Craniocervical flexion test in patients with migraine: Discriminative validity and accuracy
Funding information
First and fourth authors received a grant to develop this research respectively from Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP/process 2018/21687-8) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brazil (CAPES/Finance Code 001). The sponsor had no role in the design of the study, conduct, analysis, interpretation of data and reporting and decision to publish.
Abstract
Objectives
To evaluate the discriminative validity and provide a clinical cut-off of the craniocervical flexion test (CCFT) in migraineurs stratified by the report of neck pain, headache-related disability and neck disability.
Methods
Fifty women without headache and 102 women with migraine were recruited by convenience from a local tertiary care setting. Migraine diagnosis followed the International Classification of Headache Disorders. All volunteers underwent the CCFT. Patients with migraine answered the Migraine Disability Assessment (MIDAS) and Neck Disability Index (NDI) questionnaires. Discriminative validity was verified by group comparison, and the clinical cut-off was obtained and classified according to the diagnostic accuracy of the CCFT.
Results
The CCFT presented discriminative validity for comparing control (median = 28, IQR = 6) with migraine (median = 26, IQR = 4, P = .01) and migraine with neck pain (median = 26, IQR = 4, P = .01), but not among the migraine subtypes with disability by migraine or neck pain-related disability on the MIDAS and NDI. The diagnostic accuracies were classified between poor and not discriminating with the area under the receiver operating characteristic curve ranging from 57% to 69% and non-acceptable values of sensitivity, specificity and positive and negative likelihood ratios.
Conclusion
The CCFT can discriminate asymptomatic controls from migraine patients with and without neck pain. However, it cannot discriminate patients with migraine according to their pain-related disability. Also, the CCFT does not offer an optimal cut-off value in migraine patients adequate to clinical practice.
What’s known
- The craniocervical flexion test evaluates the motor control of cervical flexor muscles and is used as a specific exercise for physical rehabilitation.
- It has been widely used and strongly recommended for assessing cervical dysfunction in patients with migraine, but it has not been validated for this population.
What’s new
- This study confirms the validity of the craniocervical flexion test in patients with migraine but does not present optimal cut-off value in migraine patients adequate to clinical practice.
- Although it is indicated to assess cervical dysfunction, the test was not proven to help determine the degree of migraine and neck pain-related disability.
1 INTRODUCTION
Migraine is a primary and chronic neurological condition that affects more than 10% of the world population1 and is commonly associated with pain and musculoskeletal disorders related to the craniocervical region.2 These disorders can trigger migraine, increase the frequency of attacks3 and contribute to migraine disability.4 Also, they are associated with delaying or impeding the therapeutic effects of abortive drugs and other prophylactic interventions.5, 6 Thus, evaluation of the craniocervical region is essential to offer an effective treatment for migraine2 and must be performed with reliable and valid instruments to avoid inaccurate or biased results.7, 8 Evaluation should also include instruments with diagnostic accuracy to discriminate between different conditions.9
The craniocervical flexion test (CCFT) is a low-load test that evaluates the performance of the deep cervical flexor muscles (longus capitis and colli) that contribute to the active spinal segmental stabilisation in support of the cervical lordosis and motion segments.10 The CCFT presents positive reliability and convergent validity to assess the function of the deep cervical flexor muscles in several populations,11 including asymptomatic individuals12 and those with neck pain.13 Although the CCFT is reliable and valid; a recent systematic review suggested that future studies should be conducted with high methodological quality to more accurately assess measurement error, discriminative validity and responsiveness.11
The CCFT has been widely used and strongly recommended for assessing cervical dysfunction in patients with migraine.14, 15 In fact, neck pain in patients with migraine worsened muscle performance of cervical musculature as evaluated by the CCFT.16 The discriminative validity of the CCFT for migraine is still unknown, and further investigation will contribute to a better understanding of this clinical test's role in migraine evaluation. The clinical diagnosis of migraine is well-established by the International Headache Society (IHS)17; the CCFT could assist physical therapists in the kinetic diagnosis to identify musculoskeletal neck dysfunction and help guide clinical decisions.
Moreover, it would be helpful to obtain a cut-off point for identifying the deficit in the function of deep flexors in migraine because there are currently no parameters for this in clinical practice. Therefore, the objectives of this study are (1) to evaluate the discriminative validity of the CCFT between control and migraine individuals, in addition to considering the stratifications of the migraine group associated with neck pain, migraine-related disability, and cervical spine-related disability and (2) to identify a cut-off for a deficit of function of the deep flexors capable of distinguishing the migraine patient from the control and the migraine stratifications defined by neck pain, migraine and neck disability.
