Cool but dangerous: How climate change is increasing the risk of airborne infections
Less obvious but more certain and immediate than future droughts and floods, the escalating use of air conditioning (AC) globally is directly resulting in conditions favoring increased person-to-person transmission of airborne infections such as tuberculosis (TB), influenza (flu), and measles. Unlike the gradual environmental effects of increased CO2 emissions, the impact of AC on airborne infection is nearly instantaneous. This is because for efficient AC use, windows and doors must be closed, immediately eliminating the natural ventilation upon which much of the world depend for diluting and disinfecting room air. Moreover, the most common, highly efficient AC models are ductless or split units, that is, they quietly cool and dehumidify room air but provide no outdoor air exchange.
In 2015, Davis and Gertler predicted the potential impact of escalating AC use on energy consumption over the coming decades in response to global warming and rising incomes.1 They used Mexico as an example, but the impact will be greater in more populous and hotter countries, like India and China, where the largest number of TB cases reside (Table 1).
| Country (from highest to lowest potential for AC usage) | Population (millions) | Annual CDDs (cooling degree days) | Annual GDP per capita (thousands) | Tuberculosis incidence (per 100 000 population, 2017) |
|---|---|---|---|---|
| India | 1252 | 3120 | 1.5 | 204 |
| China | 1357 | 1046 | 6.8 | 63 |
| Indonesia | 250 | 3545 | 3.5 | 319 |
| Nigeria | 174 | 3111 | 3.0 | 219 |
| Pakistan | 182 | 2810 | 1.3 | 267 |
| Bangladesh | 157 | 2820 | 1.0 | 221 |
| Brazil | 200 | 2015 | 11.2 | 44 |
| Philippines | 98 | 3508 | 2.8 | 554 |
| United States | 316 | 882 | 53 | 3.1 |
| Vietnam | 90 | 3016 | 1.9 | 129 |
| Thailand | 67 | 3567 | 5.8 | 156 |
| Mexico | 122 | 1560 | 10.3 | 22 |
Note
- Except for the US and Mexico, all countries on the list are WHO high TB burden countries (TB incident rates in bold type), and all countries are vulnerable to annual and pandemic influenza outbreaks.
Tuberculosis is the greatest single infectious cause of adult deaths globally, and India has the highest tuberculosis burden in the world (Table 1).2 In addition to annual influenza epidemics, another H1N1 influenza pandemic is predicted, most likely beginning in Asia. Influenza is spread by direct contact with respiratory droplets, but it spreads most efficiently by the airborne route. Measles, the most infectious of airborne viruses, is controllable by immunization, but where herd immunity is lacking, indoor transmission is facilitated in unventilated, air-conditioned indoor environments.
The Davis and Gertler article focused on residential cooling, but the impact of AC on TB transmission will be arguably greater in congregate settings such as hospitals, clinics, prisons, schools, and shelters. Extreme temperatures, high humidity, and air pollution are poorly tolerated, especially by the young, the elderly, pregnant women, and those with pre-existing illnesses, all of whom are also at higher risk for airborne infections. With temperatures in Indian megacities now regularly exceeding 40°C, ductless AC is increasingly common in crowded clinic waiting rooms. Fully air-conditioned hospitals are being marketed in India to reduce heat and air pollution risks. Accustomed to AC at home, medical personnel are also demanding more tolerable work environments. Occupants are cool and comfortable, but a much higher fraction of inhaled air is rebreathed, that is, air recently exhaled by other occupants, with a proportionately higher risk of airborne infection, given an infectious source in the room.3
Although an epidemiological impact of increasing AC use and closed windows on TB transmission at the population level may be measurable over time, it will be a large, long, and expensive study because TB risk factors are many and the association of building occupancy with specific instances of transmission is difficult to document. However, the quantitative relationship between decreased non-recirculated ventilation and increased risk of airborne infection has long been understood.4 Ambient CO2 level monitoring is routinely used to estimate exposure to rebreathed air, a surrogate marker for airborne infection risk.
