Healthcare Professional Perspectives on the Impact of the Physical Health Nurse Consultant
Funding: The authors received no specific funding for this work.
ABSTRACT
Early mortality experienced by people living with mental health issues (hereon termed consumers) is largely preventable. Healthcare professionals perceive healthcare system inadequacies such as diagnostic overshadowing, stigma and fragmentation of physical and mental healthcare services can be resolved through effective integration approaches. Service- and individual-level integration approaches involve multidisciplinary teams collaborating and coordinating care to holistically meet consumers' physical and mental health needs. Evidence suggests appropriately trained healthcare professionals can deliver effective integrated treatment without financial or organisational restructuring. Specialist nursing positions such as Physical Health Nurse Consultants can support and integrate physical and mental health care. Consumers report the Physical Health Nurse Consultant as providing dedicated, integrated, coordinated and holistic mental and physical health care. This study aimed to explore the Physical Health Nurse Consultant role from the perspectives of healthcare professionals. A qualitative exploratory study design was used. Fourteen healthcare professionals participated in individual interviews or focus groups. Interview recordings were transcribed, and thematically analysed. Three themes were identified: (i) role functions, including integration of physical and mental health care, (ii) impact on consumer physical health outcomes and (iii) impact on service delivery. Healthcare professionals perceive the Physical Health Nurse Consultant effectively integrates physical and mental health care and subsequently support the continuation and embedding of the role in routine practice. Future research is required to explore healthcare professionals' experiences and perceptions of how these roles be translated to routine clinical practice. Examining the professional development requirements, service provider constraints and economic implication to achieve these outcomes also warrants attention.
1 Introduction
Concerted efforts to reduce the alarming premature mortality for people diagnosed with mental illness, (hereon referred to as consumers), have increased, yet physical health disparities persist (Chan et al. 2023; Roberts et al. 2022). Integrated physical and mental health care is recognised by consumers and healthcare professionals as a preferred solution to improve physical health outcomes (Green et al. 2022; Dickens et al. 2019). One approach to applying integrated care in practice involves embedding a Physical Health Nurse Consultant (PHNC) within a mental health setting to coordinate and deliver physical health care (Happell et al. 2018). Current literature focuses on nurses, carers and consumers' views and experiences with the PHNC role. There is limited body of evidence regarding the impact of the PHNC role within an integrated context. The perspectives of other healthcare professionals are crucial in the successful implementation of a specialist physical health nursing role such as the PHNC, yet their perspectives and experiences with the PHNC role are yet to be explored. Findings from individual interviews and focus groups with healthcare professionals indicate specialist mental health nursing roles such as the PHNC possess personal and professional attributes to effectively deliver integrated physical and mental health care (Cheetham, Arunogiri, and Lubman 2023; Rodgers et al. 2018). The unique insights provided by healthcare professionals who worked directly with the PHNC role adds to the trustworthiness of their perceived value and contribute to future role developments and contextual implementation approaches relevant and beneficial to carers, public and private healthcare services. Taken together, the translation of new knowledge to practice will benefit the physical health care of people experiencing mental ill health.
1.1 Background
Integrating physical and mental health care is vital in reducing the early mortality of up to 25 years for consumers (Chan et al. 2023; Fiorillo and Sartorius 2021; Firth et al. 2019). The early mortality and increased morbidity consumers experience compared to the general population is an amalgamation of preventable physical health comorbidities such as cardiometabolic syndrome, socioeconomic and healthcare system factors (Chan et al. 2023; Roberts et al. 2022; Rodgers et al. 2018). Efforts to improve the physical health outcomes and care for consumers are well described in the literature. A plethora of reviews report interventions seeking to: (i) increase access to and uptake of physical health screening (Lamontagne-Godwin et al. 2018); (ii) improve lifestyle behaviours such as physical activity and diet (Bradley et al. 2022); (iii) identify nurse-led interventions (Happell et al. 2023); (iv) promote the use of physical health care (Strunz et al. 2022); and (v) map integrated service models of care to improve physical health care for consumers (Rodgers et al. 2018). Despite these efforts, the mortality gap between consumers and the general population continues to widen (Chan et al. 2023; Fiorillo and Sartorius 2021; Hayes et al. 2017; Roberts et al. 2022).