2 METHOD
2.1 Study design
The analysis of the discriminative validity of the CCFT can be classified as a cross-sectional study. However, according to the Statement for Reporting Studies of Diagnostic Accuracy18 (STARD), this could be considered as a prospective observational study, as the data collection was planned before the index test and reference standard were performed. The protocol was designed following (STARD)18 and The Consensus-based Standards for the Selection of Health Measurement Instruments (COSMIN) guidelines.7
2.2 Ethical aspects
The Ethics Committee in Research from Ribeirão Preto Medical School approved this study (process N. 1100/2017), which complies with the Declaration of Helsinki. All participants gave written informed consent before data collection began.
2.3 Participants, therapists, centres
The study included patients already diagnosed with migraine (target condition) and participants in whom the condition was excluded. Women with migraine were recruited by convenience sampling at a local tertiary care setting between March 2019 and February 2020. The inclusion criteria for women with migraine were: age between 18 and 55 years and a clinical diagnosis of migraine, with the absence of other types of associated headache, according to the International Classification of Headache Diseases.17 Two neurologists diagnosed migraine from the outpatient clinic who were specialists in headache care and not involved in the study. The study researchers screened asymptomatic controls in the same period among the local population. Participants in the asymptomatic control group were 18-55 years old, had no history of cervical pain and were headache-free. The exclusion criteria applied to both groups were systemic and neurological diseases, injury to the face and/or neck, pregnancy and lactation.
2.4 Measures
All eligible individuals responded to an assessment form with information on age and body mass index (BMI), conducted by a physiotherapist from a local tertiary care setting. The physiotherapist assessed migraine patients for the characteristics of the migraine (time of illness, frequency of crises and intensity of pain based on the Numeric Pain Rating Scale (NPRS, 0-10 points) and their responses to the Migraine Disability Assessment (MIDAS) and the Neck Disability Index (NDI). Patients with migraine were asked about the presence of neck pain and, if it was present, they provided information on the time, frequency and intensity of this pain (NPRS). Following the assessment, the CCFT was performed by all individuals and supervised by another physiotherapist previously trained and qualified to use the measure. The physiotherapist did not participate in the other evaluation procedures and was blinded to the subjects' condition.
MIDAS is a five-item questionnaire that assesses migraine-related disability in participating in activities at work, school and the home environment.19 For each question, the subject responds according to the number of days in which activities were affected in the last 3 months. The final score ranges from 0 to 90 points, and individuals can be classified as without disability (0-5 points) or with mild (6-10 points), moderate (11-20 points) and severe disability (21 or more points).
The NDI consists of 10 questions about neck pain's influence on daily tasks, such as personal care, sleep and reading.20 The questions are composed of six alternatives that range from zero to five points each. The final score ranges from 0 to 50 points, and individuals can be classified as without disability (0-4 points) or with mild (5-14 points), moderate (15-24 points), severe (25-35 points) or total disability (36 or more points).
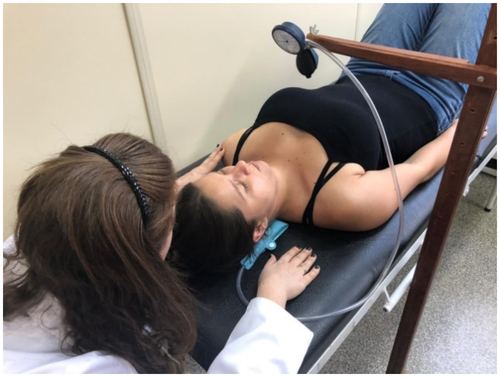
The CCFT assesses the activation and isometric endurance of the deep cervical flexors and their interaction with the superficial cervical flexors in a low-load task using biofeedback.10 It can be described as a test of neuromotor control created to reflect, with more specificity, the deep flexors' function in active movements and postures for the clinical assessment.10 To perform the CCFT, the subject remained supine with lower limbs relaxed on a stretcher. A biofeedback pressure unit (Stabilizer Pressure Biofeedback®; Chatanooga, Hixson, TN, USA) was positioned behind the neck, close to the occipital region, and used to effectively monitor the tendency to rectify cervical lordosis due to the contraction of deep flexors. The unit was inflated to a basal pressure of 20 mmHg, and the subjects were instructed to perform craniocervical flexion, characterised by a slight nodding movement, during five progressive stages of increasing craniocervical flexion range of motion (reflected by the pressures 22, 24, 26, 28 and 30 mmHg at the biofeedback pressure unit). The task consisted of maintaining an isometric contraction for 10 seconds at each stage until reaching 30 mmHg. The rest interval between the stages was 30 seconds.10 Evaluators observed whether the subject made compensations, such as head retraction or elevation, mouth opening or simultaneous contraction of the sternocleidomastoid and anterior scalene muscles (verified by the evaluator's manual palpation).10 Evaluators familiarised the subject with the test before conducting it. Individual's CCFT score was determined by the last stage (mmHg) that the participant could sustain without making compensations (Figure 1). Although different ways of performing the test are reported, the principles described here followed the same protocol used in most studies.10, 16, 21, 22
