Enhancing Disability Nursing Practice in Australia: Addressing Educational Preparedness
Funding: The authors received no specific funding for this work.
ABSTRACT
People with intellectual disabilities (IDs) face significant health challenges, including poor outcomes, limited access to health care, and a 26-year life expectancy gap compared with the general population. This highlights the need for improved public health and social policies to enhance the quality of care in hospital and community settings. An integrated literature review was conducted to examine the state of disability nursing practice in Australia following the implementation of the National Disability Insurance Support (NDIS) scheme. The review included English-language studies published from 2010 to 2023. Systematic searches in five databases resulted in a final sample of 28 studies. The data were then thematically analysed, and the following three themes emerged: Workforce development and professional standards, hospital experience and support needs of individuals with IDs, and nursing curriculum and ID. Study findings suggest that nurses lack preparation for effective health communication with individuals with IDs and their families. Evidence is insufficient to guide nursing practice and policies in ID care. Varying understandings of practice standards exist among nurses. Nursing curriculums in Australia fail to adequately prepare students to manage the unique needs of individuals with IDs, perpetuating the high mortality rates in this population. Specialised nursing practice areas are vital for meeting the complex needs of individuals with IDs. Reintroducing a disability nursing specialty and integrating dedicated study units and clinical placements in undergraduate programmes are recommended steps to improve care outcomes and support the overall well-being of this population.
1 Introduction
The United Nations Convention on the Rights of People with Disabilities (UN Convention on Rights of Persons with Disabilities, 2007) recognises the importance of principles and policy guidelines for equalising the opportunities for people with disabilities to mainstream their needs. It also affirms that discrimination against any person with a disability violates the inherent dignity and worth of the person as a human. Despite this, people with disabilities still encounter many barriers to participation as equal members of society (UN Convention on Rights of Persons with Disabilities, 2007). People with intellectual disabilities (IDs) should be afforded a healthy life and well-being without facing inequality resulting from their disability (UN Convention on Rights of Persons with Disabilities, 2007). The United Nations' third Sustainable Development Goal (SDG) emphasises the imperative of promoting and securing good health and well-being for all individuals (United Nations, 2015). In parallel, SDG 10 endeavours to minimise societal disparities and inequalities (United Nations, 2015). The Australian Government adheres to the principles outlined in the Disability Discrimination Act of 1992, which serves as a guiding framework in combating discrimination based on disabilities (Disability Discrimination Act, 1992).
Over half a million Australians (around 3%) have an ID (Australian Bureau of Statistics, 2012; Australian Institute of Health and Welfare [AIWH], 2008). The majority (60%) have a severe or profound disability in meeting their own daily needs and require a significant amount of support from family, caregivers or health professionals, especially nurses (AIWH, 2008; Australian Bureau of Statistics, 2012). The prevalence of ID is more than double in First Nations Australians compared with the general population, 5.9% compared with 2.5% (AIWH, 2015). However, there is still a significant disparity in the access to health care for people with disabilities. The care needs for people with disabilities are dynamic and variable, escalating in complexity where multiple disabilities exist exponentially, for example, with co-existing psychological and behavioural conditions, higher risks for heart disease, hypertension, obesity and respiratory conditions (O'Reilly et al., 2018; Wilson, Howie, & Atkins, 2019). Poor health literacy, inadequate healthcare services, low utilisation of screening and preventive services, misdiagnosis, discrimination, communication barriers and limited nurse education contribute to a higher risk of diseases (Cashin, Buckley, et al., 2022; Furst & Salvador-Carulla, 2019; Jaques et al., 2018; Trollor et al., 2018; Wilson, Howie, & Atkins, 2019). Studies have reported poor hospital experience, discrimination and lack of confidence in nurses in providing adequate care and increased reliance on caregivers for care (Hemsley et al., 2011; Jaques et al., 2018; Lacono et al., 2014; Lewis et al., 2019). Furthermore, in addressing the needs of First Nations People and Closing the Gap, priority reforms should concentrate on strengthening the workforce to deliver complex care to individuals with IDs, given the existing issue of overrepresentation (Australian Government, 2020).
It is known that people with IDs experience poorer health outcomes overall, compromised physical health and well-being and limited access to health services. Statistics demonstrate that individuals with IDs experience 38% of preventable deaths, compared with 17% in the general population. (Trollor et al., 2018; Wilson, Howie, & Atkins, 2019). Furthermore, this population has a 26-year gap in life expectancy compared with the general population, which is contributed by increased risk for lifestyle diseases, oral health issues and respiratory diseases (Wilson, Howie, & Atkins, 2019).
In Australia, national policy and public funding shifts resulted in the formation of a National Disability Insurance Scheme (NDIS) in 2013 (Buckmaster, 2017). This individualised general insurance funding model fundamentally changed the delivery mode of disability health and social care from institutionalised care services to a new community care delivery model (Buckmaster, 2017). A further implication arising from the introduction of the NDIS was an alteration in the makeup of the ID workforce, particularly a dynamic shift in the nature and activity of the nursing workforce, where the speciality of disability nursing has stalled (Lewis et al., 2019; Trollor et al., 2016, 2018; Wilson, Howie, & Atkins, 2019). The nature of complex health conditions associated with ID frequently increases the health demands for people with disabilities, who often need high levels of health care from hospital and community health services. Despite the high care needs of many people with IDs, nursing preregistration programmes do not adequately include ID care within the nursing curriculum (Lewis et al., 2019; Trollor et al., 2016, 2018; Wilson, Howie, & Atkins, 2019). As a result, nurses feel unprepared, without suitable education and training to deliver safe care in this context (Lewis et al., 2019; Trollor et al., 2016, 2018; Wilson, Howie, & Atkins, 2019).
The absence of a specialised field in disability nursing has overlooked the health care, recovery and well-being needs of people with IDs. There has been a resultant pause in disability nursing advocacy within the health, social care and education sectors and a lag in leadership arising following the adoption of a national nursing curriculum (Furst & Salvador-Carulla, 2019; Lewis et al., 2019; Trollor et al., 2016, 2018; Wilson, Howie, & Atkins, 2019). The absence of leadership and advocacy has meant that the needs of people with IDs have been generally overlooked in the nursing discipline (Furst & Salvador-Carulla, 2019; Lewis et al., 2019; Trollor et al., 2016, 2018; Wilson, Howie, & Atkins, 2019). With 3% of the population impacted, nurses will likely encounter people with IDs at some point in their practice in any setting. Therefore, our nurses must be adequately educated to care for this priority population.
A National survey among Australian nurses revealed a high percentage of older (M = 52.31, SD = 10.05) and female nurses (n = 78) working in the disability sector (Lewis et al., 2020). This age is higher than the average age of all nurses working in the UK, USA, Canada and Australia. This is concerning because this aging workforce with specialised training in ID will continue to decrease in number and may not be replaced by nurses qualified to care for people with IDs. Lack of interest in joining the ID workforce is primarily contributed by the absence of an ID nursing speciality, lack of ID content in undergraduate programmes and absence of clinical placement opportunities in the ID area (Lewis et al., 2020).
This is significant because governmental policy changes related to the public care of people with IDs inherently affect the quality, quantity and safe delivery of care provided in hospital and community settings. Later sequelae from these changes result in a reduction in the supply chain of suitably prepared nurses to carry out the specialist healthcare needs of people with IDs, with university nursing schools opting to squeeze out ID nursing knowledge from the comprehensive curriculum to make room for other topic areas (Furst & Salvador-Carulla, 2019; Lewis et al., 2019; Trollor et al., 2016, 2018; Wilson, Howie, & Atkins, 2019). Previous reviews, including studies by Jaques et al. (2018), Taua et al. (2012) and Lewis et al. (2019), which focused on the roles and experiences of nurses in caring for people with ID, along with research by Lacono et al. (2014) exploring hospital experiences of individuals with ID, have provided valuable insights into specific aspects. However, despite these contributions, there remains a significant gap in understanding the nuanced factors related to care quality and nursing education within the context of IDs. In contrast to prior literature reviews that mainly concentrated on global sources, our review adopts a focused strategy, specifically analysing Australian literature within a defined time frame following the 2012 move to national registration of nurses and the associated shift to accrediting preregistration nursing courses nationally. This focused strategy enables us to comprehensively grasp the contextual evolution of disability nursing within a specific timeline.
