. As shown in Figure 7, LOS in the NPWT group was shorter relative to the control group, although high heterogeneity existed (SMD = −0.42, 95% CI −0.83 to −0.02).
4.4 Publication bias
Publication bias was assessed by a funnel plot and Egger's test (Figure 8 and Figure S2). Although the P value was found to be 0.033 (Figure S3), the trim and fill analysis recognised these results stable (Figure S4).

4.5 Evidence grading
Primary and secondary outcomes in this meta-analysis were evaluated using the GRADE system (Table S1). The evidence quality of SSI, total complications was high, moderate, and low, respectively. We demonstrated that the overall evidence quality is moderate, which means that further research is likely to significantly change confidence in the effect estimate and may change the estimate.
5 DISCUSSION
The successful application of NPWT in healing wounds in general has led some doctors to apply NPWT to orthopaedic surgical wound dressing. This study set out a meta-analysis to compare the incidence of SSI in varied orthopaedic surgeries between NWPT and conventional wound dressing. It is found that the incidence of SSI is lower in patients in the NPWT group relative to the control group. Subgroup analyses were conducted to evaluate the change of incidence of SSI in different study designs and operation sites. Moreover, we found a lower total complication rate and shorter length of hospital stay in the NPWT group.
Previous studies have shown that reducing surgical site infection in NPWT is biologically feasible.32 Proposed mechanisms of NPWT could achieve wound shrinkage, clean extracellular fluid, and induction of cellular stretch, which are supposed to accelerate wound healing, thus creating a favourable healing environment for angiogenesis.33 In addition,it may also serve as a microbial barrier that helps to increase blood flow and improve tissue oxygenation. In open wounds, NPWT contributes to wound healing through clearing excess interstitial fluid, reducing edema, and promoting tissue growth.34
The findings of this study were consistent with previous meta-analyses. Five studies from 2018 to 2021 show with strong evidence that NPWT can significantly reduce the incidence of SSI in orthopaedic surgery wounds, whether the wounds are deep or shallow.35-39 Furthermore, NPWT promotes not only rapid healing of open fracture wounds,35 but also be effective in cases of wound dehiscence.10, 37 Some studies also evaluate other outcomes, such as mortality, reoperation, incidence of seroma, pain, quality of life scores, and so forth.38, 39 However, it is reported that NPWT significantly increased the medical cost of patients undergoing elective primary hip arthroplasty.13
This is a comprehensive meta-analysis to evaluate the incidence of SSI between NPWT and traditional wound dressings in varied orthopaedic surgeries and compare relevant efficacies among different operation sites. We also assessed data from both randomised trials and observational studies, applying the GRADE approach to appraise the available evidence. However, very few studies have demonstrated any economic benefits of NPWT application in varied orthopaedic surgeries. In addition, long-term use of NPWT may bring in added values, like accelerating the final reconstruction of muscle and fasciocutaneous flap recovery. Therefore, more evidence is welcome to prove the feasibility and effectiveness of NPWT in this field.
This meta-analysis has some limitations. First, despite that most of the included studies had a scientific and rigorous experimental design, high patient compliance, low follow-up losses, and high quality, the above-mentioned factors also contributed a lot to the unclear risk of bias, thus accounting for high heterogeneity in the meta-analysis results as well. Secondly, the injury severity and treatment protocol of these studies varied, and not all studies reported the details. Third, the patients in the studies received NPWT at different durations and frequencies. Therefore, high-quality RCTs with a larger sample size and standard protocol should be incorporated in future studies to examine the role of NPWT for the incidence of SSI, length of hospital stay as well as comprehensive medical cost.
To sum up, NPWT may be a safe and effective way to accelerate wound healing in arthroplasty, fracture, and spinal surgery. The rational use of NPWT should be based on the presence of patients' clinical conditions and relevant risk factors.
AUTHOR CONTRIBUTIONS
All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. YS designed the study. YS and DL acquired the study data. HF and ZZ analysed and interpreted the data. YS wrote the first draft of the manuscript. All authors revised the manuscript and approved it for publication.
FUNDING INFORMATION
Sichuan Provincial Science and Technology Plan, Grant#: 2018JY0324.
CONFLICT OF INTEREST
All authors have no conflict of interest to report for this study.
ETHICAL APPROVAL
Ethical approval was waived for this meta-analysis because it only involves published patient data.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing not applicable to this article as no datasets were generated or analysed during the current study