Healthcare system inadequacies such as stigma towards consumers, diagnostic overshadowing, fragmentation and insufficient integration of physical and mental health care contribute to these physical health disparities (Molloy et al. 2023; Rodgers et al. 2018; Strunz et al. 2022). Stigma and diagnostic overshadowing occur when healthcare professionals misattribute consumer physical health concerns as mental health issues (Molloy et al. 2023). These experiences often preclude consumers from accessing and receiving adequate physical health care (Molloy et al. 2023). When healthcare systems fail to respond to consumers' holistic needs, further marginalisation and health inequities are imminent (Duggan et al. 2020; Molloy et al. 2023). Integrating physical and mental health care is a frequently proposed solution to effectively work with consumers in redressing physical health disparities (Cheetham, Arunogiri, and Lubman 2023; Fiorillo and Sartorius 2021; Firth et al. 2019; Molloy et al. 2023).
Broadly, integrated care is a multifaceted approach used to overcome fragmentations and inadequate coordination and has various conceptual frameworks and taxonomies (Goodwin 2016). In this paper, service and individual level integration approaches are the focal points as they typically involve multidisciplinary teams collaborating and coordinating care to holistically meet the consumers' physical and mental health needs (Cheetham, Arunogiri, and Lubman 2023; Goodwin 2016). To effectively integrate care, interpersonal and service level drivers such as co-location of physical and mental healthcare providers, informal and conversational handover approaches, collaborative collegial relationships between healthcare professionals, strong leadership support and shared electronic health records are required (Monaghan and Cos 2021). A review examining the barriers, facilitators and evaluations of integrated care mirrors these drivers and suggests shared protocols, joint action plans and decision support tools clarify healthcare professionals' responsibilities, communication and record keeping (Rodgers et al. 2018). Integrated care encompassing these levers results in better coordination, stigma reduction and access to services for consumers who subsequently experience improved physical health outcomes (Cheetham, Arunogiri, and Lubman 2023; Monaghan and Cos 2021).
Application of integrated care approaches require appropriately skilled, interpersonally capable and empowered healthcare professionals to deliver services (Rodgers et al. 2018). A recent narrative review examining Australian research evaluations of the effectiveness of novel and effective integrated treatment approaches demonstrated this can be achieved without financial or organisational restructuring (Cheetham, Arunogiri, and Lubman 2023). Specialist mental health nursing positions such as the PHNC are well situated, skilled and trained to support and integrate physical and mental health care (Happell et al. 2018; Hassan et al. 2020). Trials of similar Cardiometabolic Health Nurse (CHN) roles coordinating and integrating mental and physical health to deliver systematic and comprehensive preventative care and treatment demonstrated capacity and capability for specialist mental health nursing roles to support consumers' physical health (Happell et al. 2014; McKenna et al. 2014). Enduring calls to action and promising results from the CHN trial led to the emergence and embedding of a PHNC within mental health services (Happell et al. 2018, 2019). Consumers working with the PHNC role have reported experiences of dedicated, integrated, coordinated and holistic mental and physical health care (Tabvuma, Stanton, and Happell 2022). These experiences align with the intent of the role's description (Happell et al. 2018) and confirm prior research findings that appropriately skilled and trained clinicians can deliver effective integrated treatment (Cheetham, Arunogiri, and Lubman 2023; Rodgers et al. 2018). Existing studies focus on nurses, carers and consumers' views and experiences with the PHNC role. There is limited body of evidence regarding the impact of the PHNC role within an integrated context. To fully understand the impact of the role within an integrated care context, it is critical to explore the perspectives and experiences of healthcare professionals working with the PHNC during its implementation.
1.2 Aim
Situated within a large implementation study of the PHNC role, this study aims to explore healthcare professionals' perspectives and experiences of working with the PHNC role. Exploring the views and experiences of healthcare professionals provides insights into the perceived impacts of the role on consumers and service delivery, particularly in an integrated care context.