2.5 Data analysis
All analyses were performed between the control and migraine groups, control and migraine-with-neck-pain groups and, to verify potential differences between the migraine groups, through the following comparisons: (1) according to the MIDAS score, between groups without disability (0-10 points) and with disability (>11 points) and (2) according to the NDI score, between groups without disability (0-4 points) and with disability (>5 points). The group with disabilities, according to the MIDAS, included only moderate and severe levels to distinguish them from subjects with significant disabilities, in addition to allowing a balance in the sample size because migraine is a highly disabling condition.17
Data regarding age, BMI and migraine characteristics related to the duration of the disease, frequency of crises and intensity of pain were compared through Mann–Whitney's U test, given the non-normal distribution of data residues. The characteristics of neck pain were described as a median (interquartile range) or as a percentage.
Between-groups discriminative validity compared the median values of the CCFT between groups by the Mann–Whitney's U test because it is an ordinal variable. The effect size (ES) was calculated by dividing the Z score by the square root of the total number of the sample and interpreted as a large effect (0.5), a medium effect (0.3) or a small effect (0.1).23
The diagnostic accuracy of the CCFT to differentiate controls from migraine and migraine with neck pain and differentiate subtypes of migraine was assessed using different measures. These measures were the area under the receiver's operational characteristic curve (AUC), sensitivity (SN), specificity (SP), positive likelihood ratios (LR+), negative likelihood ratio (LR−), positive predictive value (PPV) and negative predictive value (NPV).
The AUC is a global measure of diagnostic accuracy and was interpreted as follows: 0.9-1, excellent; 0.8-0.9, good; 0.7-0.8, fair; 0.6-0.7, poor; and 0.5-0.6, not discriminating.24 The analyses of the receiver operating characteristic (ROC) curve also provided the optimal cut-off score for the CCFT, that is, the score with the best overall accuracy in identifying subjects according to compared groups considering the best SN and SP.24 SN considered the percentage of people with a positive test for a given condition. SP considered how many people had a negative test among people who do not have the condition. PPV and NPV are the proportions of individuals with positive and negative test results, respectively, who are correctly diagnosed.9 LR+represented the ratio between the probability of a positive result occurring in individuals with the disease and those who do not have the disease. LR− represented the ratio between the probability of a negative result occurring in individuals with the disease, as compared to those who do not have the disease. Good diagnostic tests show LR+ > 10 and LR− < 0.1.25 The values of SN, SP, PPV, NPV, LR+and LR−were analysed using cross-tabulation. The frequencies used are given as supplementary material. All of them were reported with their respective 95% confidence intervals. A significance level of 0.05 was established, and all statistical analyses were completed using SPSS software, version 20 (SPSS Inc, Chicago, IL, USA). Analyses of variability in diagnostic accuracy were not performed.
The sample size was stipulated as the largest possible number of individuals selected through convenience sampling during the collection period. According to COSMIN recommendations for discriminative validity, we needed a minimum sample size of 50 individuals in each group to achieve adequate methodological quality.7
3 RESULTS
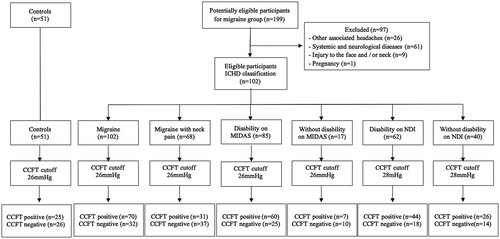
A total of 199 individuals with potential eligibility were recruited, but 97 were excluded, resulting in a final sample of 102 patients with migraine and 51 controls (Figure 2). There was a significant difference in the mean age of the control group and the migraine (P = .02) and migraine-with-neck-pain groups (P = .03). Migraine patients presented high intensity of headaches, and those with disabilities, according to the MIDAS, had a higher frequency (P = .002) and intensity of headaches (P = .02) compared to migraine patients without disabilities (Table 1).