2 Definitions
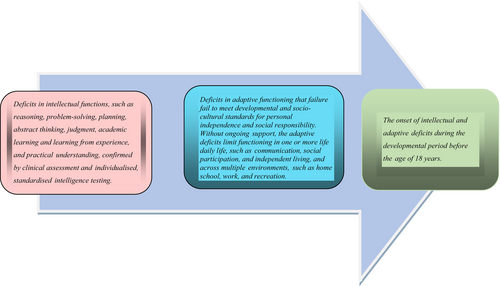
Intellectual disability (ID), as defined by the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM–5; American Psychiatric Association, 2022), is a neurodevelopmental disorder characterised by intellectual and adaptive functioning deficits across conceptual, social and practical domains. These deficits typically manifest during the developmental period and are marked by limitations compared with individuals of the same age, gender and social-cultural background (DSM-5). The DSM-5 criteria for ID are illustrated in Figure 1.
3 Methods
3.1 Aim
An integrative literature review was conducted to collect all available literature to illuminate what is known about the quality of nursing care and educational preparedness for ID nursing practice in Australia.
3.2 Review Questions
- What is known about the quality of nursing care of people with IDs in Australia across the last 13 years (2010–2023)?
- What is known about nursing education and preparedness to care for people with IDs safely?
4 Search Strategy
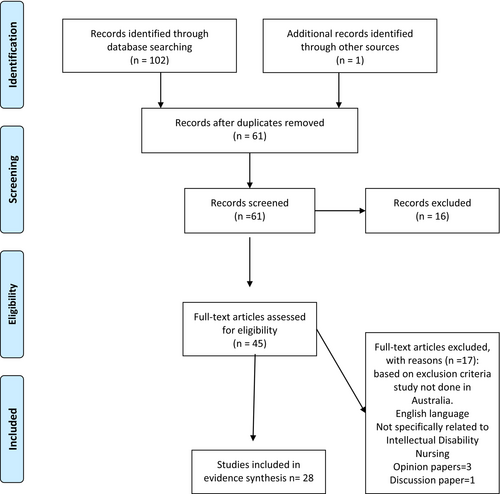
We followed the PRISMA framework (Page et al., 2021). Table S1 contains the completed PRISMA checklist for reference. Integrative literature was selected because it included a wide range of literature, study types and any relevant reports that would inform the review question. Theoretical and policy articles and reports were also included in the review. Opinion and discussion papers were excluded from the review. Because of the paucity of literature on ID nursing, the search was supplemented with hand-searching of reference lists. Five electronic databases were systematically searched: CINAHL, MEDLINE, PsycINFO, Scopus and Cochrane Library. The search terms can be found in Table 1.
| Population | Context 1 nursing | Context 2 setting | ||
|---|---|---|---|---|
|
“Intellectual disability*” OR “developmental disability*” OR “learning disability*” OR “neurodevelopmental disorder*” |
AND |
“delivery of care” OR “nursing workforce” OR “disability nursing” OR “nursing practice” OR “nursing role” OR “nursing skills” OR “education nursing” OR “nurse education” |
AND |
Australia* OR “New South Wales” OR Queensland OR “northern territory” OR “Western Australia*” OR “South Australia*” OR Victoria* OR Tasmania* OR “Australian capital territory”. |
The search inclusion criteria included peer-reviewed English articles published between January 2010 and August 2023. The period is aligned with the 2012 move to national registration of nurses and the associated shift to accrediting preregistration nursing courses nationally.
A total of 28 articles were located and retrieved from the combined databases. Figure 2 provides a PRISMA flow chart (Page et al., 2021) of the search process. A total of 28 articles were reviewed and were independently considered relevant by an experienced team of researchers. Each article was read in-depth, and data were extracted following a format developed for the study (Table 2). We then coded this data systematically, using descriptive labels to categorise and organise similar information across studies. Through an iterative process of review and refinement, we identified overarching themes that emerged consistently across the included literature. These themes were carefully defined, named and described in detail, with supporting evidence from the original studies. Finally, we interpreted these themes about our research question, synthesising the findings to draw meaningful conclusions and insights.
| SL No | Author/Country – First Author | Year | Main issue/research question | Type of the study | No. of participants/no studies | Main findings | Recommendations | Limitations |
|---|---|---|---|---|---|---|---|---|
| 1 | Lewis et al./Australia | 2019 | Nurses' experience of caring for people with intellectual disabilities in the acute setting |
Literature review (2006–2015) |
14 papers (3 Australia) |
Nurses were unprepared Poor communication, the ambiguous expectations of carers and reliance on paid/unpaid caregivers were reported |
Nursing education should include enough opportunities to develop communication skills with people with ID and practical experience Recommend strategies for a therapeutic relationship with carers promoting the collaborating relationship |
Most studies in the United Kingdom Only three studies from Australia |
| 2 | Wilson et al./Australia | 2019a | Make a series of recommendations concerning the educational preparation required for nurses to meet future health, aged care and disability needs of the Australian community, including clinical training |
Professional Association of Nurses in developmental disability (PANDDA) Australia report |
NA |
People with ID experience poor health outcomes reduced physical health, and poor accessibility to health services 38% of deaths (over 6 years from 2005 to 2011) were avoidable, and there is a 26-year gap in life expectancy Higher risk for heart disease, high blood pressure, obesity, poor oral health and respiratory diseases Four domains of the roles of nurses were identified: direct health care, teaching and coaching, advocacy and case coordination and education, research and evaluation to ensure evidence-based practice Communication problems and the capacity to take consent is an area of concern The increasing aging population of ID and age-related issues Existing knowledge gap, abysmal administration of ID content in university Building a workforce is essential |
Dedicate content within the national undergraduate nursing curricula either in the form of a standalone unit of study or embedded within a team (chronic illness and disability) ID is embedded in the NMBA RN standards Clinical placement opportunities where student nurses care for people with ID Development of a fourth-year-embedded honour component for interested and capable students who can combine a small research study with their new graduate year |
Not listed |
| 3 | Wilson et al./Australia | 2019b | How can existing speciality practice standards inform the development of speciality practice standards for intellectual and developmental disability nurses? |
Descriptive design Web search |
33 speciality practice standards that are published | Sixty-nine specialist nursing associations in Australia have publicly accessible specialty practice standards. The content of these standards can be categorised in six primary ways, which reflect the definite organisation of the Nursing and Midwifery Board of Australia practice standards. This suggests that nursing is a unifying identifier in the context of superficially disparate subspeciality areas of practice. Therefore, existing nursing practice standards can inform the development of new practice standards for specialist intellectual and developmental disability nurses |
Newly developed speciality practice standards need to reflect the beliefs and values about nursing prescribed in the Nursing and Midwifery Board of Australia standards Explore the omission of speciality practice standards for 52% of the specialities identified Development of consistent language in the standards for better articulation Newly developed specialty practice standards that reflect the beliefs and values about nursing prescribed in the NMBA standards |
Only speciality areas are taken which had an accessible and published nursing standard |
| 4 | O'Reilly et al./Australia | 2018 |
What professional and published policy developments have shaped ongoing changes in the conceptualisation and practice of nursing people with ID? How has the delivery of education and development of practice standards for nurses in the specialist area of ID changed over time? What can be learned from the past to inform the future development of the specialist area of nursing people with ID? |
Systematic literature review (30 years) 1986–2017 |
66 |
Lack of evidence to inform ID nurse practice, guidelines and policies The greater life expectancy of people with ID means their health issues are becoming more complex and intractable People with ID have significant health disparities compared with the general population Nurses with expertise in caring for people with ID continue to be needed despite deliberate policy changes |
Reintroduction of The Specialisation of ID Nursing in the Australian Context |
Only one study from Australia Limited to the published literature and the potential exclusion of articles that may have been about ID nursing Some areas of ID nursing are likely missed, such as the published literature on ID nursing history or ID nursing research |
| 5 | Trollor et al./Australia | 2018 | Determine how intellectual disability content is taught within Australian nursing schools | Two-phase audit using interviews and online survey |
Phase 1 31-course coordinators from schools Phase 2 15-course coordinators |
Over half of the universities are not providing ID content Across 15 schools offering ID content, lectures were the most common method (82%), followed by tutorials (59%), workshops (26%) and other methods (e-learning 12%). Approximately three-quarters of intellectual disability teaching uses some problem or inquiry-based learning. Only one school involved a person with ID. Six (19%) schools identified staff specialising in ID, and 7 (23%) identified staff with declared interest |
It would be valuable to ask curriculum coordinators for more details on teaching methods used and how people with ID were involved in teaching, the professional background of educators and whether there was an opportunity for interprofessional education Review the teaching methods and develop guidelines to encourage using strategies that foster learner-centred education, practical skill development and inclusive teaching |
The definition of units of study varies across nursing schools, so it is not easy to compare curricula across universities directly It was impossible to determine if the information provided online was complete or if forced-choice questions may not have allowed participants to provide responses that accurately represented their practice |
| 6 | Jaques et al./Australia | 2018 | Identify the specialist roles that nurses perform and the specialist skills that nurses use when caring for people with intellectual disabilities |
A Review of the Literature 2000–2017 |
27 articles |
Similarities exist between the physical care delivered to people with ID and those with an intellectual disability However, skills in communication, advocacy and person-centred care differ between these groups The skill set of ID nurses is not uniquely technical but is uniquely relational Because of the communication challenges, ID nurses should be proactive with their clients. This incorporates increased patience and resilience when developing relationships with those they care for |
