Effect of the addition of chlorhexidine and miswak extract on the clinical performance and antibacterial properties of conventional glass ionomer: an in vivo study
Abstract
Background
Antibacterial restorations can increase the success rate of minimum invasive dentistry especially in young permanent molars with deep carious lesions as an attempt to preserve maximum dental structure and avoid pulp exposure. Further research is warranted to evaluate different antibacterial agents.
Objectives
This study aimed to evaluate the efficacy of adding chlorhexidine gluconate (CHX) or aqueous miswak (Salvadora persica) extract on the clinical performance and in vivo antibacterial activity of conventional anhydrous glass ionomer cement (GIC).
Design
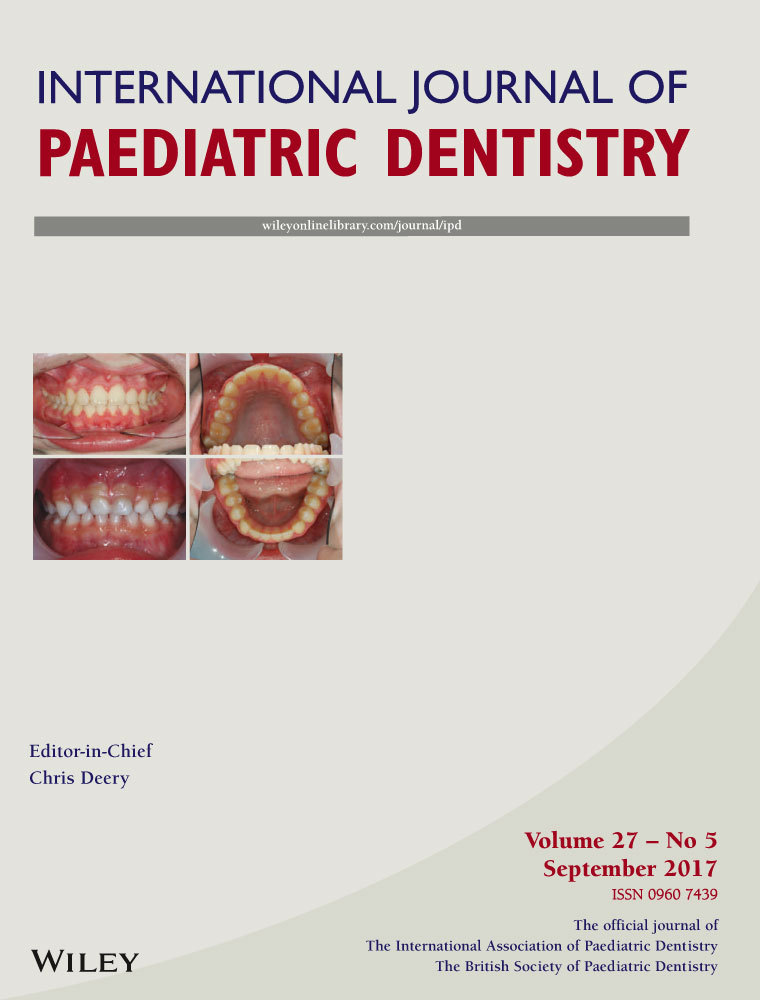
The study was a randomized clinical trial. Sixty young permanent molars, with deep carious lesions in 6- to 9-year-old children were included. After randomization, atraumatic restorative treatment (ART) or stepwise excavation was performed followed by bacterial sampling from the center of the remaining carious dentine in the floor of the pulp. GIC powder was mixed with 0.5% chlorhexidine gluconate liquid in group I; with 100% aqueous miswak in group II; and with deionized water in group III (control). Clinical performance for all groups was assessed at 3, 6, and 9 months. After 9 months, restorations were removed and a second bacterial sample was collected for Streptococcus mutans (S. mutans) quantification and analysis by real-time polymerase chain reaction (PCR) test.
Results
Results showed no statistically significant difference in the success rate of the three groups at the 3-month interval. At 6 and 9 months, however, restoration success was 75% then 60% in group I, 100% then 90% in group II, and 95% then 85% in control group. Group II and the control group showed statistically significant higher survival rates than group I. All groups showed reduction in S. mutans counts in underlying dentine, but the percent reduction was significantly higher in group I. (P < 0.001).
Conclusions
The addition of CHX and miswak to GIC showed superior antibacterial properties than conventional GIC, without seriously affecting the clinical performance of the restoration until the 6-month follow-up, but failure significantly increased in terms of marginal defects at 9 months with CHX (group 1).