| Characteristic | Control (n = 51) | Migraine (n = 102) | Migraine with neck pain (n = 68) | Migraine | |||
|---|---|---|---|---|---|---|---|
| Without disability on MIDAS (n = 17) | With disability on MIDAS (n = 85) | Without disability on NDI (n = 40) | With disability on NDI (n = 62) | ||||
| Age (y) | 27.9 (6.0) | 31.0 (12.0) | 30.5 (11.0) | 31.0 (12) | 31.0(13) | 31.5 (14.0) | 31.0 (11.0) |
| BMI (kg/cm2) | 22.7 (6.0) | 23.7 (6.4) | 23.9 (7.1) | 23.6 (6.6) | 23.8 (6.8) | 22.8 (6.7) | 24.0 (7.3) |
| Headache years | — | 15.5 (12.0) | 15.0 (11.0) | 15.0(10.5) | 16.0 (13.0) | 16.5 (18.0) | 15.0 (11.0) |
| Days/month headache | — | 8.0 (11.0) | 8.0 (11.0) | 4.0 (4.5) | 8.0 (11.0) | 6.5 (8.0) | 8.0 (11.0) |
| Headache intensity | — | 8.0 (3.0) | 8.0 (3.0) | 7.0 (2.5) | 8.0 (2.5) | 8.0 (2.7) | 8.0 (3.0) |
| Neck pain years (%) | |||||||
| Less than 2 y | — | — | 29.4 | — | — | — | — |
| More than 2 y | — | — | 70.6 | — | — | — | — |
| Days/month neck pain (%) | |||||||
| Less than 15 d | — | — | 55.9 | — | — | — | — |
| More than 15 d | — | — | 49.1 | — | — | — | — |
| Neck pain intensity | — | — | 5.7 (2.1) | — | — | — | — |
Note
- The bold values were used to highlight the statistical differences.
- Values presented as median and interquartile range (IQR), except when indicate otherwise.
- Abbreviation: BMI, body mass index.
3.1 Discriminative validity
In the CCFT performance, the control group obtained a higher median (28 mmHg) in relation to the migraine (26 mmHg) and migraine-with-neck-pain group (26 mmHg). The CCFT showed between-groups discriminative validity only when comparing the control group with the migraine (P = .01) and migraine-with-neck-pain (P = .01) groups. Also, there were no differences between the CCFT median in migraine patients with or without migraine-related disability (verified by the MIDAS) and with or without neck pain-related disability (verified by the NDI) (Table 2).
| Groups | Median (IQR) | Mann–Whitney's U | Z score | P value | Effect size |
|---|---|---|---|---|---|
| Control (n = 51) | 28 (6) | 1233.000 | −2.759 | .01 | 0.25 |
| Migraine with neck pain (n = 68) | 26 (4) | ||||
| Control (n = 51) | 28 (6) | 1915.500 | −2.717 | .01 | 0.22 |
| Migraine (n = 102) | 26 (4) | ||||
| Without disability on MIDAS (n = 17) | 26 (6) | 582.500 | −1.290 | .20 | 0.13 |
| With disability on MIDAS (n = 85) | 26 (4) | ||||
| Without disability on NDI (n = 40) | 26 (4) | 1117.500 | −0.862 | .39 | 0.09 |
| With disability on NDI (n = 62) | 26 (4) |
Note
- The bold values were used to highlight the statistical differences
- Values presented as median and interquartile range (IQR).
- Abbreviations: MIDAS, Migraine Disability Assessment; NDI, Neck Disability Index.