There is a need for further research into how ID-specific nursing skills are unique Development of nursing policy and practice so that nurses working with clients with ID can begin to be recognised and valued for their work and roles |
A limited number of studies identified what is unique about the performance of the role of specialised intellectual disability nurses, especially in Australia |
| 7 | Wilson et al./Australia | 2019c |
Explore the perception of Australian nurses working in disability-specific settings on roles about 1. nursing people with an intellectual and developmental disability living in Sydney 2. Utility and applicability of professional practice standards explicitly designed for intellectual and developmental disability nursing |
Qualitative design Thematic analysis |
18 |
Three themes were identified: a unique investment in the nurse/patient dyad, a bridge between disparate systems and an ambiguous future Nurses reported a variable understanding of professional practice standards designed for intellectual and developmental disability nursing but also a belief in their importance |
A robust empirical research base is needed to support the leadership and advocacy activities to be undertaken by nurses on behalf of people with ID A research evidence base will also require the development of education programmes for nurses that equip nurses more thoroughly for practice with people with ID and the skills to engage in rigorous enquiry about their health, well-being and care It is necessary to develop ID nursing practice standards for Australian nurses that articulate their unique roles |
|
| 8 | Furst et al./Australia | 2019 | Identify education in the health care of persons with ID available to nursing students and registered nurses within the current Australian model concerning NSW and Tasmania | Systematic mapping and documentary analysis | 12 |
Minimal educational content relating to the health needs of people with ID was found in the academic programmes It was inconsistently applied where it existed, being made available as an aspect of professional development rather than an identified educational pathway |
Mandatory inclusion of ID health in undergraduate nursing curricula Development of a framework for competencies for nurses working with persons with ID drawing on specialist nursing sources Inclusion of persons with ID in the development of resources and teaching A database of resources available to nurses as professional development Development of a career pathway for those wishing to specialise in the health of persons with ID Inclusion of the needs of persons with ID in all disability health education policies and planning |
Scarcity of scientific literature about ID nurse education in Australia The number of modules and educational programmes in the two states analysed in the paper is deficient |
| 9 | Edmonds et al./Australia | 2016 | Determine whether registered nurse Australian specialty competency standards identified unique capabilities of nursing practice | Content analysis to cross-map the standards to the national standard domain of professional practice, critical thinking and research, provision and coordination of care and collaborative and therapeutic practice | 28 sources speciality standards | Of the 28 sourced speciality standards, only the nursing informatics standards displayed unique elements of nursing practice. Other nursing capabilities, such as leadership and person-centred care, were prominent in speciality standards while more challenging to interpret in the national averages. In addition, developmental and intellectual disability nursing was not evident in the national competency standards | Specific performance indicators of how the registered nurse standards are applied in the speciality context are developed in place of multiple speciality standards | Identifying every eligible speciality competency standard was impossible as many were not publicly available and only accessible through membership fees |
| 10 |
Douglas et al. Australia |
2016 | Support needs of parents of a child with ID (0–12 months) | Qualitative descriptive design |
11 interviews Three parents Victoria, Australia |
Parents need assistance with adjusting to diagnosis and implication Knowledge/information Connecting with other parents The nurse can enable connecting with parents |
Need for policy and guidelines to support holistic nursing care |
Small sample One region in Australia Mothers voice dominant We need to hear from fathers and culturally and linguistically diverse groups |
| 11 | Trollor et al./Australia | 2016 | Establish the quantity and the nature of intellectual disability content offered within Australian nursing curricula | Two-phase audit using interviews and online survey |
Phase 1- 31-course coordinators from schools Phases 2–15 |
Over half of the schools offered no intellectual disability content. Alternatively, in units of study that contained some auditable ID content, the area was taught an average of 3.6 h per unit of study. Units were evenly distributed across the 3 years of study. Three schools offered 50% of all units audited. Clinical assessment skills, ethics and legal issues were most frequently taught where human rights issues and preventative health were poorly represented. Only one school involved a person with an ID | Australian and international nursing schools respond by reviewing their curricula to ensure nurses receive an education that covers all the major topic areas mentioned above and the consistent content and principle-based |
Researchers cannot be sure that the ID content figures were not inflated or that the information and details were complete Almost all data were collected through the mail; this may have reduced the participant's enjoyment due to survey fatigue There was inconsistency in the course type and structure and variable definition of study, which made it challenging to directly compare the proportion of the curriculum dedicated to ID content across nursing schools |
| 12 | Williams et al./Australia | 2015 |
The empathetic attitude of undergraduate paramedic and nursing students towards four medical conditions To find how a group of paramedic students and nursing and paramedic double-degree students show differences in attitude towards four medical conditions and note changes occur through their education |
A prospective cross-sectional longitudinal study | 554 |
A statistically significant difference was found between double-degree and single-degree students, year of course and gender for patients with substance abuse Similar results were found with ID and attempted suicide No statistically significant difference with acute mental illness Double-degree students have less regard for ID but have increased consideration this past year Females have high regard for all conditions |
Nil |
Convenience sampling, hence less representative Volunteers who may be more academically inclined or proactive learners may introduce study bias Students tend to reply in a socially desirable manner |
| 13 | Lacono et al./Australia | 2014 | Hospital experience of people with ID | Literature review (2009–13) | 16 papers |
Fear of hospital encounter by people with ID Failure of staff to provide care Lack of knowledge and skills of hospital staff Poor and negative attitude by hospital staff towards people with ID Staff or system failure to adjust to the needs of people with ID Over-reliance by the team on family or paid caregivers The presence of a hospital liaison person Hospital policies and systems to address the needs of ID willingness of staff to go beyond the call of duty to ensure communication and markets Parents of children with ID have poor hospital experiences |
Further research is needed to understand the specific needs for each episode for patient care and staff Hospital-based care Include diverse disability |
Most of the literature is from the United Kingdom |
| 14 | Taua et al./Australia | 2012 | Nurses' role in caring for people with a comorbidity of mental illness and intellectual disability |
Literature review integrated 2000–2010 |
21 | The roles identified are advocacy, /health promotion, assessment, behavioural interventions, communication, leadership and nurse's position within the multidisciplinary team, medication administration, safety and risk management |
Need significant improvement in health screening Education and training of the workforce to understand and respond to those complexities of ID The knowledge base of staff critical Advanced knowledge and skills are required due to the complexity of care |
Lack of quality research studies Different methodologies make comparison difficult No replications A relatively small number of articles was found; none were excluded, therefore a chance for bias |
| 15 | McKenna et al./Australia | 2012 | Assess the level of empathy and regard for specific medical conditions in undergraduate nursing students | Cross-sectional study | 106 |
There was no statistically significant difference among the years of study, age group and gender Favourable attitude towards intellectual disability, chronic pain, acute mental illness and terminal illness Significantly lower regard towards substance abuse |
A longitudinal study to track student empathy Studies that involve other attributes, such as communication and listening style, can be explored to develop an overall picture of how nurses engage with their patients |
The ability to analyse the variance between empathy and year of Bachelor nursing is limited as the number of first-year students is too low (n = 3) Why students have a less favourable attitude towards substance abuse is not elicited Tools do not measure the participant's behaviour or empathy but only state intent The self-report measure has a chance for bias Convenience sampling, hence the results are not generalisable |
| 16 | Hemsley et al./Australia | 2011 | Role of paid caregivers supporting adults with ID and complex communication needs | Qualitative narrative analysis |
15 adults with ID 15 paid cares 15 hospital nurses |
Paid caregivers are essential in supporting ID, providing information, delivering primary care and communicating Reflected paid care giver's volunteerism, lack of orientation of carers and hospital staff to paid care roles, and blurred boundaries between paid care, family care and nurses Paid caregivers uncertain about their responsibility for staff and patient safety |
New policies and practice guidelines are needed to guide both health and disability services in clarifying paid care's roles and role boundaries and to enable paid carers and hospital staff to work together effectively Further research on the income range of paid caregivers shows this plays a part in the increased responsibility for patient safety Develop theory on social, political and workforce issues, including funding demands for delivering community-based paediatric care |
