Contribution of the new XN-1000 parameters NEUT-RI and NEUT-WY for managing patients with immature granulocytes
Sir, Haemogram is the most commonly prescribed examination by clinicians to laboratories in France for both diagnostic purposes and patient follow-up. Haematology disorder suspicions in particular are often based on an initial cell blood count and differential. New automated haematology analysers let one quantify immature granulocytes (IG) in number (IG#) or in percentage (IG%). Occurrence of IG in peripheral blood is a frequent criterion for slide review and could appear not only in case of haematological malignant disease [myeloproliferative syndrome, myelodysplastic syndrome (MDS) or chronic myelomonocytic leukaemia] but also in infectious (septic) or noninfectious reactive (inflammatory) conditions. In most of cases, IG and IG% in blood have an infectious origin without any cytological contribution to an improvement in results but contribute significantly to an increase in manual review rates in daily practice. In Caen University hospital, about 10% of samples show an IG count above 2% and 3% of samples are over 5%. A persistently increased IG count (>10%) in the case of infection is considered as a grave criteria for sepsis 1. When IG appear or disappear, they provide real-time information but no indication of the evaluation of the patient's status. It would be interesting to offer the possibility of relating the occurrence of IG to infectious or noninfectious conditions and ‘anticipating IG% variation’ to efficiently supply the clinician with information regarding the patient's outcome.
The aim of our study was to investigate the potential contribution of research parameters provided by XN-1000 (Sysmex Corporation™, Hyogo, Japan), Neutrophil Granularity Intensity (NEUT-GI), Neutrophil Reactive Intensity (NEUT-RI) and width on y-axis (NEUT-WY) in enhancing the laboratory process for both management of IG count and clinical contribution.
Neutrophil Granularity Intensity, expressed in side scatter intensity, is derived from the NEUT-X parameter already used by the Sysmex XE series analysers. Neutrophil Granularity Intensity is the mean value of high angle diffraction and represents the complexity of the neutrophils (nucleus lobularity, granulations) and has proven to be related to dysplasia of neutrophils on XE-2100 2, 3 and to be independent of the IG% value. Combined with other parameters, it is useful for detecting MDS syndromes or chronic myelomonocytic leukaemia (CMML) at diagnosis and is an effective contribution to both laboratory clinical contribution and workflow improvement. Neutrophil Reactive Intensity, expressed in fluorescence intensity, is representative of the mean fluorescence of the neutrophils and can therefore be related to the activation or immaturity of the population. It is derived from NEUT-Y on XE instruments and few data are available relating the value of this parameter to infection disease/sepsis management 4, 5. NEUT-WY represents the width of the neutrophil scattergram in the WDF channel on the fluorescence axis. This parameter is calculated according to distribution width as it represents the range of the distribution in fluorescence of the major population, excluding outliers below 20% peak height in the distribution curve. It is then representative of heterogeneous fluorescence signal in this population related to either band cells or activated neutrophils.
First, we studied a large group of patients to determine the normal ranges of these new structural parameters. Then, we analysed the potential contribution of these parameters on interpreting IG count in blood samples collected from patients without any haematological disease. All blood samples were collected in K2-EDTA tubes and analysed routinely on properly controlled XN-1000 analysers. The IG compartment measured by the XN-1000 analyser included promyelocytes, myelocytes and metamyelocytes.
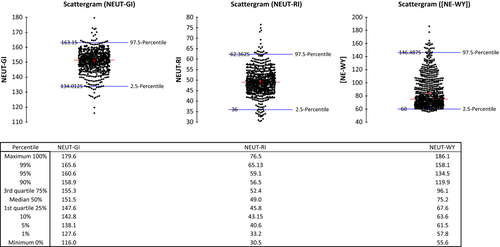
To define the normal ranges of structural parameters, we analysed 3082 strictly normal samples in terms of the quantitative values documented by the ‘Groupe Francophone d'Hématologie Cellulaire’ (GFHC) 6 and without any qualitative flag issued by the analyser. The mean values obtained for NEUT-GI, NEUT-RI and NEUT-WY were 151.045 ± 4.13 (1 SD), 45.43 ± 2.796 (1 SD) and 61.1 ± 3.31 (1 SD), respectively. None showed any significant correlation with either IG% (respective R2 at 0.035, 0.02 and 0.192 for NEUT-GI, NEUT-RI and NEUT-WY) or IG# (respective R2 at 0.015, 0.015 and 0.027 for NEUT-GI, NEUT-RI and NEUT-WY). When both NEUT-RI and NEUT-GI showed homogenous and symmetric distribution, NEUT-WY appeared to be far more heterogeneous (Figure 1).