2 Methods
2.1 Study Design
A qualitative exploratory design encompassing individual interviews and focus groups was used to gain an in-depth understanding of the PHNC role from the perspectives and experiences of healthcare professionals (Stebbins 2001). This approach is recommended for novel phenomenon where limited knowledge exists (Katharine et al. 2019). This manuscript adheres to the COREQ (Consolidated criteria for Reporting Qualitative research) guidelines for reporting qualitative research (Tong, Sainsbury, and Craig 2007).
2.2 Setting
The present study was conducted in May 2021 at two sites within an Australian public Community Mental Health Service (CMHS). The service offers mental health support to people aged 18 to 65 and diagnosed with a range of mental health conditions. Services include day services, assertive care and outpatient programmes including the acute response team, and forensic consultation and intervention service.
2.3 Physical Health Nurse Consultant Role
- The Positive Cardiometabolic Health treatment framework (Curtis, Newall, and Samaras 2012). This framework considers the clinical and behavioural risks identified as part of cardiometabolic assessment, along with the consumer's self-identified needs, goals and health priorities, shared decision making with the consumer and local availability and consumer acceptability of management options.
- Care coordination. The PHNC received training in care coordination including referral to appropriate programmes or services; communicating and documenting relevant clinical history, approaches to communicating with consumers and timely follow-up of results.
- The PHNC received ongoing clinical and research supervision from members of the research team.
The PHNC was co-located at two sites within the CMHS. Co-location involved embedding the PHNC role within clinical teams to share resources such as office space and electronic medical records. Considering the high propensity for physical health issues for consumers diagnosed with psychosis, the PHNC role worked with this cohort by providing health behaviour change advice, integrating and coordinating physical and mental health care. Approaches to physical health care delivery by the PHNC were informed by the Positive Cardiometabolic Health treatment framework, an internationally established guideline for metabolic screening, prevention and interventions (Curtis, Newall, and Samaras 2012). Consumers were supported by the PHNC to identify and implement their self-identified goals and health priorities. Additionally, and if required, the PHNC referred consumers to allied health services such as exercise physiologists and dieticians to ensure holistic care.
2.4 Study Population and Recruitment
Fourteen healthcare professionals working with the PHNC at the two CMHS sites participated in this study. A convenience sampling approach was used. The lead author, a female Credentialed Mental Health Nurse with no prior relationships with participants, promoted the study via group emails and staff meetings. Further study information, participant Information Sheets and consent forms were provided to interested participants.
2.5 Procedure
In May 2021, seven semi-structured individual interviews and two focus groups ranging between 45 and 90 min were conducted until no evidence of new themes was identified from the concurrent data analysis (Vasileiou et al. 2018). Focus groups were conducted in person. Individual interviews occurred in person, via telephone and videoconference as preferred by the participant. All participants provided written informed consent prior to interviews and focus groups. Following the individual interviews, participants had the opportunity to review a password-protected individual transcript via email.
2.6 Analysis
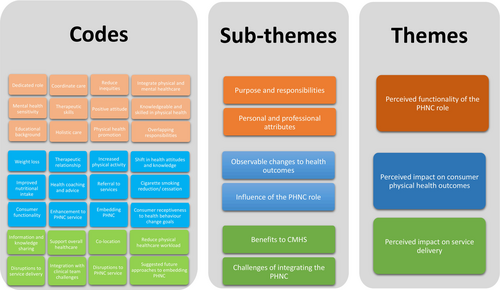
Audio recordings of interviews and focus groups were transcribed verbatim by the lead author, and thematically analysed according to the six-step Braun and Clarke (2022) framework using NVIVO 14 (QSR International, Burlington, MA). Inductive thematic analysis is frequently used in qualitative research because it provides a systematic approach to organise, interrogate and interpret data (Braun and Clarke 2022). Using NVIVO 14 and an inductive process throughout the six stages; (i) transcripts were re-read to familiarise researchers with data leading to (ii) identification of similar concepts which were coded. Similar codes were grouped to generate (iii) initial themes. These initial themes were further (iv) reviewed to broadly reflect the content. Discrepancies in interpretation of themes were discussed and resolved by the research team. Consensus themes were (v) refined for (vi) reporting in academic outputs (Braun and Clarke 2022) (Figure 1).