Only 15 participants—not possible to generalise The second interview with only five participants would have been conducted among all for additional insights |
| 17 | Hemsley et al./Australia | 2012 | Investigate nurses' expressed concept of time in stories about communicating with patients with developmental disabilities and complex communication needs in the hospital | Narrative enquiry | 15 nurses | Nurses identified time as a barrier and facilitator to successful communication with patients. A barrier was thematically related to avoiding direct contact with the patients and preferring to communicate with family or paid caregivers. Time as a facilitator was related to valuing communication, investing extra time and applying a range of adaptive communication strategies to establish communication |
Observational studies of the interaction between nurses and patients with DD and complex communication needs might provide helpful information on the relationship between the frequency and duration of interactions and success in communication Research on how the complete application of strategies outlined by Fink et al., along with support by hospital policy and action, might save nurses time and improve the care of patients with DD and CCN in a hospital |
Time is perceptual and relative; nurses were not asked to focus specifically on the amount of time, and discussion is limited to time, which limits comparison around groups The small number and limited generalisation The second interview was only with seven nurses. If interviewed for a second time, more insights would have been gained |
| 18 | Goddard et al./Australia | 2010 |
Create a functional clinical placement model in intellectual disability in a baccalaureate nursing programme Promote the health and well-being of families through a partnership health mentoring model focusing on the strengths of all participants |
Action research |
Five families of children with disability Nine nursing students And 2-nurse academics |
The key themes were increased awareness, valuing of the health needs of families and understanding Community-focused professional experience placement effectively achieves the competency-based learning outcome required of undergraduate nursing students |
Research needs to be carried out to investigate whether the project has the potential for more comprehensive application into other disciplines involved with families of children with ID |
The project is context-specific, focusing on families of children with intellectual disabilities The project is resource-intensive |
| 19 | Cashin et al./Australia | 2022b | Survey the educational experience of registered nurses in hospital and community-based health care settings in Australia | A cross-sectional descriptive survey | 639 nurses |
Poor educational preparation related to intellectual disability and autism: 68.5% of nurses reported no content on intellectual disability, and autism was included in their undergraduate curriculum. Most (80.8%) did not have a clinical placement dedicated to caring for people with intellectual disabilities, 65.2% of respondents had not taken any ID-related CPD, 55.7% of nurses reported they were somewhat knowledgeable, and 60% said they were confident The highest level of comfort was reported related to discussing a person's disability with another health professional, establishing a therapeutic relationship, establishing treatment procedures and communicating. The lower level of comfort with referring families to ID/ASD resources, communicating with people who use nonverbal communication and de-escalating behaviour Students who had clinical placement had high knowledge, confidence and comfort |
Include ASD and ID content in the curriculum in the preregistration curriculum Recommendation for dedicated clinical placements Assessment with a focus on ASD or ID |
The sample was based on self-selection Findings related to education preparation were based on the recollection of nurses |
| 20 | Lewis et al./Australia | 2020 | Describe the demographic profile of the workforce in intellectual disability in Australia | Descriptive cross-sectional survey design | 101 nurses | Most of the nurses were females, and the mean age was 55–59 (mean age 52.31 SD = 10.05) 0.88 nurses were RNs, and the remaining was EN. Eighty-five nurses worked directly with people with ID, reporting at least some ID experience. Seventy-one nurses were working full-time, 22 were part-time, and the remaining were casual employees. 50% of the sample had specialist qualifications in ID-specific content. They mainly reported completed Mental Retardation Nursing certificate (N = 12), which was discontinued in 1985 |
Reintroduction of ID nursing content in the undergraduate curriculum Establishment of a widely accessible PG programme for nursing people with ID |
Not reported |
| 21 | Foo et al./Australia | 2021 | To explore the experience of specialist palliative care staff in talking with people with ID regarding dying and death and factors that influence this conversation | AN inductive thematic analysis | 20 palliative care staff (nurse, physician and occupational therapist, family worker, music therapist, social worker) | The experience of staff talking with people with ID varies from no or indirect conversation to explicit conversation with the patient. The conversation was based on the perceived capacity of the patient with ID to understand the concept of death and dying, communication ability and ability to cope with discussions. Staff who had undertaken special training in ID were likelier to converse about death and dying |
They recommended developing communications guidelines, resources and training for palliative care teams More comprehensive research on the needs of people with ID and their caregivers in palliative care is needed, particularly emphasising communication around death and dying. Prior training demonstrated greater confidence, and staff with great rapport and familiarity with the patient showed a higher ability to talk about death and dying |
A self-selecting nature might have influenced results The qualitative nature of the study reflects the participants' personal experience, which may not be generalisable |
| 22 | Hurley et al./Australia | 2021 | To better understand the lived experience of carers and families of persons with a disability after entering NDIS and following the 18 months | A longitudinal qualitative study |
72 caregivers NSW |
Carers' well-being score remained below the recommended cut-off. There was a reported increase in the carer's self-care strategies supported by a reduction in caring responsibilities with additional free time. Some carers reported reduced financial pressures 28% of the carers reported satisfaction with the NDIS workforce. But the majority reported a need for improvement in technical and nontechnical skills, such as the need for staff with expertise in disability (26%) |
Recommended support to reduce time spent caring Offer individual wellness and recovery action plans for carers Educational institutions such as universities and TAFE establish specialised support for carers entering higher education Cares need to have more opportunities to meet with NDIS planners Every disability support worker requires formal training at least certificate IV levels. The curriculum should include nontechnical skills such as empathy. Self-awareness, communication, team working and reflection and value-based behaviours and disability-specific knowledge. Capabilities in the therapeutic use of self-care also should be included Further research is needed to understand how to influence better the health and well-being of carers of a person with a disability |
|
| 23 | Lewis et al./Australia | 2021 | Compare the service engagement at the time of diagnostic assessment at the Disability specialist unit across CALD and non-ALD groups in a retrospective record rev. View |
Retrospective Audit |
43 45 NSW Children with a developmental disability |
Considering that a large percentage (21%) speak a language other than English, it significantly impacts service delivery. The cultural and social barriers they encounter while accessing and utilising services are enormous, further complicated by Australia's fragmented delivery of services. It is reported that there is an observed trend where children from CALD backgrounds are less likely to access therapy services when compared to children from a non-CALD experience and require more referrals to access NDIS. Interestingly, children from CALD backgrounds are significantly more likely to receive a diagnosis of GDD/ID and ASD. Children are accessing services for diagnosis after 4 years, which is a concern as the early intervention could be started earlier than that, which may be further delayed due to delay in the referral, which will delay the more targeted interventions for the child | Further research needed with a focus on the targeted cultural group may be required to identify the cultural barriers to inform the policies and management pathway; it is recommended that adjustment to the referral pathways, simultaneous referral to NDIS and translation services, and availability of developmental disability information sheet in broader language, and designating CAD as risk factor a prioritising the services and incorporating social work support would be beneficial for a more equitable service (Lewis, 2021) |
The study definition of CALD as a LoTE speaking at home needs to be more complex and might have failed to compute influences outside the language difference The population of CALD is probably under-represented CALD data were analysed at the single group level, likely to mask significant differences between communities The potentiality for not controlling confounding barriers in the study contributed to service engagement |
| 24 | Wilson et al./Australia | 2020 | To describe the roles that Australian nurses play, the breadth of skills that they deploy and the range of contexts in which they practice | Cross-sectional study using descriptive survey |
101 nurses 78 females 22 males |
The primary focus of roles was direct assessment and care of people with ID, followed by supervision of support workers, education and advocacy of people with ID Most nursing practice involves meeting gastrointestinal, neurological and sensory care. Genito urinary care and sexual care were the less frequent. Seizure management is the most common care provided Adaptive behaviour: Communication and social skills were the most endorsed items, followed by personal living: motor skills and community living skills The most frequently provided support was behavioural support for self-harm and harm to others Anxiety and depression were the most supported areas of care, and support for suicidality was the least likely to provide support |