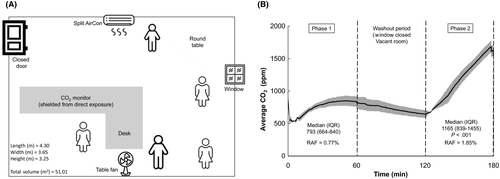
In a university administrative office with a single operative window and a ductless AC unit in Cape Town, South Africa (Figure 1A), five colleagues participated in a simple demonstration of the immediate effects on ambient CO2 levels of closing an open window and turning on a ductless AC unit. (Figure 1A,B). Ambient CO2 was monitored in the center of the room with the window open and the AC off.3 Air was mixed by a table fan. With the window open and AC off, CO2 levels in the occupied room (Phase 1, Figure 1B) appeared to plateau just under 800 ppm, well above average outdoor CO2 levels in the area, but normal in offices and public indoor settings. The room was vacated, and CO2 allowed to return to approximately baseline unoccupied room levels (about 600 ppm) for the next hour (washout period). Finally, with the window closed, and the AC turned on, the same 5 occupants returned to the room for another hour (Phase 2, Figure 1B). The entire procedure was repeated 3 times, and the average CO2 levels are shown in Figure 1B. CO2 levels rose steeply with no sign of plateauing at study end. CO2 levels were on a trajectory to plateau considerably higher levels had the experiment continued several more hours. The average peak level was about 1600 ppm—roughly twice ambient levels with the window open. Restated, within an hour of closing the window, with other parameters unchanged, the estimated fraction of air rebreathed doubled and with it, the risk of airborne infection in the presence of an infectious source. In theory, reducing ventilation by half, doubles the risk of airborne infection.4 A further reduction by half, to 25% of the original ventilation, doubles risk again to four-times baseline. Closing windows generally reduces natural ventilation by more than 75%—to that produced by infiltration around closed windows and doors.
Although climate change is creating new transmission opportunities for airborne infections in warm climates, similar conditions have long existed in cold climates like Russia, former Soviet Union countries, and Central Asia. In Siberia, for example, the risk of MDR-TB was more than sixfold greater for adherent drug susceptible TB patients treated in hospital for any duration compared to those treated entirely on an ambulatory basis.5 Re-infection of drug susceptible TB patients in crowded, unventilated wards by other patients with unsuspected MDR-TB on ineffective treatment is the explanation. Hyper-transmission conditions in cold climates together with delayed diagnosis have led to rates of primary (ie, transmitted) MDR-TB among previously untreated persons ranging from 22% to 38% whereas it rarely exceeds 5%-6% in the rest of the world.6
There are no easy solutions to this complex healthcare delivery problem due to the intersecting considerations of climate, comfort, safety, and cost. Judicious use of air conditioning is warranted, balancing the obvious risks and discomfort of excessive heat against the occult risks of reduced ventilation. However, currently available air disinfection technology can mitigate the transmission of airborne infections if properly applied. We suggest that wherever ductless air conditioning is used in high-risk settings such as healthcare facilities, supplemental room air disinfection should also be installed. Currently, besides natural and mechanical ventilation, there are only two practical technologies to disinfect room air: (a) upper room germicidal ultraviolet (GUV) fixtures and (b) portable room air cleaners. Portable room cleaners filter (and sometimes ultraviolet irradiate) air within an enclosure and circulate disinfected air in the room. A variety of such air cleaning devices is aggressively marketed to hospitals and in a small room might reduce discomfort from some indoor particulate air contaminants, such as pollen, but they commonly deliver too few equivalent room air changes per hour to effectively protect occupants against airborne infection.4
Upper room GUV uses the open space above the heads of occupants to rapidly disinfect large volumes of air, which then mixes with air in the lower, occupied room by low-velocity ceiling fans (Figure 2).7 This simple and safe technology has long been available, but remains underused. With well-designed and installed systems, room occupants are not exposed to dangerous levels of UV. Properly designed, installed, commissioned, and maintained, GUV systems can safely produce the equivalent of 10 to 20 or more effective air changes per hour, both economically and sustainably. Practical, evidence-based dosing and maintenance guidelines have been published.7 Over the years, upper room GUV has been shown to reduce airborne transmission of measles, influenza, and TB in congregate settings.7-9 Effective and safe GUV fixtures, with germicidal output fully characterized, are being marketed in high-burden countries. Local expertise in planning, installing, and maintaining safe and effective GUV air mixing systems is growing. Ideally, AC manufacturers could also market and maintain upper room GUV units designed specifically to be installed above or below wall AC/air mixing units to render air-conditioned rooms much less conducive for airborne infection.

Other, administrative approaches can reduce the risk of airborne infection in buildings. Unsuspected, infectious TB cases can be quickly identified by active case finding and rendered quickly non-infectious by prompt, effective treatment.10 Ambulatory, community-based treatment for TB, even drug-resistant TB, can reduce hospitalization. Influenza and measles vaccination programs can be implemented or improved. New construction and renovations can avoid interior central corridors that often become poorly ventilated waiting areas, heat-collecting glass walls can be avoided to reduce AC needs, and buildings can be constructed with shaded, outdoor waiting areas (climate permitting) designed for natural ventilation.
Climate change represents clear threats to global health from many perspectives. Increasing energy consumption due to AC usage and resulting air pollution in warm countries is a recognized challenge. Less obvious in cool and comfortable congregate settings is the silent danger of increased airborne infection—TB, including drug-resistant strains; influenza, both annual and pandemic, and measles where herd immunity is low. The reality of climate change will increasingly require greater attention to the cooling and dehumidification of indoor air, green building design, solar and wind power, and cost-effective, sustainable air disinfection technology, such as upper room GUV. Greater investment in health systems requires attention to the built environment and the impact of climate change.