3.2 Diagnostic accuracy
The diagnostic accuracy of CCFT ranged from poor to not discriminating when distinguishing control subjects from migraineurs (AUC 62.8; 95% CI 54.6; 10.4) and patients with migraine with neck pain (AUC 58.0; 95% CI 48.6; 67.0), as well as distinguishing migraine with and without disability (according to the MIDAS) (AUC 68.6; 95% CI 58.7; 77.5) and migraine with and without disability (according to the NDI) (AUC 56.86; 95% CI 46.7; 66.6). SN was low and varied from 68.6% to 74.5%, and SP ranged from 35.0% to 58.8%. There was a low diagnostic value LR+ (1.09 to 1.79) and LR− (0.50 to 0.83) for all variables.25 PPV values ranged from 62.9% to 89.6% and NPV values from 28.6% to 44.8% (Table 3).
| CCFT | Sample | Cut-off | AUC (95% CI) | Sensitivity (%) (95% CI) | Specificity (%) (95% CI) | LR+ (95% CI) | LR− (95% CI) | PPV (%) (95% CI) | NPV (%) (95% CI) |
|---|---|---|---|---|---|---|---|---|---|
| Differentiating between control and subjects with migraine | 153 | 25 | 62.8 (54.6; 70.4) | 68.6 (58.69;77.4) | 51.0 (36.6;62.2) | 1.40 (1.0;1.9) | 0.62 (0.4;0.9) | 73.7 (67.3;79.2) | 44.8 (35.4;54.6) |
| Differentiating between control and subjects with migraine and neck pain | 119 | 25 | 58.0 (48.6; 67,0) | 45.6 (33.4;58.1) | 74.5 (60.4;85.7) | 1.79 (1.0;1.0) | 0.73 (0.6;1.0) | 70.5 (58.2;80.3) | 50.7 (43.9;57.4) |
| Differentiating between migraine without (0-10 points) and with (≥11 points) disability on MIDAS | 102 | 25 | 68.6 (58.7; 77.5) | 70.6 (59.7;80.0) | 58.8 (32.9;81.5) | 1.71 (1.0;3.1) | 0.50 (0.3;0.8) | 89.6 (82.7;93.9) | 28.6 (19.3;40.1) |
| Differentiating between migraine without (0-14 points) and with (≥15 points) disability on NDI | 102 | 27 | 56.9 (46.7; 66.6) | 71.0 (58.1;81.8) | 35.0 (20.6;51.7) | 1.09 (0.8;1.4) | 0.83 (0.5;1.5) | 62.9 (56.2;69.1) | 43.8 (30.5;58.0) |
- Abbreviations: 95% CI, 95% confidence interval; AUC, area under the receiver's operational characteristic curve (value multiplied by 100); LR−, negative likelihood ratio; LR+, positive likelihood ratio; NPV, negative predictive value; PPV, positive predictive value.
Because the CCFT is a non-invasive and low-load test, there were no adverse effects resulting from the test.
4 DISCUSSION
The CCFT showed satisfactory discriminative validity to distinguish asymptomatic controls from individuals with migraine and migraine associated with neck pain. However, the CCFT does not offer a cut-off point capable of discriminating such groups, nor does it distinguish patients with migraine in relation to the presence of migraine or neck-related disability. This fair diagnosis accuracy has also been observed for patients with cervical pain.21
The performance of the CCFT between control and migraine subjects was different when the clinical stages (ranging from 22 to 30 mmHg) were considered, which not only agree with previous reports15, 16 but also establishes the between-groups discriminative validity of the CCFT. Despite the need to interpret this difference with caution given the small effect size, the CCFT can be suggested for patients with migraine to characterise better the cervical dysfunction of these patients.2
Although we assume that the CCFT can distinguish between controls and migraineurs, in our study, it was not possible to establish how much the results may be affected by the measurement error of the test due to the lack of these studies in migraine patients. Measurement error is analysed by the minimal detectable change, which consists of the variability between measurements by the same evaluator and measurements made by two different evaluators.12 For patients with neck pain, the between-groups discriminative validity of the CCFT has been previously confirmed, but the differences from controls were within the limits of the minimal detectable change (4.00 mmHg),13, 26 which implies that the positive tests may have also been false-positive.
Considering the non-discriminative validity results to distinguish between the migraine groups defined by MIDAS and NDI, migraine and neck pain-related disabilities do not seem to have a direct relationship with the performance of the motor function of the deep flexor muscles assessed by the CCFT. Likewise, Jørgensen et al8 demonstrated that the CCFT did not reflect the clinically important change in neck disability assessed by the NDI, suggesting that the CCFT does not adequately reflect the clinical situation of the neck or the evolution of the neck pain.