More focused research is recommended on the economic benefits of disability service employing nurses and the description and effect of nursing interventions specific to people with ID New NDIS-ready models of nursing care for people with ID are recommended for further development and advancement Extant models of specialist practice in the UK and Ireland could combine with those in Australia |
Inconsistent responses across different geographical locations limit generalisability Recruitment from the NDIS service provider list might have excluded some prospective participants Interpretation of data may be limited due to the cross-sectional design adopted for the study |
| 25 | Desroches et al./United States | 2022 |
What are the most significant challenges to ID nurses across the globe in meeting the care needs of people with ID 1 year into the COVID-19 pandemic? How much and what types of support are nurses receiving within their organisations? What challenges and strategies employed to overcome these challenges are reported by nurses related to enacting COVID-19 guidelines during the pandemic? |
A convergent mixed-methods design |
369 nurses United States (n = 255), Canada (n = 5), United Kingdom (n = 11), Ireland (n = 14), Australia (n = 12), New Zealand (n = 9) |
Nurses faced four main challenges while caring for people with ID: (1) Socialisation, meaningful activity and mental/behavioural health; (2) understanding and complying with COVID-19 guidelines; (3) access to, quality of and continuity of care; and (4) COVID fatigue and the influence of time. The isolation of adults with intellectual disabilities from family and friends due to social distancing guidelines and disruption of daily activities, day programmes and work affects their mental health Several technology-related challenges are faced by people with ID while using telehealth as an alternative option, especially with complex needs requiring face-to-face consultation. In acute care, masks and the need for a support person have complicated the care received. Staff shortage was another challenge globally, with increased reliance on unqualified and unmotivated staff |
There is a need for a better understanding and promotion of a person-centred approach and safe telehealth options More research with appropriate international representation is required to understand nurses' challenges during public health crises. Including countries where ID nursing speciality exists would be suitable for comparison Research is needed to compare COVID-19 policy responses and outcomes for people with ID across countries and settings Interventions are needed to support people with ID to cope with pandemic-related changes and improve mental health and well-being There is a need to strengthen public health services concerning preparation and education about the needs of people with ID |
They limited demographic information from nurses, including gender or racial information Most participants were from the USA, limiting statistical cross-country comparisons. The study captured nurses' responses simultaneously; there may be possible variation based on differences in COVID-19 severity and public health response |
| 26 | Desroches et al./USA | 2021 |
1. Do Australian nurses' attitudes and emotions significantly differ between caring for adults with an intellectual disability versus physical disability? 2. Do nurses' attitudes and emotions towards caring for adults with intellectual disabilities significantly differ between Australian mainstream and intellectual disability nurses? 3. What factors predict Australian nurses' attitudes and emotions towards caring for adults with ID? |
A cross-sectional correlational predictive replication study | 115 nurses and endorses nurses 108 registered nurses |
Nurses held more positive attitudes towards caring for an adult with a physical disability (median = 634) than an intellectual disability (median = 567), Z = −5.473, p = 0.000. There are no statistically significant differences in nurses' positive and negative emotion scores between physical disability and intellectual disability conditions Intellectual disability nurses and mainstream nurses reveal that intellectual disability nurses experience a greater frequency of positive emotions towards caring for adults with intellectual disability (median = 180) than mainstream nurses (median = 153), U = 941.5, p = 0.013. No statistically significant differences in attitude or negative emotions were found between intellectual disability nurses and mainstream nurses |
There should be strategies to support all nurses to improve outcomes for adults with intellectual disabilities, which nurses should initiate All students should be taught about ID content in their UG curriculum with clinical placement opportunities. People with ID can be included in the education programme to deliver some content. Practising nurses should participate in disability awareness training underpinned by values of human dignity, inclusion and respect for autonomy. Researchers should evaluate these strategies to continue building the evidence base |
As with any cross-sectional study, there are limitations with generalisability. A proportionate representation was only achieved across some states and territories, with Victoria standing out as under-represented Self-reporting limited comparison of responders and nonresponders There may be confounding variables, such as the practice context, which should have been explored in the study |
| 27 | Cashin et al./Australia | 2022a | To compare the self-perceived preparedness, knowledge, comfort and confidence of Australian Registered Nurses when caring for people with ID and ASD across contexts of practice: primary care and community, intensive care, acute hospital, emergency department, paediatrics and ID/ASD | Cross-sectional descriptive study | 693 |
The mean age of nurses working in ID/ASD is 49.5 (SD = 12.4), which was high compared with people working in paediatrics, acute care, ED and ICU. Most of the nurses working in the ID sector were females (88.6%) A significant proportion of educational content and opportunities than any other area of nursing suggests that working in the ID/ASD context is associated with educational content and exposure Additionally, ID/ASD nurses reported feeling significantly more prepared when compared to all other practice contexts ID/ASD nurses reported the highest levels of comfort across all domains; in contrast, ICU nurses reported the lowest levels across all eight disciplines |
CPD must be offered to all nurses in all practice contexts to improve self-reported knowledge and confidence in working with people with ID and ASD. This content needs to be designed to meet the specific needs of nurses in each practice context. Further study indicates that it moves beyond self-reporting knowledge to determine the knowledge level of practising nurses working with people with ID and ASD | Not reported |
| 28 | Mimmo et al./Australia | 2022 | To understand what constitutes a good experience of care for inpatient children and young people with intellectual disabilities as perceived by nursing staff | Interpretive qualitative study | 29 nurses |
The study identified six themes mentioned in the conceptual components: use rapport, know the child, negotiate roles, shared learning, build trust and relationships, and past experiences. Three new themes were identified: the unique position of a paediatric nurse, joy and job satisfaction Participants agreed that using rapport to build familiarity with a child or young person (CYP) with an intellectual disability helped the child feel safe and comfortable in the hospital. The groups identified the importance of nurses using play and rapport to form connections with CYP, where they had had some distressing experiences |
The model in the study can be used as a practical guide for new graduate nurses and serve as a framework for nurse managers and policymakers to advocate and assess the ward's requirements and develop policies and procedures for guiding staff in care delivery |
The study was conducted in the two tertiary childrens hospitals in the city. So, experiences of paediatric nurses working in children's wards in adult tertiary or district hospitals or experienced nurses who are not frequently exposed to CYP with intellectual disability may have different perspectives not captured in the study The study was conducted during the COVID-19 pandemic, which might have affected the participants' stories |
5 Results
An integrative literature review examined the state of disability nursing practice in Australia following the implementation of the National Disability Insurance Support (NDIS) scheme. A total of 28 articles were considered eligible for inclusion in this study.
Table 2 presents a comprehensive overview of the relevant articles included in the review. Because of the limited availability of literature on this topic, all types of articles were included, following the methodology of an integrative literature review. The dataset comprised literature reviews (n = 5), qualitative studies (n = 8), descriptive and correlation studies (n = 7), mixed-method research (n = 1), web searches or document analyses (n = 3), audits (n = 3) and one report (n = 1). Details of the studies are included in Table 3.
| Types of study | Number of papers | Authors |
|---|---|---|
| Literature reviews | 5 | Jaques et al. (2018), Lacono et al. (2014), Lewis et al. (2019), O'Reilly et al. (2018) and Taua et al. (2012) |
| Qualitative studies | 8 | Douglas et al. (2016), Foo et al. (2021), Goddard et al. (2010), Hemsley et al. (2011, 2012), Hurley and Hutchinson (2022), Mimmo et al. (2022) and Wilson, Wiese, et al. (2019) |
| Descriptive and correlation studies | 7 | Cashin, Pracilio, et al. (2022), Cashin, Buckley, et al. (2022), Desroches et al. (2021), Lewis et al. (2020), McKenna et al. (2012) and Williams et al. (2015, 2020) |
| Mixed-method research | 1 | Desroches et al. (2022) |
| Audits. web searches or document analyses | 6 | Edmonds et al. (2016), Furst and Salvador-Carulla (2019), Lewis (2021), Trollor et al. (2016, 2018) and Wilson, Lewis, et al. (2019) |
| Report | 1 | Wilson et al. (2019a) |
Interestingly, the Australian literature review has focused on international collective findings (Jaques et al., 2018; Lacono et al., 2014; Lewis et al., 2019). A literature review from an Australian perspective relies more on international literature (Jaques et al., 2018; Lacono et al., 2014; Lewis et al., 2019).