2.7 Trustworthiness
Triangulation, reflexivity and member checks were used to limit bias and increase rigour. Investigator triangulation and reflexivity enhanced the credibility and trustworthiness of data by obtaining multiple perspectives about the PHNC role and, personal and professional discipline biases discussed and resolved. This process involved three members of the research team, with PhD qualifications, backgrounds in nursing and exercise physiology and qualitative research, reflecting and resolving their interpretations of data, assumptions and opinions about the research topic (Braun and Clarke 2022). To further strengthen the trustworthiness of data, member checks were performed by individually interviewed participants from varying health disciplines who reviewed and verified the accuracy of their transcripts.
2.8 Ethics
This study was guided by the National Statement on Ethical Conduct in Human Research (Commonwealth of Australia 2018). Ethics approval was gained from ACT Health Human Research and Ethics Committee (approval number 2020/ETH.00081), prior to participant recruitments. Participants received a Participant Information Sheet containing study information, including data collection, usage and storage. Researchers maintained participant confidentiality and anonymity by confining the identities of participants to the researchers and maintaining confidentiality during the data analysis and reporting phase.
3 Results
Fourteen healthcare professionals participated in this study which explored their perspectives and experiences with the PHNC role. Participants' professional backgrounds included seven registered nurses, two social workers, one nurse practitioner, occupational therapist, psychologist, academic and allied health assistant, respectively. Participants had between 9 months and 40 years of professional experience, reflecting a broad spectrum of expertise and insights. This diverse sample ensured a comprehensive exploration of the perceived impact of the PHNC from the healthcare professions likely to work alongside the PHNC in a clinical setting.
Three themes identified from the data convey participants' perceptions of the PHNC's: (i) role functions, including integration of physical and mental health care, (ii) impact on consumer physical health outcomes and (iii) impact on service delivery.
3.1 Theme 1: Perceived Functionality of the PHNC Role
My understanding of the [PHNC] role was they exclusively looked after physical health of patients taking antipsychotic medications to mitigate the risk factors for the metabolic syndrome that a lot of people experience once they start taking the antipsychotic medication… the role of the physical nurse was to purely advocate for the physical health of the patient by monitoring and by assessing the patient through the journey of the treatment. (Participant 1)
It's a really important role… nurses are very well placed to provide that service because of their educational background, which I think is more holistic than other disciplines… the combination of their knowledge and skill and their more positive attitudes and their availability means that it's very important. (Participant 7)
We spend so much time concentrating on people's mental health and their risk, that so much of the physical stuff just gets left behind or is not seen as important. The [PHNC] role has lots of potential… a dedicated position… to improve the physical health of our clients. (Participant 3)
I was surprised when I first heard that the idea was being proposed…because I thought that was something that nurses [promote health] generally did anyway…Are they [PHNC] trying to take over the role of their GP because that's where I'd see the GP's role being in that area… people are already engaged with their GP. (Participant 6)
3.2 Theme 2: Perceived Impact on Consumer Physical Health Outcomes
Most of the clients said that it [PHNC] had helped them a great deal… One amazing male consumer kept losing astronomical amounts [of weight]. In the beginning, he was in a severely obese category, and in the end, he was down at the lower end of the overweight category on the BMI scale. (Participant 2)
A lot of people were able to have a better understanding of nutrition… a lot of people were adding vegetables and fruit into their diet who weren't before…people who will have increased their exercise for sure, like [some were less] sedentary and … wiser food choices… People felt they were getting positive experience, regardless of where they're up to. (Participant 5)
Definitely the attendance at that quit smoking went up and people quit smoking… It's amazing. They'd been trying before, and they were able to quit. (Participant 2)
