Pseudo-macrocytosis in chronic lymphocytic leukaemia
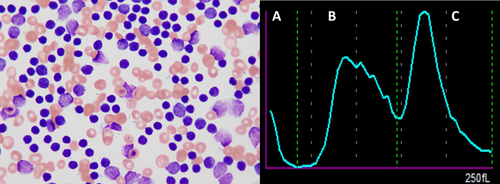
A 49 years old man, without regular medical follow-up, presented with fatigue, over the last 3 months, and new onset dyspnoea. On physical examination numerous lymphadenopathies, massive splenomegaly and hepatomegaly were noted. The laboratory work-up realized on the Sysmex XN 9000®, showed extreme leucocytosis (820 x 109/L) which appeared morphologically as small, mature lymphocytes interspersed with smudges cells (Gumprecht shadows) (Figure 1 left). Immunophenotyping on peripheral blood and bone marrow showed a restriction of lambda immunoglobulin light chain (low intensity), as well as the coexpression of CD5 with CD19, CD20 (low intensity), CD22, CD23, CD38 (partial expression), CD43 and CD200, thus confirming the diagnosis of chronic lymphocytic leukaemia (CLL).
In addition, the patient exhibited severe hyporegenerative hypochromic anaemia (haemoglobin 3.0 g/dL, MCHC 123 g/L), and marked macrocytosis (mean corpuscular volume, MCV, 139 fL, norm: 81–99); not accounted for by reticulocytosis (reticulocytes 30 G/L), B12/B9 vitamin deficiency (B12 236 pm/L, B9 > 45 nmol/L assessed on day 5 of hospitalisation), hypothyroidism, medication or alcohol intake. Unexplained, extreme, macrocytosis with hyporegenerative anaemia usually indicates the presence of an underlying myelodysplastic syndrome (MDS), but the simultaneous occurrence of both neoplasms of distinct cell origin (lymphoid and myeloid) was highly unlikely.
Hyperleukocytosis may hamper haematological count1 or interfere with biochemistry analysis2 (secondary to in vitro hemolysis). Most hematology analyser rely mainly on impedance to count and characterize red blood cells, identified by volumes cut-offs. The three logarithmic difference between leucocyte and erythrocyte counts usually allows for accurate results even if a few lymphocytes are included in the RBC analysis.3 In that case, the red blood cell (RBC) scattergram showed two distinct merging peaks (Figure 1 right, B and C) with the lymphocyte population (Figure 1 right, C) being counted within the RBCs. Therefore, the initial aberrantly high MCV value represents the mean between RBC and the slightly larger lymphocytes volumes, not a true macrocytosis. This pitfall was resolved using a manual haematocrit and leucocrit assessment in combination with the optical (cytometric) measurements to obtain reliable values, free of the influence of the lymphocytosis. The corrected results still showed a profound anaemia with a haemoglobin of 35 g/dL, which was however normocytic (MCV 99 fL) and normochromic (MCHC 350 g/L). The profound anaemia was explained by the massive bone marrow infiltration by the clonal leukemic B-cells.
CLL is a common diagnosis in the haematological department, and sometimes presents with extreme leucocytosis and pseudo-macrocytosis. Obtaining accurate CBC parameters is not anecdotal as it is essential to (i) correctly stage the lymphoid neoplasms and provide associated prognosis information, (ii) eliminate alternative diagnosis and unnecessary diagnostic procedures, and (iii) adequately guide life supportive treatment such as transfusions. This piece advocates for collaboration with lab experts and wise use of the redundant measurement techniques provided by modern automates as well as manual technique to circumvent such issues.
AUTHOR CONTRIBUTIONS
MC, and MG collected the data, analysed the data and co-wrote the manuscript; CC and AC were involved in management decisions and provided critical input to the manuscript. All the authors revised and approved the manuscript.
FUNDING STATEMENT
We have no founding source to declare.
CONFLICT OF INTEREST STATEMENT
All authors declare that they have no conflict of interest.
PATIENT CONSENT STATEMENT
We obtained a signed consent form from the patient.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.