The primary subthemes identified in qualitative studies revolve around the experiences of families and children (Douglas et al., 2016; Hurley & Hutchinson, 2022; Lacono et al., 2014; Mimmo et al., 2022). In addition, there is a blend of other themes encompassing workforce development (Goddard et al., 2010; Hemsley et al., 2011, 2012), including professional standards (Wilson, Wiese, et al., 2019). Lastly, there is a focus on the needs of adults with IDs and the palliative care requirements of individuals with IDs (Foo et al., 2021; Lewis et al., 2019).
The primary themes found in quantitative studies encompass workforce development and practice standards (Cashin, Buckley, et al., 2022; Cashin, Pracilio, et al., 2022; Lewis et al., 2020; Wilson et al., 2020; Wilson, Lewis, et al., 2019). Furthermore, these studies delve into curriculum-related aspects, emphasising nurturing attitudes within an educational context (McKenna et al., 2012; Williams et al., 2015). The studies also explored nurses' attitudes as a key theme (Desroches et al., 2021; Williams et al., 2015).
The audits and document analyses primarily focused on examining nursing curricula, disability content, competency standards and participant experiences (Edmonds et al., 2016; Furst & Salvador-Carulla, 2019; Lewis et al., 2019; O'Reilly et al., 2018; Trollor et al., 2016, 2018; Wilson, Howie, & Atkins, 2019). Although mixed-methods studies were relatively scarce, one study specifically delved into primary care within the context of the COVID-19 pandemic (Desroches et al., 2022). This study specifically explored the challenges faced by specialist ID nurses in primary care settings while providing care to individuals with IDs during the pandemic (Desroches et al., 2022).
The reviewed literature identified three main themes, including (1) workforce development and professional standards, (2) hospital experience and support needs of individuals with IDs and (3) nursing curriculum and ID. Table 4 summarises themes, subthemes and the corresponding studies.
| Themes | Subthemes | References |
|---|---|---|
| Theme 1: Workforce development and professional standards | Lack of preparation of nurses | Cashin, Pracilio, et al. (2022), Cashin, Buckley, et al. (2022), Desroches et al. (2022), Foo et al. (2021), Furst and Salvador-Carulla (2019), Hurley and Hutchinson (2022), Hemsley et al. (2011, 2012), Jaques et al. (2018), Lewis et al. (2020), Lewis et al. (2019), Lacono et al. (2014), O'Reilly et al. (2018), Taua et al. (2012), Mimmo et al. (2022), Wilson, Howie, and Atkins (2019) and Wilson, Wiese, et al. (2019) |
| Poor communication between nurses and people with intellectual disability | Foo et al. (2021), Hemsley et al. (2012), Jaques et al. (2018), Lewis et al. (2019) and Wilson, Howie, and Atkins (2019) | |
| Reliance on paid/unpaid caregivers. | Cashin, Pracilio, et al. (2022), Hemsley et al. (2011), Lewis et al. (2019) and Lacono et al. (2014) | |
| Training needs in ID care | Cashin, Buckley, et al. (2022), Furst and Salvador-Carulla (2019), Hemsley et al. (2011), Lacono et al. (2014), Lewis et al. (2020) and Wilson, Howie, and Atkins (2019) | |
| Professional standards | Edmonds et al. (2016), Wilson, Lewis, et al. (2019) and Wilson, Wiese, et al. (2019) | |
| Role of nurses | Taua et al. (2012), Mimmo et al. (2022), Wilson, Wiese, et al. (2019) and Wilson et al. (2020) | |
|
Theme 2: Hospital experience and support needs of individuals with intellectual disabilities |
Support needs of parents/carers/CALD population | Douglas et al. (2016), Desroches et al. (2021), Hurley and Hutchinson (2022), Lacono et al. (2014) and Mimmo et al. (2022) |
| Attitude of nurses | Desroches et al. (2022), Lacono et al. (2014) and Mimmo et al. (2022) | |
| Fear of hospital encounter | Lacono et al. (2014) | |
| Role of paid care givers | Hemsley et al. (2011), Lewis (2021) and Lacono et al. (2014) | |
| Poor experience of parents | Hemsley et al. (2011) and Lacono et al. (2014) | |
| Theme 3: Nursing curriculum and intellectual disability | Lack of ID content in universities | Cashin, Pracilio, et al. (2022), Foo et al. (2021), Furst and Salvador-Carulla (2019), Lewis et al. (2020), Trollor et al. (2018, 2016) and Wilson, Howie, and Atkins (2019) |
| Attitude of nursing students | McKenna et al. (2012) and Williams et al. (2015) | |
| Clinical placement in ID | Cashin, Buckley, et al. (2022)and Goddard et al. (2010) |
6 Theme 1: Workforce Development and Professional Standards
An Australian national survey reported that the education of nurses working in the disability sector is fragmented; it varies between vocational qualifications and postgraduate education (Lewis et al., 2020; Wilson et al., 2020). Most of the nurses in the sample (n = 33) had an undergraduate (n = 33), postgraduate (n = 31) or hospital-trained qualification (n = 25), and some were with vocational qualification (n = 12). Only half of the nurses in the disability sector had a further acquired specialist qualification in ID-specific contexts. Around 12 people had a mental retardation nursing certificate discontinued in 1985, and a few (n = 7) had a Certificate IV qualification in disability studies (Lewis et al., 2020). This explains the challenges faced by nurses in caring for people with IDs reported in different studies in Australia (Foo et al., 2021; Hemsley et al., 2012; Jaques et al., 2018; Lewis et al., 2019; Taua et al., 2012; Wilson et al., 2018, 2020).
It was reported that nurses face challenges communicating with people with IDs in acute care settings (Lacono et al., 2014). In particular, a communication problem was evident where the capacity for the person (or guardian) to agree with informed consent could have been more apparent, and this was an area where nurses described themselves as unprepared (Lacono et al., 2014). Hence, nurses are cautious about the need to depend on paid or unpaid caregivers for communication when caring for people with IDs (Hemsley et al., 2011; Lewis et al., 2019). The effort to communicate with people with IDs was limited by insufficient time, which forced the nurses to rely on communicating with family or paid caregivers (Hemsley et al., 2011). Paid care providers play an essential role in supporting people with IDs, meeting activities of daily living and communicating and advocating (Hemsley et al., 2011). Nurses encounter difficulties in comprehending the requirements of individuals with IDs and struggle to accommodate their unique conditions. (Lacono et al., 2014). It is further complicated by the poor attitude of nurses towards people with IDs (Lacono et al., 2014). This highlights the need for proper training and educational preparation for nurses working in the disability sector.
A national survey (Cashin, Pracilio, et al., 2022) in Australia has revealed significant deficiencies in the knowledge, preparedness, confidence and comfort of nurses when caring for individuals with IDs (Cashin, Pracilio, et al., 2022). The survey found that the vast majority of nurses lack postgraduate qualifications related to ID, and a significant proportion have not received continuing professional development (CPD) in these areas. This highlights the need for improved knowledge and confidence among registered nurses in addressing the needs of individuals with IDs. Nurses reported the least confidence in specific skills, such as referring caregivers to resources, nonverbal communication and managing escalation behaviours. Additionally, many nurses were unfamiliar with reasonable adjustment plans, the NDIS and their role within NDIS support services. Clinical placements improved nurses' confidence and preparedness, but there remains a clear need for enhanced education and training in this critical healthcare area.
A qualitative study conducted in Australia among staff working in palliative care explored their experience with death and dying with people with IDs and reported that nurses, doctors and occupational therapists found it difficult and stressful to communicate with people with IDs (Foo et al., 2021). Most of the time, there is no direct or no conversation; conversation is purely based on the perceived capacity of the patient to understand the concept of death and dying, communication ability and ability to cope with discussions. They expressed the need for a different approach when communicating and the lack of knowledge and familiarity in caring for people with IDs. It was reported that staff training in ID were more likely to talk to people with IDs about death and dying (Foo et al., 2021). This further strengthens the argument for including ID content and training for nurses in the disability sector.
The literature indicates that individuals with IDs often fear hospital visits due to concerns about nurses' ability to deliver safe and suitable care, insufficient knowledge and skills among hospital staff, negative attitudes and system failures to accommodate their changing needs and over-reliance of staff on family or paid caregivers (Lacono et al., 2014). Parents of young children, especially those less than 1 year of age, require extensive support from nurses. They need assistance adjusting to the ID diagnosis, information on supporting their child's daily needs and development, and connecting to other parents of children with IDs with similar needs (Douglas et al., 2016).