…there were people who were not as high functioning who managed to quit smoking and I can't attribute that all to just what [the PHNC] was doing, but I definitely saw some significant changes with people who weren't as high functioning…The role would sit really well in a structured program, like how they do it at the Bondi Junction clinic, where … they all work together and people are part of the program. (Participant 5)
…There were two groups [of consumers]. One was the one that were maximising the physical nurse. They were very happy with the plan [goals]. They felt enabled and you could see that they were enthusiastic …There was another group that they felt it was too much. That the expectations…from the physical health nurse was unrealistic and that they didn't feel like that it was something they could follow…they would say I am so drowsy most of the time and I don't get up until lunchtime, I don't feel like doing physical exercise. (Participant 1)
There were some [consumers] that improved, and they looked forward to seeing the physical health nurse. There are others that whilst they saw the physical health nurse and didn't mind going, overall, I couldn't see that there was any improvement in their health …Some of them are just going to keep putting on weight regardless…People on clozapine, it's a really difficult one to maintain or lose weight. (Participant 6)
3.3 Sub-Theme 3: Perceived Impact on Service Delivery
… The nurses doing the project, there was a wealth of expertise and knowledge. Also, to share that with us has been a bonus. (FG1)
I always appreciate the assistance of the nurses on the team in terms of getting observations when a client might come in for depo [outpatient clinic for intramuscular antipsychotic injections] … having that separation from the medication administration… makes it a little bit more comfortable for clients… (FG2)
I think it [PHNC] would give us shortcuts because they would guide us [navigating the system]…It [workload] would shrink it a bit, not too much but they [PHNC] will make it a lot easier for us to do our job…[PHNC] will always be there to deliver [physical healthcare] because we're dealing with [the mental health of the] consumer, but they'll [consumers] get a better service…. (FG1)
Considering the [PHNC] collocated with these teams and [PHNC service was] adding workload to admin in terms of taking messages and sending emails…I think they were quite supportive. [Site B] was not as supportive as [Site A]. [PHNC] on the same floor in the same office as the team [at Site A]. In [Site B], [PHNC] on a completely different floor…have nothing to do with the team… (Participant 3)
Maybe that would be different if it was an actual role…Someone who was part of the [clinical] team… rather than someone that comes in and out… a permanent position within each community team. (Participant 3)
There was difficulty getting rooms…they [clinical staff] did ask [PHNC] to leave the room, for their clients, not identifying the fact that participants were also clients of that service. The idea that you would kick somebody out of the room in the middle of a consultation…I was just horrified that that would ever happen. We [project team] had a meeting about that with the team leaders and I think that resolved… (Participant 7)
4 Discussion
The present study sought to explore the perspectives and experiences of healthcare professionals with the PHNC role. Results indicated broad support for the continuation of the PHNC role stemming from participants perceiving positive consumer health behaviour changes such as increased physical activity, reduced cigarette smoking and improved nutrition. Moreover, participants recognised and attributed improvements in health outcomes such as weight loss to a multidisciplinary approach inclusive of the PHNC role. Therapeutic approaches and advanced skills of the PHNC to integrate physical and mental health care were considered strong contributors to producing positive behavioural and health outcomes for consumers. Participants realised indirect benefits for themselves like reduced workload which contributed to their support for the PHNC despite some uncertainty about the function of the role. The reported uncertainty about the usefulness of the PHNC emanated from perceptions that all nurses engage in physical health promotion and the role seemingly overlapped with GP physical healthcare responsibilities. While this is an uncommon perspective in this study, it warrants consideration by facilitating critical inquiry into the PHNC role and research examining the translation of this role in practice.