To analyse the potential predictive value of NEUT-RI/NEUT-WY on IG count variation and so provide useful predictive information for management of noninfectious/reactive or infectious/sepsis situations, a follow-up study was carried out for 222 selected patients (3368 analysed samples). Selection criteria included the following: no surgery between results and at least four available results, one of them showing an IG count >5%. A total of 120 male (54%) and 102 female (46%), with a median age of 62.1 years (0–98.8), hospitalized in different care units (127 from medical units, 56 from surgical units and 39 from intensive care units) were analysed. Patients with haematological diseases were excluded. The structural parameters of neutrophils were studied in relation to IG% variation during the follow-up period for each patient. In a second step, two categories were identified in this group: 172 patients with positive blood culture were classified as ‘infectious/sepsis’; all 50 others (culture negative or not required) were grouped in a ‘noninfectious/reactive’ category. To evaluate the relationship between IG% and structural parameters for neutrophils, we used a linear mixed-effect regression model with random patient effect. This analysis lets one take into account repeated measurements within the same patient. All parameters with P < 0.05 at univariate analysis were included in a multivariate model with selection. Interaction was tested between the structural parameters and the infectious situation and a subgroup analysis was performed with a Bonferroni correction if the interaction was significant. All tests were two-sided at a 0.05 significance level. Analyses were carried out using r statistical software version 2.15.2 (R Foundation for Statistical Computing, Vienna, Austria, http://www.r-project.org). Statistical analysis showed a strong relationship between changes in structural parameters of neutrophils prior to IG variation in a 72-h frame time, which was defined as the best timing for interpretation. We demonstrate an increase in NEUT-RI and NEUT-WY, as well as a decrease in forward scatter light signal (NEUT-FSC), which is representative of the mean size of neutrophils prior to IG% increase and conversely for decrease (Table 1). Based on this observation, we created a mathematic model to predict IG% for patients over 3 days: IG (%) = 7.77 + (0.2418 × NEUT-RI) + (0.0052 × NEUT-WY)−(0.2238 × NEUT-FSC). Regarding 222 patients analysed, our model was efficient and accurate for 203 of them, with only 19 outliers – more than 90% accurate IG prediction in a 3-day time frame. Patients were selected using particular criteria such that this formula is not applicable in a general cohort, but it proves the earlier changes in neutrophil structure in relation to IG%. NEUT-RI in particular appeared to be generally the most informative and very simple to use, that is ‘10 points increase of NEUT-RI leads to 2.4 IG% increase 3 days later’. There was significant interaction between NEUT-RI and infectious situation (P < 0.05), so when one goes into detail of patients with confirmed infectious/sepsis situation in terms of assumed noninfectious/reactive cases, values differed because the contribution on NEUT-WY was two times more influential in the prognosis of IG in infected patients when NEUT-RI was conversely 2.5 times more influential in noninfectious cases, suggesting that both situations follow a different mechanism (Table 1).
| Parameter | Coefficient (IC 95%) | P-value | |
|---|---|---|---|
| All patients n = 222 | NEUT-RI | 0.2418 (0.2143; 0.2694) | <0.0001 |
| NEUT-WY | 0.0052 (0.0042; 0.0061) | <0.0001 | |
| NEUT-FSC | −0.2238 (−0.2520; −0.1956) | <0.0001 | |
| Noninfectious/Reactive patients n = 50 | NEUT-RI | 0.4856 (0.4089; 0.5623) | <0.0001 |
| NEUT-WY | 0.0026 (0.0002; 0.0050) | 0.04 | |
| NEUT-FSC | −0.2079 (−0.2547; −0.1610) | <0.0001 | |
| Infectious/Septic patients n = 172 | NEUT-RI | 0.1992 (0.1665; 0.2319) | <0.0001 |
| NEUT-WY | 0.0055 (0.0044; 0.0067) | <0.0001 | |
| NEUT-FSC | −0.2321 (−0.2753; −0.1889) | <0.0001 |
As new analysers offer an increasing amount of information and parameters, it is mandatory to evaluate them in terms of their clinical benefit. We are introducing NEUT-RI and NEUT-WY values as useful criteria for interpreting IG count and predicting its variation in a 3-day time frame. Once the patient is known, a follow-up for changes in the patient's neutrophil activation parameters would be more informative than just the IG count. In the context of infection, it is of greater interest to judge the variation in these parameters than checking the IG count. Predicting the IG for a patient within a 3-day period would be of great support to clinicians. When IG occurrence is not due to a malignant haematological disease and such hypothesis is clearly rejected, it can be related either to a noninfectious/reactive situation or to an infection/sepsis. Distinguishing between both is an essential clinical matter. NEUT-WY was a good marker for infection suspicion and hence useful to distinguish between a noninfectious or infectious situation, which is an essential clinical matter because in first case, a watch and wait attitude could be recommended, when in the second case, an antibiotic treatment is mandatory and even urgent depending on the evolution of the IG count. NEUT-RI was useful for analysing both noninfectious and infectious situations, especially in the context of infection because it was predictive of the variation of IG% in a 3-day time frame.
Our results lead us to consider the decision of reviewing slides for IG and/or IG% control, especially when considering the impact of such reviews on laboratory processes and the delay in reporting results. In combination with criteria related to NEUT-GI for dysplasia in MDS and CMML that are already defined, as well as other parameters such as monocytes or platelets (CMML), basophils (CML) or haemoglobin (MDS), NEUT-RI and NEUT-WY, would contribute to improving the interpretation of IG, enhancing the laboratory workflow and providing added-value for the clinician.
Acknowledgements
We would like to thank the technical staff of the laboratory for supporting additional tasks during the study, Gemma Figueras and Jean-Pierre Pérol for precious discussions in interpreting the results, and Mark C. Gray for editorial support (Sysmex Europe).