A study by Wilson et al. (2018) found that nurses have varying understanding of professional practice standards for intellectual and developmental disability nursing but recognise their importance. However, these standards are separate from national competency standards (Edmonds et al., 2016). Existing practice standards can inform the development of new standards for disability nurses (Wilson, Lewis, et al., 2019; Wilson, Wiese, et al., 2019). Unfortunately, there is a lack of evidence to guide practice, guidelines and policies for ID nurses (O'Reilly et al., 2018; Wilson, Wiese, et al., 2019), resulting in health disparities for individuals with IDs. This highlights the ongoing demand for nurses with expertise despite policy changes. When caring for children or young people with IDs, no specific policies or procedures are currently in place. Policies are needed to support the use of family centred care in their health care (Mimmo et al., 2022).
Theme 1 highlights that nurses are generally insufficiently prepared for effective communication and care of people with IDs and their families. They lack the skills to meet the complex care needs of people with IDs. The shift towards community-based care for individuals with IDs has highlighted the need for specialised disability nursing. This finding directly relates to the research questions by shedding light on the gaps in nursing education and practice concerning ID care, prompting the call for clear practice standards and policies to enhance healthcare access and quality of life for individuals with IDs.
7 Theme 2: Hospital Experience and Support Needs of Individuals With IDs
Research on the hospital experience of people with IDs in Australia is scarce. Only three studies were identified in this review (Douglas et al., 2016; Lacono et al., 2014; Mimmo et al., 2022). The hospital experience for children were similar to that of adults with IDs in terms of communication barriers. Parents require assistance understanding their child's ID diagnosis, obtaining knowledge and information and connecting with other parents (Douglas et al., 2016). Communication barriers were also identified in the literature, with nurses relying on parents or carers for information and daily care. A 2022 study (Mimmo et al., 2022) on nurses' perceptions of providing good care to children and young people with ID who were hospital inpatients highlighted the importance of forming partnerships, communication and continuity of care to enhance the patient experience. Establishing rapport through play, involving parents, seeking guidance from experienced colleagues, and demonstrating empathy made children feel safe and comfortable during their hospital stay. Time constraints were identified as barriers, with nurses prioritising clinical requirements over the child's needs. The study recommended the inclusion of child life therapists to address the child's needs (Mimmo et al., 2022).
Individuals with IDs from culturally and linguistically diverse (CALD) backgrounds face unique challenges (Lewis, 2021). With a significant percentage of Australia's population (21%) speaking a language other than English, effective service delivery is significantly impacted (Lewis, 2021). Accessing and utilising services becomes complicated due to cultural and social barriers, further exacerbated by Australia's fragmented delivery of services. This situation creates inequities, particularly for people from CALD backgrounds (Lewis, 2021). It has been observed that children with ID from CALD backgrounds are less likely to access therapy services compared with people not from CALD counterparts and require more referrals to access the NDIS. It is clear that the challenges faced by individuals with IDs from CALD backgrounds directly impact their hospital experience and support needs. These issues highlight the critical need for healthcare systems to address cultural competence and inclusivity in service delivery, ensuring that individuals with IDs from CALD backgrounds receive appropriate and equitable support during their hospital stays.
Interestingly, children from CALD backgrounds are more likely to receive diagnoses of gross developmental delay (GDD), intellectual and developmental disorder (IDD) and autism spectrum disorder (ASD) (Lewis, 2021). Delayed access to services and interventions due to delayed referrals is a concern, as early intervention is crucial (Lewis, 2021).
Overall, the literature review provided insights into the challenges faced by individuals with IDs during hospital stays, particularly in communication, partnership-building and addressing cultural and linguistic barriers. These findings contribute to understanding the quality of nursing care and educational preparedness for ID nursing practice in Australia, aligning with the aim and questions of the integrative literature review.
8 Theme 3: Nursing Curriculum and ID
Nurses with appropriate education and expertise are required to care for people with IDs; despite this, nursing curriculums in universities in Australia are not providing adequate educational preparation for nursing students (Edmonds et al., 2016; Furst & Salvador-Carulla, 2019; Lewis et al., 2019; O'Reilly et al., 2018; Trollor et al., 2016; Trollor et al., 2018; Wilson, Lewis, et al., 2019). There is an inconsistent inclusion of content on ID in the training programme for nurses, which is mainly implemented as a part of professional development rather than an educational pathway (Cashin, Buckley, et al., 2022; Furst & Salvador-Carulla, 2019; Trollor et al., 2016).
A survey (Cashin, Buckley, et al., 2022) of 711 registered nurses' educational experiences and self-perceived capability to care for people with IDs and autism reported that 68.5% (n = 475) did not have any education and training in ID/ASD in their undergrad nursing curriculum. In total, 31.5% who received it was a single unit of study (n = 142, 61.5%), and only 17.9% (n = 39) had content embedded in the entire curriculum. Furthermore, 80.8% (n = 560) received no clinical placement opportunities caring for people with intellectual or ASD. Participants registered as a nurse between 1971 and 80 were more likely to receive a clinical placement in intellectual or ASD care when compared to nurses registered between 2011 and 2020 (28.5% vs. 10.5%). Only 55.7% reported they are somewhat knowledgeable, and 60% reported they are confident in caring for people with IDs. They also reported that their nursing education did not prepare them to care for people with IDs. Nurses felt confident discussing disability with other health professionals, developing therapeutic relationships, establishing treatment procedures and communicating; however, they were not confident in the specific health needs of people with IDs (Cashin, Buckley, et al., 2022).
Several studies conducted in Australia (Cashin, Pracilio, et al., 2022; Foo et al., 2021; Furst & Salvador-Carulla, 2019; Lewis et al., 2020; Trollor et al., 2016, 2018; Wilson, Howie, & Atkins, 2019) have established that Australian universities are failing to deliver content to prepare nurses to care for people with ID. Across 15 universities that offer content on ID, lectures (82%) were the primary mode for teaching and learning experiences, followed by tutorials (59%) and workshops (26%) (Trollor et al., 2018). Only one nursing school involved a person with a disability in the unit delivery. A person with IDs participated in the role plays with the students, which helped them to build communication skills. ID content was delivered by only some teachers who specialised in ID in almost 80% of the universities (Trollor et al., 2018). Over half of the universities offered no ID content in the curricula, and those who taught dedicated 3.6 h per unit to ID content. Clinical assessment skills, ethics and legal issues were the most frequently covered sessions, but human rights issues and preventative health could have been better represented (Trollor et al., 2016).
Goddard et al. (2010) conducted a study in Australia among undergraduate students to assess the effectiveness of a functional clinical placement model in a regional community for caring for children with IDs and their families. Five families of children with IDs, nine nursing students and two nursing academics were involved in the study. A family focused health promotion intervention was administered to promote wellness and prevent illness. The study demonstrated increased awareness and valuing of the health needs and increased level of competency of student nurses in caring for people with IDs (Goddard et al., 2010).
In one study, nurses had more positive attitudes towards adults with physical disabilities than IDs (median = 634 vs. 567, Z = −5.473, p = 0.000) (Desroches et al., 2021). However, the two conditions have no difference in positive and negative emotion scores (Desroches et al., 2021). Nurses caring for adults with IDs experience more positive emotions than mainstream nurses (median = 180 vs. 153, U = 941.5, p = 0.013). There are no significant differences in attitudes or negative emotions between ID nurses and mainstream nurses (Desroches et al., 2022).
A study by Williams found that female nurses exhibit more positive attitudes towards people with IDs than male nurses (Williams et al., 2015). Heidke found that recorded interviews of people with IDs have been shown to improve attitudes of nursing students (Heidke et al., 2018), and clinical placements are beneficial for gaining insight and improving attitudes (Doody et al., 2020). A study (McKenna et al., 2012) among undergraduate nursing students found high empathy towards people with IDs, regardless of year of study, age and gender. This level of empathy is similar to student nurse attitudes towards terminal illness, chronic pain and acute mental illness (McKenna et al., 2012).
Finally, Theme 3 sheds light on healthcare professionals' attitudes and emotions concerning IDs. Notably, nurses appear to hold more positive attitudes towards adults with physical disabilities than those with IDs. However, nurses caring for individuals with IDs experience more positive emotions than their mainstream counterparts. Furthermore, the influence of gender on attitudes is evident, with females exhibiting more positive attitudes towards people with ID. Encouragingly, undergraduate students, regardless of their year of study, age or gender, demonstrate high levels of empathy towards individuals with IDs, akin to their attitudes towards other health conditions. This finding underscores the importance of targeted education and training initiatives within nursing curriculum and professional development programmes. By addressing misconceptions, stereotypes and biases, these initiatives can lead to improved attitudes and enhanced care delivery for individuals with IDs. Integrating modules or courses specifically focused on ID within nursing education can foster empathy, understanding and positive attitudes among future healthcare professionals.