Improved physical health behaviour changes for consumers such as improved nutrition was observed by participants. These changes were observed despite participants assuming the physical and mental health complexities experienced by consumers would likely hinder positive health outcomes. For example, healthcare professionals commonly attribute the negative symptoms and diagnostic overshadowing experienced by consumers as contributors to their physical health disparities (Lerbæk et al. 2019; Dickens et al. 2019; Molloy et al. 2023; Clancy et al. 2019). An ethnographic study investigating physical health management among people with schizophrenia conceptualises these prevailing participant perceptions as the normalisation and expectation for consumers' to experience poor physical health as part of their recovery journey (Lerbæk, Jørgensen, and McCloughen 2023). Normalisation in this context is a process whereby healthcare professionals become habituated to consumers experiencing numerous ongoing physical health issues and daily functional capacity challenges (Lerbæk, Jørgensen, and McCloughen 2023). In this study, normalisation presented itself as some participants deprioritising the importance of physical health care as exemplified by the mid-consultation disruption to the PHNC service. This possibly explains the negative or ambivalent attitudes and behaviours of some participants towards the PHNC. It is important to note normalisation within this context is an emerging concept therefore caution is required in its application as a potential explanatory model for persisting physical health disparities. Nevertheless, healthcare professionals are acutely aware and concerned about the physical health disparities consumers' experience (Fiorillo and Sartorius 2021; Sampogna et al. 2022; Molloy et al. 2023). Healthcare professionals and consumers continue to strongly advocate for focussed, integrated and coordinated efforts to redress physical health disparities (Tabvuma et al. 2022; Happell et al. 2018; Fiorillo and Sartorius 2021; Strunz et al. 2022). The findings suggest participants believed the dedicated PHNC role ensured consumer physical health needs were met. Considering participants' expectations of barriers to positive consumer health outcomes, their reports of observable positive physical health behaviour changes signify potential for the role to reduce physical health disparities when implemented long term.
Positive physical health behaviour changes for consumers were attributed to the skills and therapeutic approaches used by the PHNC. Participants described the role as a dedicated position providing and coordinating holistic health care while maintaining mental health sensitivity. These descriptions demonstrate an alignment with the proposed intent of the role (Happell et al. 2018) and prior research demonstrating the capacity of advanced clinicians to effectively deliver integrated treatment (Cheetham, Arunogiri, and Lubman 2023). Similar descriptions of consumers receiving dedicated, integrated, coordinated and holistic mental and physical health care from the PHNC were reported by Tabvuma, Stanton, and Happell (2022). The functionality of the PHNC role reflects essential elements described in research as conduits for addressing physical health disparities. These elements include integration and coordination of physical and mental health care, coordination and collaboration with community resources, continuity of care and person-centred approaches (Strunz et al. 2022; Fiorillo and Sartorius 2021; Goodwin 2016; Rodgers et al. 2018). Additionally, therapeutic skills such as empathy, non-judgement and positivity to create a safe and supportive environment were features identified by participants. Strong therapeutic relationships and integrated care approaches are highly valued by consumers and perceived to positively impact their personal and health outcomes (Tabvuma, Stanton, and Happell 2022; Cheetham, Arunogiri, and Lubman 2023; Monaghan and Cos 2021; Green et al. 2022).
The literature exploring perceptions of quality health care indicate effective care processes include interpersonal connection with the healthcare professionals, person-centred and integrated care, patience, empathy and reassurance (Hannawa et al. 2022). Person-centred and integrated approaches that empower and genuinely include consumers in their healthcare journey contribute to increased engagement in the recovery process (Hartley et al. 2020; Hassan et al. 2020; Wu, Yang, and Chen 2021; Cheetham, Arunogiri, and Lubman 2023). Effective therapeutic relationships with consumers have been correlated with reduced use of emergency services and length of hospital stay (Yağar 2021). For this reason, the positive association between the perceived effective PHNC therapeutic and integrated approaches and positive consumer health behaviours changes warrant further investigation. Furthermore, the perceived positive impact of the PHNC role on consumer health outcomes and health behaviours, may hold unrealised potential cost savings for the healthcare service.