This study was the first to attempt to determine the cut-off for the patients with migraine and its disability-related groups. However, our data demonstrate that the CCFT does not offer a cut-off with adequate SN (46%-71%) and SP (35%-75%) to distinguish these patients. Using the CCFT score as an ordinal variable is likely what made it impossible to find this cut-off value and may contribute to its low accuracy. It presents an increase of 2 mmHg and a slight possibility of variation and change in the test (from 20 to 30 mmHg). Futures studies may verify the discriminative validity and the diagnostic accuracy of other score options such as the CCFT performance index reported by Jull et al27 through the performance index.
The current study presented the CCFT cut-off values together with a complete analysis of the accuracy of the CCFT, which is related not to the diagnosis of migraine but to the investigation of the diagnostic accuracy of the CCFT to differentiate between migraine patients with and without disabilities (according to the MIDAS or NDI) that could reflect differences resulting from musculoskeletal and cervical dysfunction. As expected, the diagnostic accuracy of the CCFT was poor to not discriminating when it came to differentiating the controls from migraine and migraine with neck pain. Also, the CCFT did not present adequate diagnostic accuracy to identify the migraine groups defined by the migraine disability on the MIDAS and neck disability on the NDI. Therefore, CCFT alone is not sufficient to clinically characterise musculoskeletal dysfunction in migraine. Thus, the worst performance of the CCFT is associated with migraine disease, regardless of the associated cervical disability.
Similarly to our results, in patients with neck pain and control subjects, Elsing et al21 found that the CCFT has a fair diagnosis accuracy (0.73; 95% CI 0.60-0.85) but was considered in conjunction with other tests as one of the most promising for clinical practice for the evaluation of the craniocervical segment.
The other CCFT accuracy measures regarding likelihood ratios and predictive values also showed low diagnostic values. According to Jørgensen et al,8 the responsiveness of clinical tests for people with neck pain presented values similar to our findings for the CCFT for LR+ (1.1), LR− (0.9), which also had LR+ > 10 e LR− < 0.1 as a reference, PPV (15.6%) and NPV (86.5). In addition, Calixtre et al28 obtained LR+ (2.69-3.33) and LR− (0.53-0.57), with reference values higher than 2 for positive LR and lower than 0.5 for negative LR, in patients with TMD associated with the presence of headache and neck pain. These values were also considered low, and the authors did not present the predictive values.28
The CCFT has already been identified as part of a cluster of six physical tests that better characterised the cervical musculoskeletal disorders in patients with migraine.15 The confirmation of the CCFT discriminative validity to distinguish patients with migraine from controls reinforces these results. However, considering the small effect size and the fair diagnosis accuracy, we suggest the CCFT be considered only a complementary tool for assessing cervical dysfunction that accompanies the clinical picture of migraine.
Moreover, it is advised to consider all the potential sources of dysfunction in the cervical spine's clinical assessment to plan the best therapeutic options.29 A complete physical evaluation of the cervical spine should be composed not only by passive components such as pain to palpation or visual observation of head and neck posture but also by active components involving function and movements.29 Future directions in the research related to assessing the cervical spine of patients with migraine should also consider other active tests, rather than CCFT, that could provide better parameters to clinicians to make their clinical decision.
4.1 Limitations
We do not know how these data would behave in a population of male patients with migraine. However, it represents the majority of the patients with migraine, as 18.9% of women are affected by the migraine, but it only occurs in 9.8% of men.30 In addition, the sample was recruited via convenience sampling. It may not have reached the appropriate sample size for migraine groups, especially migraine with headache-related disability (assessed by the MIDAS). Also, we cannot discard the potential influence of the age difference between groups. Worse performance at the CCFT was observed for healthy older adults (60-75 years old) compared to healthy young adults (18-35 years old).31 However, it is unknown whether or not the CCFT performance would be affected by a mean difference of about 3 years old in a sample composed mainly of young adults. Finally, the present analysis is restricted to a portion of all possible properties of measures that could support the use of the CCFT in migraine patients. Future studies are needed to assess aspects such as the test–retest reliability and construct validity of the CCFT in migraine patients.
5 CONCLUSION
This study confirms the discriminative validity of the CCFT in patients with migraine. However, the test did not prove to help determine the degree of migraine and neck pain-related disability. Moreover, CCFT does not present optimal cut-off value in migraine patients adequate to clinical practice.
ACKNOWLEDGMENT
Authors want to acknowledge the members of the headache center and members of the Laboratory of Posture and Human Movement, who supported our research and helped us in this clinical study of patients with migraine. We also acknowledge the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP/process 2018/21687-8) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES/ Finance Code 001) for the financial support.
DISCLOSURE
The authors declared that there is no conflict of interest.