In summary, fostering positive attitudes and emotions among healthcare professionals and students towards individuals with IDs is vital for providing inclusive and empathetic care. These insights highlight the importance of education, exposure and ongoing training to create a healthcare environment that values and respects the diverse needs of all patients, including those with IDs.
9 Discussion
Insufficient knowledge and training regarding IDs among nurses have been well-documented in scientific literature. Several studies (Cashin, Buckley, et al., 2022; Furst & Salvador-Carulla, 2019; Goddard et al., 2010; Trollor et al., 2016, 2018; Wilson, Howie, & Atkins, 2019) emphasise the lack of educational content on ID in university curricula in half of the universities. Consequently, the nursing workforce's ability to provide comprehensive care to individuals with IDs has been severely compromised, further exacerbating the growing healthcare demand for this population. The study's research questions, focusing on understanding the nursing care needs of individuals with IDs and assessing nursing education's preparedness in this area, are directly informed by the documented knowledge gap highlighted in the scientific literature. The lack of explicit ID content in university curricula, as evidenced by multiple studies, underscores the urgency of addressing this issue to enhance healthcare professionals' ability to provide safe and effective care to this population.
The life expectancy of people with IDs is increasing, and their health issues are complex with advanced age (O'Reilly et al., 2018; Wilson, Howie, & Atkins, 2019; Wilson, Lewis, et al., 2019). The physical care needs may be similar for people with or without IDs. However, skills in communication, advocacy and person-centred care differ from the general population (Jaques et al., 2018). Ideally, nurses working with people with IDs should develop a clinical skill set focusing on building relationship pro-activeness and reasonable adjustments in communication, which incorporate increased patience and resilience (Jaques et al., 2018; O'Reilly et al., 2018).
The low levels of self-reported knowledge and confidence of nurses working in the public mainstream care environment are significant, as it raises the question of to what degree nurses are meeting their responsibilities as outlined in the UN convention relating to the rights of people with disabilities (United Nations, 2015). Considering that people with ID present more frequently to the ED have more extended stays in acute hospitals and have more readmission rates when compared to the general population, the reported low levels of knowledge suggest that education programmes about ID for this cohort of nurses are an urgent priority. The identified lack of knowledge underscores the urgent need for education programmes focused on ID within this nursing cohort, highlighting the imperative of ensuring safe and effective care for individuals with these conditions.
To address these gaps, Weise et al. (2017) propose implementing a comprehensive national strategy to ensure nondiscriminatory access to health care for individuals with IDs. Nurses play a crucial role in interdisciplinary collaborations facilitating the transition of individuals with IDs between different healthcare settings, such as from paediatric to adult healthcare services or moving from hospital care back to community-based care. Community health centres are particularly suitable settings for nurses, given their scope of practice. Nurses specialising in intellectual and developmental disabilities should have the necessary skills to assess individuals and fulfil the support and training needs of people with IDs and their caregivers. Additionally, nurses should acquire adequate communication skills tailored to the unique requirements of individuals with IDs.
10 Limitation
A publication bias not to include papers about ID may exist in the nursing literature as an artefact of its absence in nursing curriculum and health settings with the advent of the NDIS sector. Because of the dearth of literature about the specialised nursing field for people with IDs originating from Australia, all studies were included. Hence, the quality of the individual studies was not formally assessed. Critical studies might have been published in languages other than English, which would have been missed in our search strategy. A limited number of studies identified the unique roles of ID nurses in Australia.
11 Recommendations
The literature reveals a gap in knowledge regarding the nursing educational preparedness for nurses working with individuals with IDs. Further research is recommended to investigate the quality of health service delivery to this population, especially in light of the introduction of NDIS in Australia. Additionally, research is needed to support leadership and advocacy activities undertaken by nurses for the welfare of individuals with IDs.
There is a clear need for the inclusion of introductory units on ID within undergraduate nursing curricula, alongside the availability of postgraduate courses to facilitate specialisation in ID nursing. The absence of specific registration standards for ID nursing in Australia represents a significant oversight, as it fails to address the unique needs of individuals with IDs. This underscores the urgent requirement for workforce development in this crucial area. Literature highlights the negligible number of studies done in various contexts, such as palliative care, emergency care and primary care. Both undergraduate and specialist postgraduate programmes in ID nursing exhibit notable gaps, particularly concerning mental health literature, where there is a surprising lack of studies addressing the mental health needs of individuals with IDs—a population mental health nurses often engage with.
- Enhancing nursing knowledge, experience and competency in caring for individuals with IDs.
- Improving the experience and confidence of individuals with IDs and their carers or guardians during hospital and community health episodes of care. This aligns with the aim by seeking to enhance the overall quality of care provided to this population, reflecting the review's focus on nursing care quality.
- Better understanding of the current nursing care needs of individuals with IDs and their parents, caregivers and guardians. This emphasise the importance of understanding the existing challenges and requirements in ID nursing practice, which is fundamental to improving care quality and educational preparedness.
- Developing strategies to promote collaborative relationships between carers and individuals with IDs. Acknowledging the significance of effective collaboration and communication in nursing practice, particularly in the context of caring for individuals with IDs, contributes to enhanced educational preparedness and practice quality in this field.
- Inclusion of individuals with IDs in the development of ID content for university teaching
- Establishing a comprehensive database of ID resources for nurses would facilitate their professional development and knowledge update.
The establishment of a recognised specialty in disability nursing and the improvement of nursing education and curricula demand a solid evidence base derived from research. This initiative offers a clear career path for experienced clinicians to provide competent care to individuals with IDs. Practical recommendations include the integration of mandatory disability nursing units into preregistration nursing programmes, ensuring that all nursing graduates in Australia possess a foundational knowledge of disability nursing, and promoting collaboration between nursing schools and the Nursing and Midwifery Board of Australia. To deliver high-quality health care to individuals with IDs, the adoption of a coordinated care model, such as intellectual liaison nurses' care coordination, is crucial. This model necessitates a highly skilled workforce capable of addressing the complex needs of this population.
12 Conclusion
The literature emphasises the necessity of educational preparation for nurses and the inclusion of ID content in nursing curricula. Specialised areas of nursing practice are crucial for equipping nurses to provide quality care to individuals with IDs. The findings of the review recommend reintroducing a disability nursing specialty to cater to the complex requirements of these patients. Furthermore, the review suggests incorporating dedicated study units and clinical placements focusing on IDs in undergraduate nursing curricula.
13 Relevance to Clinical Practice
The findings from a national survey among Australian nurses underscore the relevance of clinical practice in the ID sector (Cashin, Pracilio, et al., 2022). The survey highlighted a significant proportion of older and predominantly female nurses working in this field, indicating an aging workforce with specialised training in ID care (Cashin, Pracilio, et al., 2022). However, this workforce is at risk of decreasing due to various factors such as the absence of a dedicated ID nursing specialty, limited ID content in undergraduate programmes and insufficient clinical placement opportunities in this area. These issues contribute to a reduction in the supply of adequately trained nurses capable of addressing the complex healthcare needs of individuals with IDs. The implications of these findings suggest a critical need for prioritising ID nursing education, fostering interest among nursing students and ensuring comprehensive clinical training to support quality care for this vulnerable population.
The study underscores the pressing need to integrate ID education into nursing curricula at all levels to enhance nurses' readiness for comprehensive care of individuals with IDs. The absence of specific registration standards for ID nursing is a crucial gap that must be addressed to recognise the essential role of these nurses in health care officially. Additionally, addressing care gaps across various healthcare settings, including palliative, emergency and primary care, is vital for clinical improvement and ensuring the delivery of high-quality, person-centred care for individuals with IDs.
The dearth of research on the mental health of individuals with IDs is particularly concerning, as mental health nurses frequently engage with this population. It underscores the need for comprehensive mental health support and specialised training to address the unique challenges faced by these individuals. The under-representation of First Nations people and CALD populations reveal significant deficiencies that demand a more inclusive and culturally sensitive approach to care.
Acknowledgement
Open access publishing facilitated by University of Canberra, as part of the Wiley - University of Canberra agreement via the Council of Australian University Librarians.
Conflicts of Interest
Prof Rhonda Wilson is an Editorial Board Member of the International Journal of Mental Health Nursing.
Open Research
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.