The perceived impact of integrating a PHNC role into a CMHS setting raised mixed responses. Notably, most participants identified indirect benefits from the PHNC role such as reducing workload related to physical health care. Similar findings were reported in a study describing how a nurse-led behavioural response team improved staff safety and reduced perceived burden in caring for patients with behavioural disturbances (Afriyie-Boateng et al. 2019). Very few participants questioned the usefulness of the PHNC role based on the perception that all nurses were responsible for physical health promotion and considered an overlap in role responsibilities with GP's. While GP's are broadly considered by clinicians as the appropriate profession to address a range of physical health issues, GP's increasingly find it challenging to meet the growing expectations of their role (Clancy et al. 2019; Lerbæk, Jørgensen, and McCloughen 2023). Concerns about GP's low self-efficacy in addressing physical health problems have been raised (Fitzpatrick et al. 2018) because of ongoing healthcare professionals exhibiting diagnostic overshadowing and negative attitudes towards consumers (Happell et al. 2016; Molloy et al. 2023; Green et al. 2022). Subsequently among mental health professionals, psychiatrists and nurses are the considered primary providers of physical health care to consumers (Clancy et al. 2019; Butler et al. 2020). Nurses continue to report personal and organisational barriers such as diagnostic overshadowing, perceived role ambiguity, lack of knowledge, confidence and resources (Happell, Platania-Phung, and Scott 2014b, 2014a; Dickens et al. 2019; Green et al. 2022). Evidence supports the view that mental health nurses delivering integrated mental and physical health care must be adequately trained and skilled (Lerbæk et al. 2019; Dickens et al. 2019; Molloy et al. 2023). Participants subscribe to these views and report congruence between the PHNC role and these prerequisite advanced skillsets. In this regard, the mixed responses from participants towards the introduction of PHNC role imply technicalities of translational research with this role yet to be explored. More research is required to understand the experience of healthcare staff with the implementation of the PHNC role within a translational research context.
4.1 Limitations and Strengths
One strength is the diverse professional disciplines interviewed albeit a small sample size. This is possibly a consequence of the limited workforce at the CMHS. Another limitation is the reliance of recall and self-reported observations of changes in consumer behaviour and attitudes. However, the use of qualitative exploratory research design is a strength of this study and circumvents the recall and sampling diversity concern as participants provided their in-depth perceptions and experiences with the PHNC role, including their perceived positive impact on consumer physical health outcomes and service delivery. There is a limitation in generalising the findings from this study because data are only reflective of present participant perspectives. The study is further strengthened by having the interviews undertaken and analysed by a researcher with no prior relationship with participants, with subsequent member checks and investigator triangulation, which reduces the risk of confirmation bias.
5 Conclusion
This research contributes to a growing body of evidence suggesting specialist roles such as the PHNC effectively integrate physical and mental health care. Such roles are increasingly recognised by healthcare professionals as having positive impacts on consumers' physical health outcomes and reducing workload related to physical health care. A dedicated PHNC role is considered crucial to ensure consumer physical health needs are met. Further research is required to investigate healthcare professionals' perceptions regarding implementation of the PHNC role within a BAU model.
5.1 Relevance for Education, Practice and Research
Consumer physical health disparities continue to widen because of multifaceted barriers, including healthcare system inadequacies. Embedding the PHNC role in routine clinical practice is supported by healthcare professionals because of the perceived effectiveness to deliver integrated physical health care resulting in observable positive consumer physical health behaviours and outcomes. Further exploration of consumer, carer and healthcare professional perceptions of the barriers and facilitators of contextual co-production and implementation of the role in routine practice is required. A skilled PHNC is a potential healthcare asset that can provide mentoring and specialised training for mental health nurses and healthcare professionals to develop physical healthcare knowledge and skills. In addition to a potential mentor and educator role, the coordination and integration of physical and mental health care undertaken by the PHNC provides benefits to consumers, carers, and healthcare professionals in mental healthcare settings. Examining the professional development requirements, service provider constraints and economic implication to achieve these outcomes also warrants attention.
Acknowledgements
Thank you to the Southern Cross University for supporting TT's Doctoral Thesis. Thank you to all the participants who took part in this study. Open access publishing facilitated by Southern Cross University, as part of the Wiley - Southern Cross University agreement via the Council of Australian University Librarians.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.